OVERVIEW
- SRBD is a spectrum of conditions ranging from simple snoring to severe OSAHS that develops with increasing reduction in airflow and has a major impact on patient life (socially and medically)
- A major risk factor is obesity and effective strategies to achieve long-term weight loss are desperately needed to curtail the concurrent epidemics of obesity and obstructive sleep apnoea
- The gold standard for diagnosis is polysomnography but this is not always available and other sleep studies are used in conjunction with a detail history (with the patient’s partner)and thorough examination
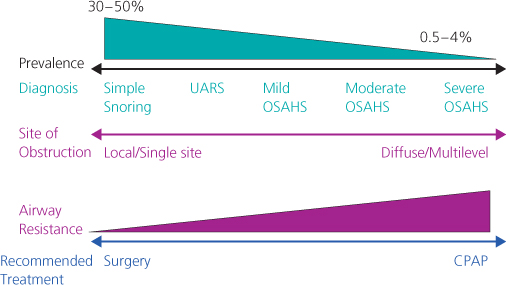
- Treatment of the SRBD depends on its severity and ranges from lifestyle changes and simple surgery amongst simple snorers to mild OSAHS patients whilst patients with moderate to severe OSAHS benefiting from CPAP
- SRBD is common in children and the most common treatment choice for paediatric OSAHS is adenotonsillectomy
Snoring and obstructive sleep apnoea syndrome (OSAHS) are different degrees of a broadly identified disorder; sleep-related breathing disorder (SRBD). Identifying SRBDs is important as they have a major impact on a patient’s life. The medical implications of SRBDs such as increased risk of stroke, hypertension and other cardiovascular conditions such as arrhythmias and myocardial ischaemia are well-documented. Daytime somnolence poses a risk to the individual and public with respect to road traffic accidents. Lastly, marital and relationship disharmony can occur as a consequence of simple snoring; significant improvement in the quality of life is achieved with successful surgery.
Spectrum of the condition
SRBD results from partial or total obstruction of the upper airway. The pathogenesis is multifactorial; reduced muscle tone during sleep and certain anatomical variations in the upper airway predisposing to the condition. Increasing upper airway resistance results in progressive worsening of the disease. SRBD is a spectrum of conditions (Figure 19.1) ranging from simple snoring to severe OSAHS that develops with increasing reduction in airflow.
Figure 19.1 The continuum of sleep-disordered breathing. UARS, upper airway resistance syndrome; OSA, obstructive sleep apnoea; OSAHS, obstructive sleep apnoea hypopnea syndrome.
Depending on the degree of obstruction and associated symptoms, individuals are categorised into one of the following categories:
Progression of airway collapse and obstruction leads to either complete with total cessation of airflow (apnoea) or partial with significant hypoventilation (hypopnoea). Severity of OSAHS is determined by frequency of the apnoeas and hypopnoea called the apnoea/hypopnoea index (AHI) (Table 19.1).
Table 19.1 Categories of severity of OSAHS.
| Severity of OSAHS | AHI (apnoea/hypopnoea events per hour) |
| Mild | 5–14 |
| Moderate | 15–30 |
| Severe | greater than 30 |
Clinically significant OSAHS is only likely to be present when the AHI is greater than 15 events per hour in association with unexplained EDS.
Aetiology
The airway between the posterior end of the nose and the larynx is unprotected by cartilaginous or bony structures and reliant on muscle tone for its patency. SRBD only occurs during sleep when pharyngeal muscle tone falls progressively as sleep condenses to deeper levels. This phenomenon is present in all humans and yet not all humans have SRBD. Abnormalities in both “upper airway” size and muscle activity appear to contribute to its pathogenesis.
Factors found to increase the risk of SRBD are:
Table 19.2 Other associated risk factors of OSAHS.
| Risk factor | Associations | Salient points |
| Age | Progressive increase in prevalence of SRBD in 6-7th decades | Narrower and possibly more collapsible upper airways seen with increasing age |
| Hereditary | Two- to fourfold greater | In first degree relatives |
| Medical history | Hypothyroidism Acromegaly Neuromuscular diseases Chronic lung disease* (*not a direct risk for SRBD) | Due to craniofacial anomaly Central apnoeas are more likely OSAHS is more severe with deeper events de-saturation due to hypo-ventilation and lower lung reserve |
| Social history | Smoking Alcohol | |
| Drugs | Hypnotics Opioids | Central depression increase the risk of SRBD |
Consequences of sleep-related breathing disorders
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


