14 Friedrich E. Kruse and Leonhard M. Holbach The available therapies for dry eye are focused mainly on augmenting or stabilizing the tear film and on reducing primary or secondary causative factors, such as inflammation of the ocular surface. Although drug treatment combined with environmental measures is the mainstream of therapy, patients with very severe dry eye disease often need surgical intervention. Surgery in the context of dry eye has primarily four objectives. The first is to reduce the rate of tear clearance and to increase the availability of existing tears by interfering with the lacrimal drainage system. This type of intervention is most commonly used to treat patients with dry eye. Among the interventions in this group are simple office procedures such as punctal plugs. Table 14-1 provides an overview of the types of interventions that have been described to increase the availability of tears on the ocular surface. The second group of surgical interventions adds additional tear-like substances to the ocular surface by using the secretory products of glands that are not normally associated with the ocular surface, such as salivary glands. Surgery by which the ocular surface is connected to reservoirs of artificial tears can also be put into this context. This type of surgery is demanding and invasive and therefore is limited to a few highly specialized centers. The procedures, which are applicable only to a small subset of patients with dry eye with unusually severe disease, are shown in Table 14-2. The third type of surgery alters the area of the ocular surface that is exposed to air, thereby reducing tear evaporation and protecting the surface, primarily by lid surgery. This type of intervention comprises procedures that reduce the inter-palpebral space and that are important measures to protect the ocular surface from desiccation. Procedures meant to enlarge the lacrimal basin are also in this group, as shown in Table 14-3.
Surgery for Dry Eye Disease
Key Points
|
|
|
The fourth type of surgery is often needed to correct disease entities that lead to secondary dry eye or that worsen dry eye conditions, such as trichiasis. These procedures are of great importance for the correction of surface abnormalities such as keratinization, conjunctivochalasis, and limbal stem cell disease. The different types of adjunct surgical procedures are shown in Table 14-4.
|
♦ Procedures to Reduce the Tear Clearance and to Increase the Availability of the Patient’s Own Tears
Reversible Obstruction of the Lacrimal Punctum or Canaliculus
Reversible obstruction of the lacrimal drainage pathway is one of the most important options for treatment of aqueous tear deficiency. Reversible obstruction can be achieved by several simple office procedures that primarily use inserts in the punctum, so-called punctal plugs.
Collagen Plugs
Collagen punctal plugs have been introduced as a measure to temporarily reduce the amount of tears collected into the canaliculi, thereby increasing both the volume of tears on the ocular surface and their availability (Fig. 14-1). Collagen plugs are made by various manufacturers, and come in different sizes commonly ranging from 1.5 to 3 mm in length and from 0.2 to 1.0 mm in diameter. For complete obstruction of the canaliculus, it is important to estimate the diameter of the opening of the lacrimal punctum and to choose the right size of the punctal plug. This can be done by use of special gauges that are inserted into the punctum. Consequently, a suitable collagen implant is chosen and inserted into the canaliculus through the punctum by use of a jeweler’s forceps. The procedure causes only slight discomfort and can be performed without anesthesia.
The effect of collagen plugs is variable and lasts from a few days to several weeks.1,2 Therefore, patients who require permanent blockage of the efferent tear system commonly need additional interventions.3 One of the advantages of punctal plugs is that they resemble the status achieved by permanent occlusion and that they can therefore be used to predict if epiphora occurs as a result of permanent blockage of the lacrimal pathway. Several authors have reported, however, that this prediction might be inaccurate because postoperative epiphora has been encountered after permanent closure although it was not present after insertion of collagen plugs.4,5
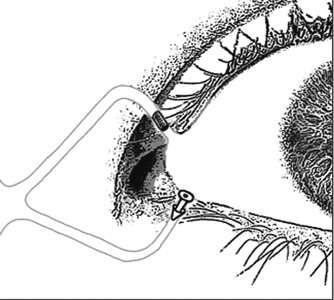
Figure 14-1 Temporary occlusion of the lacrimal punctum can be achieved by inserting collagen inserts (plugs) that last for several days to weeks. Punctal plugs are inserted in the upper part of the canaliculus and come in different materials and shapes.
The occurrence of bovine spongiform encephalopathy has caused reservations about the use of domestic bovine collagen in Europe and has resulted in the temporary discontinuation of the use of such products. However, collagen plugs are available from material originating from the Americas as well as from genetically engineered collagen. Collagen plugs are distributed by all major manufacturers that sell nonabsorbable implants (Table 14-5).
| Manufacturer | Trade Name | Description |
| Alcon Laboratories | Tears Naturale Punctal Plugs | Silicone plug, preloaded onto inserter |
| Bausch & Lomb | Punctum Plug E3990 | Silicone plug, preloaded onto inserter (diameter 0.4–0.8 mm) |
| CIBA Vision | TearSaver Plus Bio-Insulated Punctum Plugs | Silicone plug, tapered shaft (diameter 0.4–0.8 mm) |
| EagleVision | Eagle FlexPlug 3070 | Flexible, tapered shaft with indentations (diameter 0.4–1.1 mm) |
| FCI Ophthalmics | Ready-Set Punctum Plugs, Slim Line | Cap angulated (diameter 0.4–0.5 mm) |
| Ready-Set Punctum Plugs, Slanted Collarete | Slanted collarette, cap angulated (diameter 0.6–1.0 mm) | |
| PVP Perforated Plugs | Coated with PVP to enhance drainage (diameter 0.7–0.9 mm), preloaded onto inserter | |
| Lacrimedics Inc. | Herrick Lacrimal Plugs | Shaped like golf tee (diameter 0.3–0.7 mm) |
| Medennium | Smart PLUG | Temperature-sensitive polymer, changes shape upon insertion |
| Oasis Medical Inc. | Soft Plug | Absorbable collagen for medium term occlusion (1–3 months) (diameter 0.3–0.4 mm) |
| Odyssey Medical, Inc. | Parasol Punctal Occluder | Silicone plug with tail shaped like an umbrella, fit guaranteed by company |
Cellulose Implants
Other absorbable implants are less frequently used, such as inserts made from hydroxylpropyl cellulose. They melt slowly at body temperature and are dissolved within 12 hours of placement in the lower canaliculus.1 Like collagen implants, they are inserted into the canaliculus after dilation of the punctum. They are commercially manufactured and measure either 3 or 6 mm in length.6
Gelatin Implants
The use of gelatin implants is limited by the fact that they are not commercially available. They can be prepared by dissolving pure gelatin in distilled water (1 g gelatin in 1 mL water). When a cold glass rod is inserted into the gel and withdrawn, a thread of gelatin can be pulled out that is approximately 0.5 mm wide. When the thread solidifies, a small rod can be cut and inserted into the canaliculus.7 Gelatin rods usually dissolve over a period of several days to 2 weeks. Like collagen plugs, they can be used to evaluate the subjective and objective benefit of canalicular obstruction and to exclude the risks of epiphora associated with canalicular blockage.8
Nonabsorbable Punctal Plugs
Punctal plugs made from plastic or silicon were initially used by Jones et al9 for investigation of the lacrimal passage described by Freeman for therapeutic use.10 Usually, they consist of a small cylinder with a diameter of 0.3 to 1 mm. Both the head and the tail have a special configuration to provide for optimal fit in the lacrimal punctum and the upper part of the canaliculus. The tail of the plug is inserted into the canaliculus, and the head, which is often shaped like a cap, ensures a stable position within the plane of the lid margin (Fig. 14-1). Various materials and numerous sizes have been used by several manufacturers, and the design is continuously modified (for an overview of available punctal plugs, see Table 14-5).
The original silicon plugs designed by Freeman had a total length of 2.8 mm, with a spherical head of 2 mm diameter and a height of 0.7 mm. Below the head there was a neck consisting of a cylinder 1.5 mm long and 0.7 mm in diameter. The tail consisted of a triangular zone with a diameter of 1.9 mm. This device has been studied by numerous investigators.10–12 Insertion of Freeman silicone plugs in patients with aqueous tear deficiency resulted in significant decrease in tear osmolarity and ocular surface standing with rose bengal in two thirds of the patients.11 Similar results have been obtained in two other studies, one of which examined 35 patients. When both punta were treated, 75% of the patients improved, with reduced rose bengal staining and better Schirmer’s 1 test scores.12 Various modifications of the original Freeman plug have been described, such as the tapered shaft plug in which the cylindrical corpus of the plug is modified by continuously increasing its diameter toward the tail. Bernard et al have described another modification of the Freeman plug in which the head is represented by a small disk that is not perpendicular but 20 degrees oblique to the axis of the neck.13 More recently, a flexible silicone plug has been developed with a tail shaped like an umbrella, which ensures a more secure fit into the canaliculus (Parasol Punctal Occluder; Odyssey Medical Inc., Memphis, TN; Table 14-5). Another modification of the punctal plug was described by Hamano et al,14 who suggested the use of a special hydrogel polymer that changes its shape depending on the water content of its surrounding. The plug shrinks to one third of its original size when air-dried and expands to approximately 2.5 mm when it becomes moist.
Punctal occluders usually come in different sizes, and special tools are supplied for their insertion. The procedure of insertion is performed at the slit lamp either without anesthesia or after instillation of topical anesthetic drops. To ensure success of the procedure, the appropriate size of punctal plug and a suitable shape and material have to be chosen. Special calibrating tools are available for the estimation of the size of the punctum and upper canaliculus.
In about two thirds of patients, punctal plugs are well tolerated and provide for total closure of the lacrimal drainage pathway.10 In the last third, a wide range of complications occurs, including extrusion and loss of the punctal plug 10,12,15 Important factors for loss of the plug are rubbing and manipulation by the patient and overdilation of the punctum at the time of insertion.10 Irritation of the ocular surface is a potentially dangerous problem, especially in the case of corneal erosion and ulceration. These problems are explained by the normal anatomical position of the punctum close to the conjunctival epithelium and occur more frequently when plugs are inserted into the upper punctum.15,16 Lacerations and dilatation of the plug due to manipulations during insertion can also occur, and care should be exerted when dilating the punctum.10 Only rarely are plugs dislocated into the canaliculus. Canaliculitis can also occur and is one of the numerous reasons for canalicular stenosis in the context of punctal plugs.17 Canalicular stenosis seems to be more frequently caused by continuous damage of the epithelium of the canaliculus due to the punctal plug.16,17
Temperature-Sensitive Plugs for the Lacrimal Canaliculus
Anatomical differences sometimes resulting from pathological alterations of the lacrimal punctum as well as the anterior canaliculus often make it difficult to select the right size of punctal plug. This problem has led to the development of the Smart PLUG, which consists of a thermosensitive hydrophobic acrylic polymer. The ability of this polymer to change shape depending on the temperature allows the plug to alter according to the size and geometry of the canaliculus and to provide for reliable occlusion (Fig. 14-2). At room temperature and temperatures up to 32°C, the Smart PLUG (Medennium, Inc., Irvine, CA) consists of a cylinder with a diameter of 0.4 mm and a length of 9 mm. On insertion into the canaliculus, the plug is heated to 36°C, which causes significant shrinkage and a retraction. At 36°C the plaque has increased its diameter to about 1 mm and reduced its length to about 2 mm, thereby blocking the lacrimal drainage pathway. One of the advantages of this device is that insertion does not require dilation of the plaque and that it is neither visual from the outside nor does it cause irritation to the ocular surface.
Intracanalicular Silicon Plugs
To circumvent problems associated with the use of punctal plugs, a device has been described by Herrick that allows one to occlude the horizontal portion of the canaliculus.18 The Herrick Lacrimal Plug (Lacrimedics, Inc., Eastsound, WA) consists of a silicone golf tee-shaped implant that is inserted into the canaliculus with the help of a fine probe and is pushed forward to its final position in the medial part of the canaliculus (Fig. 14-2). The plug is usually well tolerated, and published studies report on experience with several hundred inserted plugs showed that less than 7% of the patients required removal of the plugs.19 Removal of the plug is necessary mainly because of undesirable epiphora and, less frequently, inflammation and dacryoliths. Removal of the plug can be achieved by probing or pressure lavage of the canaliculus. In most cases, the plug is pushed into the lacrimal sack. In rare cases, however, it has to be removed by surgical intervention, which is invasive and requires opening of the canaliculus and removal of the cul-de-sac.20
Suturing the Lacrimal Punctum
Suturing the punctum has been suggested as a temporary measure to observe the effects of obstruction of the lacrimal drainage. The procedure employs a thin monofilament suture (10-0 or 9-0 nylon or prolene) to close the punctum, an effect that lasts for about 1 week. This temporary measure allows the ophthalmologist and patient to evaluate the effect of punctal closure in respect to therapeutic benefit and the occurrence of epiphora.
Irreversible Obstruction of the Lacrimal Punctum
or Canaliculus by Application of Thermal Energy
and Laser
The application of galvanocautery, diathermy, or argon laser allows for obstruction of the lacrimal drainage pathway, although the success rate of these techniques varies. They are quick and simple office procedures that are relatively easy to perform.
Diathermy of the Lacrimal Punctum
Destruction of the lacrimal punctum by diathermy follows a principle similar to that of galvanocautery. The probe is heated by an electrical current that passes on through the body. Consequently, and in contrast to galvanocautery, a single monopolar electrode is used that produces almost no heat during operation. In principle, the procedure follows the same rules as galvanocautery and its success is determined by similar parameters.
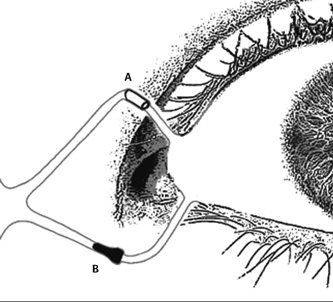
Diathermy is performed by inserting the electrode into the canaliculus (Fig. 14-3) and than activating the current for 1 or more seconds until an effect is observed. As in galvanocautery, the depth of the insertion of the probe is an important criterion for the success of the procedure. Application of diathermy to the punctum and the vertical portion of the canaliculus allows for transient obstruction of the lacrimal drainage pathway.21 Deeper insertion in the horizontal canaliculus is necessary for permanent occlution.2,21 Various techniques have been published that allow for permanent obstruction, and the parameters differ significantly depending on the device used. It is therefore important to know the specifications of the diathermy unit, which vary considerably. Dohlman used a depth of about 5 mm and gradually increased the energy until a slight discoloration and shrinkage of the skin above the probe became visible. In addition, he treated the punctum during a second application.21 Lamberts doubled the depth of the insertion to 10 mm and observed alterations of the conjunctiva above the probe. While retracting the electrode in increments of about 2 mm, he applied several cycles of treatment.2 Although several authors report higher incidences of reopening, Dohlman reported a success rate around 75%.21
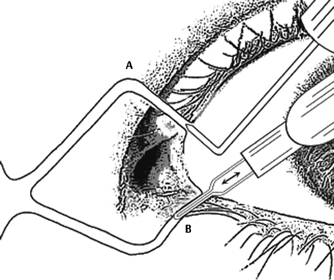
Figure 14-3 (A) Permanent, irreversible occlusion of the lacrimal punctum can be achieved by diathermy, which is performed by inserting a needle attached to a diathermy unit into the punctum. (B) Similarly, galvanocautery is performed by inserting a wired electrode that heats up when the current is applied.
Cautery of the Lacrimal Punctum
Galvanocautery is a simple method for occluding the puncta, and the instrumentation is cheap. The method has been in use for almost 60 years and represents one of the most widespread techniques used to occlude the lacrimal drainage pathway. In galvanocautery, a fine, continuous metal wire is heated by an electrical current usually originating from a battery. The degree of tissue damage depends on the duration of the application. The wire of the instrument is shaped like a flattened U, so it can be inserted into the punctum (Fig. 14-3B). A shallow regional anesthesia is applied by injecting a small amount of, for example, 2% scandicain into the vicinity of the punctum with careful observation of the anatomy. Following careful dilatation of the punctum, the cold wire is introduced into the canaliculus. Numerous suggestions have been made about the depth of the treatment. Depending on the intention, the wire can be applied to the punctum or the anterior 1 or 2 mm of the canaliculus for a temporary effect. Permanent occlusion requires treatment of the canaliculus over a length of 5 to 7 mm or the entire canaliculus up to the entrance of the sac. When the wire is inserted, the current is activated and the wire becomes hot. Coagulation is clearly visible and usually is performed for 2 to 3 seconds. The wire is withdrawn while still hot. On removal of the probe, the epithelium of the canaliculus is also removed.
Galvanocautery is not technically demanding and outcomes seem to depend on four factors: (1) relationship between the diameter of the punctum/canaliculus and diathermy probe, (2) depth of insertion, (3) duration of the heat application, and (4) speed of removal of the probe. Consequently, the results vary between immediate reopening and permanent, complete obstruction. Both healing of the thermal damage without occlusion as well as reopening, typically after a period of 2 weeks, can occur. Superficial cautery in the area of the punctum leads to reopening in every second patient.22 Reopening is reduced to about 25% when an area of 1 to 1.5 mm is cauterized.23 Deeper cauterization renders closure rates of approximately 10%.
The adverse effects of galvanocautery include mild distortion of the punctum, and dacryocystitis is reported only occasionally. In cases of postoperative epiphora, the punctum can often be opened by retrograde probing via the unoper-ated (mostly upper) canaliculus. When both canaliculi have been treated reopening is more difficult and might require a carunculo-canalicular vent as described by Murube and Murube.24
Laser Coagulation of the Lacrimal Punctum
Various lasers can be used to occlude the lacrimal punctum and most suggestions for this treatment utilize argon green. Although the thermal effect of argon lasers on the lid margins is relatively superficial, argon laser photocoagulation has been successfully used to occlude the lacrimal punctum. There are various suggestions as to how to perform this procedure, and they generally involve placing a circle of burns around the orifice of the canaliculus as well as applying burns to the center of the orifice (Fig. 14-4). Spot size for treatment of the peripheral ring varies between 10 and 200 μm, and spot sizes for the center vary between 200 and 700 μm (Table 14-6).
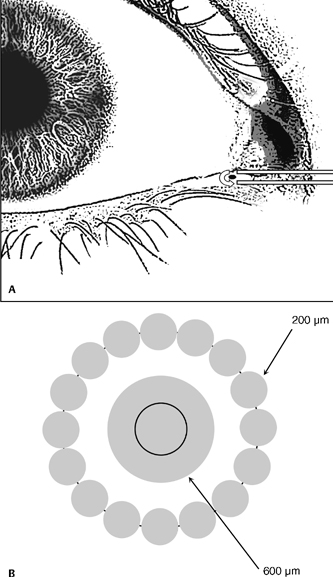
Figure 14-4 (A) Permanent, irreversible occlusion of the lacrimal punctum can be achieved by argon green laser coagulation. (B) At high magnification at the slit lamp, laser burns with a diameter of about 200 μm are placed around the punctum, whereas the center is treated with spot size of 600 μm.
Argon laser coagulation of the punctum has the advantage of simplicity and ease for the surgeon. The exact placement and the effect are controlled under high magnification with the slit lamp. The results have been reported to be sometimes unpredictable, however, and success rates vary significantly. Although some authors describe reliable occlusion and suggest retreatment in the event of reopening of the punctum, others observed a less than 15% success rate after 1 year, which is lower than reported for other methods of punctal occlusion.25–27 Reopening of the punctum following laser treatment is sometimes difficult and may require excision of the punctum and insertion of a tube or plug.
Irreversible Obstruction of the Lacrimal Punctum or Canaliculus by Glue
Permanent blockage of the lacrimal drainage pathway with acrylate glue has been described by Diamond et al.8 Canalicular occlusion is performed in topical anesthesia following dilation of the punctum. About 100 μL of N-butyl-cyanoacrylate adhesive are injected into the canaliculus via a 25-gauge cannula. Pressure is applied over the lacrimal fossa with the index finger to limit the passage of the adhesive into the lacrimal sac. In a pilot study, eight patients were treated with this method, and dacryoscintigraphy 10 to 19 months after surgery confirmed permanent occlusion.8 Cyanoacrylate glue can exert toxic effects on the epithelium of the lacrimal drainage pathway, so care is necessary in application. Some ophthalmologists use the commercially available tube in which the glue is sold and insert the tip directly into the lacrimal punctum. By pressing the tube, the material is released into the canaliculus with the inherent danger of overdosing the glue, which is avoided by using a syringe and a cannula as described earlier. A modified technique was originally described by Patten and involves dilation of the punctum as well as mechanical removal of the epithelium using a motor-driven corneal rust remover.28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree