Strabismus: Introduction
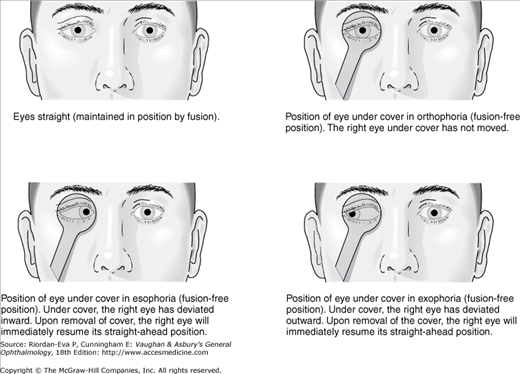
Under normal binocular viewing conditions, the image of the object of regard falls simultaneously on the fovea of each eye (bifoveal fixation) and the vertical retinal meridians are both upright. Any ocular misalignment, such that only one eye views the object of regard with the correct vertical orientation, is called “strabismus.” The misalignment may be in any direction—inward, outward, up, down, or torsional. The amount of deviation is the angle by which the deviating eye is misaligned. Strabismus present under binocular viewing conditions is manifest strabismus, heterotropia, or tropia (see Box 12.1 for definitions). A deviation present only after binocular vision has been interrupted (eg, by occlusion of one eye) is called latent strabismus, heterophoria, or phoria.
Strabismus is present in about 4% of children. Treatment should be started as soon as a diagnosis is made in order to ensure the best possible visual acuity and binocular visual function. There is no such thing as “outgrowing” childhood strabismus. Strabismus may also be acquired, due to cranial nerve palsies, orbital masses, orbital fractures, or Graves’ ophthalmopathy.
Angle Kappa: The main angle between the visual axis and the central pupillary line. When the eye is fixing a light, if the corneal reflection is centered on the pupil, the visual axis and the central pupillary line coincide and the angle kappa is zero. Ordinarily, the light reflex is 2°–4° nasal to the pupillary center, giving the appearance of slight exotropia (positive angle kappa). A negative angle kappa gives the false impression of esotropia. Conjugate movement: Movement of the eyes in the same direction at the same time. Deviation: Magnitude of ocular misalignment, usually measured in prism diopters (see later in the chapter) but sometimes measured in degrees.
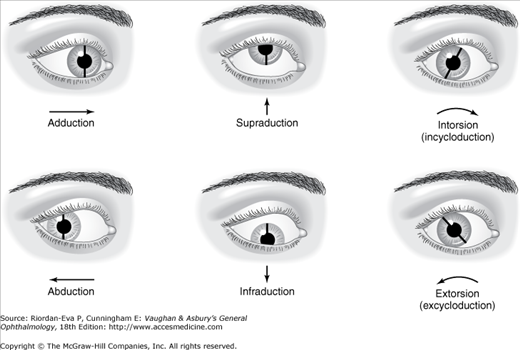
Ductions: (Figure 12–3) Monocular rotations with no consideration of the position of the other eye.
Fusion: Formation of one image from the two images seen simultaneously by the two eyes. Fusion has two aspects.
Heterophoria (phoria): Latent deviation of the eyes held straight by binocular fusion.
Heterotropia (tropia):
Orthophoria: The absence of any tendency of either eye to deviate when fusion is suspended. This state is rarely seen clinically. A small phoria is normal. Prism diopter (PD): The unit of angular measurement used to characterize ocular deviations. A 1 diopter prism deflects a ray of light toward the base of the prism by 1 cm at 1 m. One degree of arc equals approximately 1.7 PD. Secondary deviation: (Figure 12–2) The deviation measured with the paretic eye fixing and the normal eye deviating. Torsion: Rotation of the eye about its anteroposterior axis (Figure 12–3).
Vergences (disjunctive movements): Movement of the two eyes in opposite directions.
Versions: Binocular rotations of the eyes in qualitatively the same direction. |
Each of the six extraocular muscles plays a role in positioning the eye about three axes of rotation. The primary action of a muscle is the principal effect it has on eye rotation. Lesser effects are called secondary or tertiary actions. The precise action of any muscle depends on the orientation of the eye in the orbit and the influence of the orbital connective tissues, which regulates the direction of action of the extraocular muscles by acting as their functional mechanical origins (the active pulley hypothesis).
| Muscle | Primary Action | Secondary Actions |
|---|---|---|
| Lateral rectus | Abduction | None |
| Medial rectus | Adduction | None |
| Superior rectus | Elevation | Adduction, intorsion |
| Inferior rectus | Depression | Adduction, extorsion |
| Superior oblique | Intorsion | Depression, abduction |
| Inferior oblique | Extorsion | Elevation, abduction |
The medial and lateral rectus muscles adduct and abduct the eye, respectively, with little effect on elevation or torsion. The vertical rectus and oblique muscles have both vertical and torsional functions. In general terms, the vertical rectus muscles are the main elevators and depressors of the eye, and the obliques are mostly involved with torsional positioning. The vertical effect of the superior and inferior rectus muscles is greater when the eye is abducted. The vertical effect of the obliques is greater when the eye is adducted.
The position of the eye is determined by the equilibrium achieved by the pull of all six extraocular muscles. The eyes are in the primary position of gaze when they are looking straight ahead with the head and body erect. To move the eye into another direction of gaze, the agonist muscle contracts to pull the eye in that direction and the antagonist muscle relaxes. The field of action of a muscle is the direction of gaze in which that muscle exerts its greatest contraction force as an agonist, for example, the lateral rectus muscle undergoes the greatest contraction in abducting the eye (Table 12–1).
Synergistic muscles are those that have the same field of action. Thus, for vertical gaze, the superior rectus and inferior oblique muscles are synergists in moving the eye upward. Muscles synergistic for one function may be antagonistic for another. For example, the superior rectus and inferior oblique muscles are antagonists for torsion, the superior rectus causing intorsion and the inferior oblique extorsion. The extraocular muscles, like skeletal muscles, show reciprocal innervation of antagonistic muscles (Sherrington’s law). Thus, in dextroversion (right gaze), the right medial and left lateral rectus muscles are inhibited while the right lateral and left medial rectus muscles are stimulated.
For movements of both eyes in the same direction, the corresponding agonist muscles receive equal innervation (Hering’s law). The pair of agonist muscles with the same primary action is called a yoke pair. The right lateral rectus and the left medial rectus muscles are a yoke pair for right gaze. The right inferior rectus and the left superior oblique muscles are a yoke pair for gaze downward and to the right. Table 12–2 lists the yoke muscle combinations.
Motor fusion is the process by which the activity of the extraocular muscles is adjusted to maintain the necessary ocular alignment for sensory fusion (see later in the chapter). It is stimulated by disparity in images received from the two eyes, such as results from the object of regard moving toward or away from the subject.
The neuromuscular system of an infant is immature, so that it is not uncommon in the first few months of life for ocular alignment to be unstable. Transient exodeviations are most common and are associated with immaturity of the accommodation-convergence system. Gradually improving visual acuity together with maturation of the ocular motor system allows a more stable ocular alignment by age 2 to 3 months. Any ocular misalignment after this age should be investigated by an ophthalmologist.
Binocular vision, the ability to combine the visual information from two eyes viewing the same scene into a single image, provides several advantages, not least the potential for three-dimensional vision (stereopsis). The corresponding disadvantage is that the process is dependent upon maintenance of ocular alignment.
The retinal locations upon which fall the images of a single object in the two eyes are known as corresponding retinal points. Since the two eyes are not in precisely the same location, the images on these retinal points are not exactly the same. Sensory fusion is the process whereby disparities between the two images at corresponding retinal points are overcome to allow a single image to be perceived. In reality there is not absolute correspondence between the retinal points that can be stimulated to produce a single image. Each point of the retina in each eye is capable of fusing stimuli that strike sufficiently close to the corresponding retinal point in the other eye. The representation in space of this region of fusible points is called Panum’s area. It is narrowest at fixation and progressively increases in size with increasing eccentricity in the visual field. Sensory fusion is also dependent upon the images in the two eyes being sufficiently similar, equality of size being a particularly important factor.
In contradistinction to sensory fusion, stereopsis relies upon recognition of the disparities of images that are being fused, effectively utilizing parallax. It is quantified as the smallest detectable disparity, around 60 seconds of arc being high-grade (fine) stereopsis, which is only possible with bifoveal fixation, and around 1000 seconds of arc being low-grade (gross) stereopsis. Although stereopsis is essential for high-grade depth perception, monocular clues such as apparent size of objects, interposition of objects, and motion parallax can be used to judge depth.
Strabismus is associated with various sensory phenomena, including diplopia and visual confusion, abnormal (anomalous) retinal correspondence, suppression, amblyopia, and eccentric fixation. The occurrence of these phenomena is related to whether the strabismus is present during the development of the visual system, which occurs up to age 7 or 8.
In the presence of strabismus, each fovea receives a different image. The image of the object of regard falls on the fovea of the fixing eye and the object is localized straight ahead, whereas the same image falls on an extrafoveal retinal area in the deviating eye and the object is localized in some other direction, so that the object of regard is perceived to be in two places (diplopia), with a true image from the fixing eye and a false image from the deviating eye. Correspondingly, the object responsible for the image falling on the fovea of the deviating eye is localized straight ahead, so that it and the object of regard are perceived to be in the same place (visual confusion). Whereas diplopia is common in acquired strabismus, awareness of visual confusion is unusual.
In the presence of manifest strabismus, an extrafoveal retinal locus may become the preferred point of fixation in the deviating eye, resulting in abnormal (anomalous) retinal correspondence (ARC). There may be exact correlation between the position of this locus and the angle of strabismus (harmonious ARC or ARC with identity) or not (unharmonious ARC or ARC without identity). ARC is present only under binocular viewing conditions, in contrast to eccentric fixation (see below). ARC avoids diplopia and visual confusion because the extrafoveal retinal locus of fixation in the deviating eye is localized straight ahead during binocular viewing. It also facilitates binocular function, possibly resulting in low-grade stereopsis.
Suppression is a common sensory adaptation in childhood strabismus, avoiding diplopia and visual confusion and, also like ARC, being present only under binocular viewing conditions. The image seen by one eye predominates and that seen by the other eye is suppressed due to the presence in the deviating eye of an area of reduced visual sensitivity within the visual field. This suppression scotoma is termed a facultative scotoma because it is not present when the suppressing eye is tested alone, contrasting with amblyopia (see below), which persist when the affected eye is tested alone.
In esotropia, the suppression scotoma is usually approximately horizontally elliptical in shape, extending on the retina from just temporal to the fovea to the point in the nasal extrafoveal retina on which the image of the object of regard falls. In exotropia, the suppression scotoma tends to be larger, usually extending from the fovea to include the entire temporal half of the retina. If there is alternating fixation, the suppression scotoma is present in whichever eye is deviating. Suppression precludes high-grade stereopsis because of the lack of bifoveal fixation, but low-grade stereopsis may still be present due to ARC (see earlier in the chapter). In the absence of strabismus, a blurred image (usually due to anisometropia) in one eye may also lead to suppression.
Prolonged abnormal visual experience in a child under the age of 7 years may lead to amblyopia (reduced visual acuity in excess of that explicable by organic disease). The three main causes of amblyopia are strabismus, unequal refractive error (anisometropia), and visual deprivation (eg, congenital cataract, ptosis or optic nerve hypoplasia). Often, more than one etiology is present. Though previously thought to be untreatable after 7 years of age, recent studies show that some forms of amblyopia may be successfully treated in older children.
In strabismus, the eye used habitually for fixation retains normal acuity whereas acuity is persistently reduced in the nonpreferred eye. In esotropia, amblyopia is common and often severe, whereas in exotropia it is uncommon and usually mild. If spontaneous alternation of fixation is present, amblyopia does not develop.
In eyes with severe amblyopia, an extrafoveal retinal area may be used for fixation even under monocular viewing conditions, in contrast to ARC (see earlier in the chapter) when the phenomenon only occurs under binocular viewing conditions. Gross eccentric fixation can be readily identified by occluding the preferred eye and asking the patient to look directly at a light source with the nonpreferred eye. An eye with gross eccentric fixation will appear not to be looking directly at the light source and will have an eccentric corneal light reflection. More subtle degrees of eccentric fixation can be detected by an ophthalmoscope that projects a target, the patient being asked to look directly at its center. If the target is projected onto any area other than the fovea, eccentric fixation is present.
A careful history is important in the diagnosis of strabismus.
- Laterality. Does the deviation only occur in one eye or does it alternate?
- Direction. Is the deviation inward, outward, upward, or downward?
- Duration. When was the deviation first noticed? Was the onset gradual or sudden?
- Frequency. Is the deviation constant or intermittent? If intermittent, how often does it occur? Has the frequency increased, decreased, or remained the same since it was first noticed?
- Modifying factors. Is the deviation worse with fatigue, illness, or alcohol use?
- Associated symptoms. Is there diplopia, asthenopia (eyestrain), visual confusion, or headache?
- Past ocular history—including any history of spectacle wear, ocular trauma, or surgery.
- Past medical history—including any history of prematurity, developmental delay, neurological disorder, or thyroid disease.
- Family history—including any history of strabismus, “squint,” “cast”, amblyopia, “lazy eye,” or other ocular disease in the family?
Visual acuity should be evaluated even if only a rough approximation or comparison of the two eyes is possible. Each eye is evaluated by itself, since binocular testing will not reveal poor vision in one eye. For the very young child, it may only be possible to establish that an eye is able to follow a moving target. The target should be as small as the child’s age, interest, and level of alertness allow. Fixation is described as being normal if it is central (foveal) and steady, and maintained while the eye follows a moving object. In a preverbal child with manifest strabismus, a fixation preference for one eye implies amblyopia of the fellow eye. In a preverbal child without obvious manifest strabismus, fixation preference can be tested by holding a 15 prism diopter (PD) (see Box 12.1) vertical prism before each eye to induce a vertical disparity in images (induced tropia test). Placing the prism in front of an eye that was fixing will induce a compensatory vertical movement in both eyes, without any refixational movement if the same eye continues to fix or a refixational movement of both eyes if the fellow takes over fixation. Placing the prism in front of an eye that was not fixing will not result in any movement of either eye. Another technique for quantitatively measuring visual acuity in younger children is forced-choice preferential looking, in which the child’s responses are observed to simultaneous presentation of striped gratings of a range of frequencies and an otherwise identical shaped but plain target of the same mean luminance. Threshold of detection (grating acuity) is determined by the highest frequency (cycles per second) of grating that results in consistent preferential looking by the child. It is usually better than recognition acuity, particularly in amblyopic eyes.
By the age of 2½–3 years, it is possible to perform recognition visual acuity testing using Allen pictures. By age 4 years, many children will understand the Snellen tumbling “E” game or the HOTV recognition test. HOTV testing is generally preferred, the tumbling “E” game being prone to reversal errors in young children. By age 5 or 6 years, most children can perform Snellen visual acuity testing. At this age, single optotype Snellen acuity has normally developed fully, but Snellen acuity to a line of multiple optotypes (linear acuity) may not develop fully for another 2 years. In this situation, crowded optotypes may be used to simulate linear acuity test.
It is important to determine the cycloplegic refractive error by retinoscopy (see Chapter 21). Cycloplegic refraction is most often performed utilizing cyclopentolate 1% ophthalmic solution. Occasionally, atropine 1% solution or ointment is used to ensure complete cycloplegia, or in children with dark irides that do not cycloplege well in response to weaker agents.
Inspection alone may show whether strabismus is constant or intermittent, alternating or nonalternating, and whether it is variable. Associated ptosis and abnormal position of the head should be noted. The quality of fixation of each eye separately and of both eyes together should be assessed. Nystagmus indicates unstable fixation and usually reduced visual acuity.
Prominent epicanthal folds that obscure all or part of the nasal sclera may give an appearance of esotropia (pseudostrabismus). Although this entity is confusing to lay persons as well as some physicians, these children have a normal corneal light reflection test. Prominent epicanthal folds gradually disappear by 4 or 5 years of age.
Ocular examination is essential to ensure that strabismus or reduced vision is not due to structural abnormalities. In children esotropia may be the presenting feature of various diseases, including congenital anomalies such as optic nerve hypoplasia, retinoblastoma, and optic nerve glioma.
All four components of cover testing, (1) the cover test, (2) the uncover test, (3) the alternate cover test, and (4) the prism and alternate cover test, require fixation of a target, which may be in any direction of gaze at distance or near.
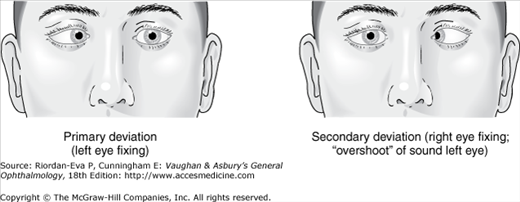
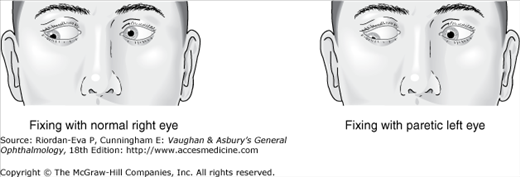
The cover test identifies manifest strabismus. As the examiner observes one eye, a cover is placed in front of the fellow eye to block its view of the target. If the observed eye moves to take up fixation, it was not previously fixing the target, and a manifest strabismus is present. The direction of movement reveals the direction of deviation (eg, if the observed eye moves outwards to pick up fixation esotropia is present). The cover test is performed on each eye. Childhood strabismus is usually comitant, meaning that the magnitude of the manifest strabismus is not significantly influenced by which eye is fixing, or the direction of gaze. Cranial nerve palsies (paretic strabismus), except when longstanding, and other types of acquired strabismus are usually incomitant, the magnitude of the manifest strabismus being less when the unaffected eye is fixing (primary deviation) than when the affected eye is fixing (secondary deviation) (Figure 12–2), and varying with direction of gaze (see Box 12.1).
The uncover test provides information on fixation preference if there is manifest strabismus, or identifies latent strabismus if there is no manifest strabismus. As the cover is removed from the eye following the cover test, the eye emerging from under cover is observed. If the position of the uncovered eye changes, either a manifest strabismus is present and the uncovered eye is once again taking up fixation, indicating that it is the preferred eye, or interruption of binocular vision has allowed it to deviate, and a latent strabismus is present. In either case, the direction of corrective movement indicates the type of manifest or latent strabismus, with the same pattern as in the cover test (eg, outwards in esotropia or esophoria). In manifest strabismus also there will be a movement of the fellow eye but in the opposite direction (eg, inwards in esotropia). In latent strabismus there will be no movement of the fellow eye. If the uncover test results in no movement of the uncovered eye, either a manifest strabismus is present but the fellow eye has maintained fixation, indicating alternating fixation, or there is no manifest or latent strabismus (orthophoria), which is rarely seen clinically. The uncover test is also performed on each eye.
The alternate cover (cross-cover) test reveals the total deviation (manifest plus latent strabismus). The cover is placed alternately in front of one eye and then the other. It should be moved rapidly from one eye to the other to prevent re-fusion of a latent strabismus.
The prism and alternate cover test quantifies strabismus. Increasing strength of prism is placed in front of one eye until there is neutralization of the movement on alternate cover testing, thus measuring both the manifest and latent components. For example, to measure the full extent of an esodeviation, the cover is alternated while prisms of increasing base-out strength are placed in front of one eye until there is no horizontal refixational movement of the deviated eye. More than the required strength of prism will result in reversal of direction of the refixational movement. Larger deviations may require prisms held before both eyes, but prisms should never be “stacked” in the same direction before one eye.
Figure 12-2.
Paresis of horizontal muscle (right lateral rectus). Secondary deviation is greater than primary deviation because of Hering’s law. With the left eye fixing, the right eye is deviated inward because of the paretic right lateral rectus. For the right eye to fix, the paretic right lateral rectus muscle must receive excessive stimulation. The yoke muscle—the left medial rectus—also receives the same excessive stimulation (Hering’s law), which causes “overshoot.”
The various types of cover test require patient cooperation and some degree of useful vision in both eyes. Two other methods commonly used depend on observing the position of the corneal light reflection, but both are less accurate than cover tests and their results must be adjusted if the angle kappa is abnormal (see Box 12.1).
Hirschberg method. The patient fixes on a light at a distance of about 33 cm. Decentration of the light reflection is noted in the deviating eye. By allowing 18 PD for each millimeter of decentration, an estimate of the angle of deviation can be made.
Prism reflex method (Krimsky test). The patient fixes on light at a distance of about 33 cm. A prism is placed before the deviating eye, and the strength of the prism required to center the corneal reflection measures the angle of deviation.
With one eye covered, the other eye follows a moving target in all directions of gaze. Any decrease of rotation indicates limitation in the field of action of the respective muscle due to weakness of contraction or failure of relaxation of its antagonist.
Hering’s law states that yoke muscles receive equal stimulation during any conjugate ocular movement. Versions are tested by having the eyes fix a light in the nine cardinal positions: primary—straight ahead; secondary—right, left, up, and down; and tertiary—up and right, down and right, up and left, and down and left (Table 12–2). Difference in rotation of one eye relative to the other is noted as underaction or overaction. By convention, in the tertiary positions, the oblique muscles are said to be underacting or overacting with respect to the yoke rectus muscle. Fixation by the normal eye in the field of action of a paretic muscle results in underaction of the paretic muscle. Conversely, fixation with the eye with the paretic muscle will lead to overaction of the yoke muscle, since greater innervation is required for contraction of the underacting muscle (Figure 12–4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree