(1)
Narayana Hridayalaya Multispeciality, Bangalore, India
Surgical Anatomy
The treatment of cranial base tumors is very challenging due to the complex anatomy of the region and its relation to important structures like the brain, eye, and cranial nerves. The space is limited at skull base and proper understanding of anatomy and extent of disease spread forms basis for skull base surgery. It is important to achieve three-dimensional clear margins even for skull base tumors, and a variety of surgical approaches have been described to achieve that. It is advisable to combine trans-facial approach with transcranial approach to have adequate exposure for three-dimensional clearance tumor.
Figure 12.1 shows schematic anatomy of the anterior skull base. The skull base bone forms dividing line between the cranial and facial sections. The dura and brain form a cranial component while nose and PNS with the eye forms the facial component. The cranial nerves and vessels passing through various foramina provide channels for communication between the two compartments, and the tumor can pass through any of these channels to adjacent area.


Fig. 12.1
Schematic diagram of skull base anatomy
The cranial base area can be divided into five sections for ease of discussion:
1.
Anterior cranial base
2.
Anterolateral cranial base
3.
Lateral cranial base
4.
Central cranial base
5.
Posterior cranial base
The central and posterior cranial base tumors are mainly addressed by neurosurgeons and are beyond the scope of this book. The remaining areas are discussed in this chapter in detail.
Surgical Pathology
The tumors at the skull base mostly arise from adjacent structures and wide variety of lesions can be encountered in this region. This can range from benign tumors to aggressive malignant lesions, and establishing tissue diagnosis is essential to plan appropriate treatment. The IHC studies are often helpful to establish the final diagnosis. Imaging studies help in identifying the structure of origin and its relation to the surrounding areas, and this can add in achieving the final diagnosis.
Figure 12.2 is a schematic representation of various skull base areas and its relation to areas from where the tumor spread. Anterior cranial base is the most frequently involved skull base area, and tumors arising from the nose and paranasal sinuses are the main culprits. The lesions arising from nose and maxilla traverse the ethmoid sinus and involve cribriform plate and dura. The olfactory neuroblastoma, minor salivary gland neoplasms, and various other neoplasms are also not uncommon in this area. The anterolateral cranial base is associated with masticator space and ITF. The tumor can spread to middle cranial fossa from ITF and requires combined approaches to achieve complete clearance. The tumors arising from the oral cavity and posterior maxilla are more inclined to spread in this area. The lateral cranial base is associated with tumors arising from the ear and temporal bone. These tumors are addressed by lateral temporal bone approaches. The author doesn’t have enough experience to treat these tumors. It is a specialized area and is ideal to refer a book on temporal bone resection.
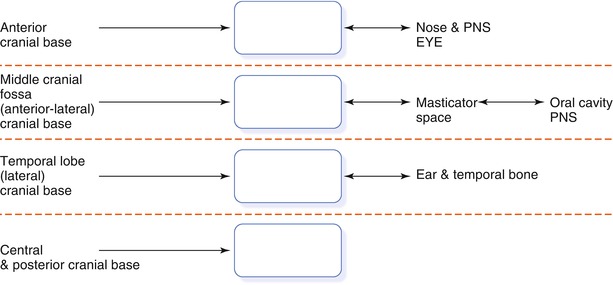
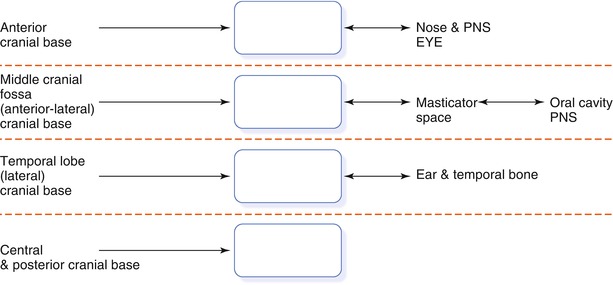
Fig. 12.2
Relations of cranial base to surrounding structures and pattern of spread
Surgical Concepts
Figure 12.3 demonstrates the concept of combined craniofacial resection (CFR). The skull base area has limited space and is associated with vital structures. The combination of transcranial approach with trans-facial approach allows better exposure to tumor from above. This helps in identifying and preserving important structures while removing the tumor in en bloc fashion.
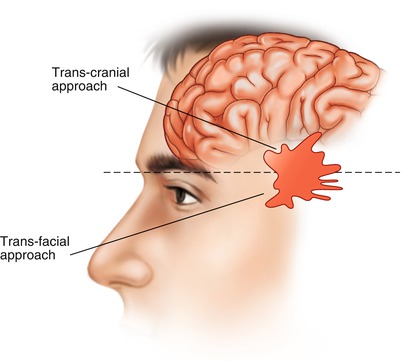
Fig. 12.3
Concept for combined CFR
Involvement of the brain and carotid artery by a tumour is generally considered sign of inoperability. The lesion can be resected if it involves a limited portion of the brain. The long-term outcome is equivocal for such group of patients.
Involvement of the dura and skull base bone in certain areas is considered operable provided it is possible to achieve negative margins. There is hardly any role of incomplete removal of tumor or debridement in skull base surgery.
It is difficult to achieve 1 cm disease-free margin at the skull base. The decision to sacrifice or preserve a vital structure for disease clearance is difficult in many cases. It is acceptable to preserve the structure when there is a clear tissue plane between the disease and the structure.
Minimal invasive approaches (endoscopic skull base approach) have become popular in recent times. In order to be a good endoscopic skull base surgeon. One needs to have adequate experience in open as well as endoscopic surgery for skull base tumors. First attempt is the best attempt and no compromise on oncological clearance should be done to improve cosmetic outcome.
Reconstructive strategy is essential for each skull base surgery, and appropriate repair of the dural defect influences the postoperative morbidity and mortality.
These procedures are best performed in an institution with a backup team to manage unexpected complications.
Surgical Approaches
The craniofacial resection is performed by combination of trans-facial and transcranial approaches to remove skull base tumor. These approaches are used based on areas of the skull base involved by the tumor.
1.
Anterior skull base:
Trans-facial approach – lateral rhinotomy, midfacial degloving, Weber–Ferguson, and endoscopic approach
Transcranial approach – bi-coronal flap with frontal craniotomy, subcranial approach (Rave’s approach)
2.
Anterolateral skull base:
Trans-facial approach – transmandibular approach, facial translocation approach, pre-auricular trans-zygomatic approach, post-auricular temporal approach
Transcranial approach – frontotemporal craniotomy
3.
Lateral skull base:
Lateral temporal bone resection, subtotal temporal bone resection, and total temporal bone resection
Anterior Craniofacial Resection
This procedure is required for nose and PNS tumors involving the anterior skull base (cribriform plate, dura). The transcranial part can be performed either by conventional frontal craniotomy approach or by subcranial approach. The conventional approach is preferred for large tumors that involve the dura and brain. This approach requires brain retraction and may cause edema in postoperative period. The subcranial approach is preferred for limited lesions that extend up to the dura. It is preferred to have a large frontal sinus to perform this limited approach. It requires minimal brain retraction resulting in less postoperative morbidity. Tumor removal is rarely a problem with subcranial approach, but dura repair is challenging particularly for tumors with large posterior spread reaching up to the sphenoid sinus.
This section demonstrates two operative procedures describing technical details for conventional and subcranial approaches.
Conventional Anterior CFR
The patient has nasal mass with anterior skull base extension infiltrating dura.







 < div class='tao-gold-member'>
< div class='tao-gold-member'>





Fig. 12.4
Bi-coronal incision for raising the flap

Fig. 12.5
The posterior flap is raised beyond and posteriorly to get added length for pericranial flap that can help in sealing the dural defect
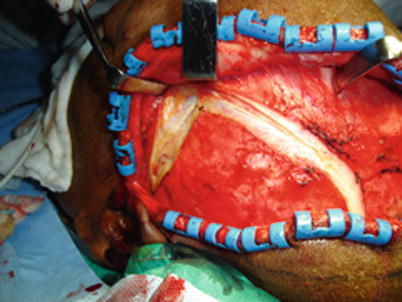
Fig. 12.6
On the lateral aspect, care is taken to avoid injury to frontal branch of facial nerve. The incision is placed on temporalis fascia and further dissection is carried out in a deeper plane

Fig. 12.7
The peri-cranial flap is raised and isolated from the skin flap. It is important to avoid button holes while raising this flap. The vascularized flap can be used for patching the dural defect

Fig. 12.8
The frontal craniotomy is performed
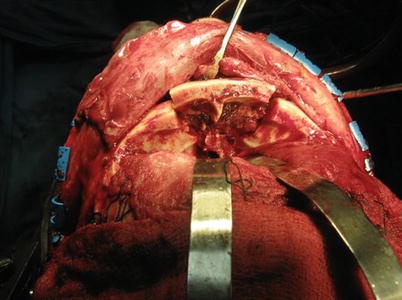
Fig. 12.9
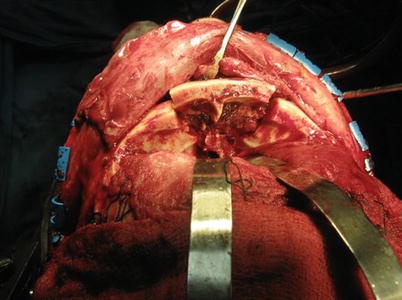
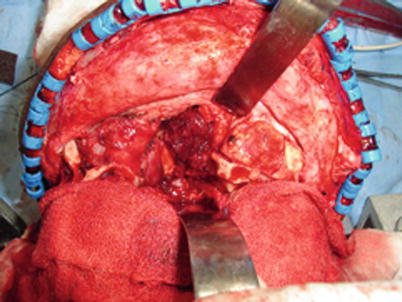
The brain is retracted to expose anterior skull base. The dura is separated gradually from skull base bone and olfactory tracks are clamped and cut to isolate cranial cavity from the tumor. If the tumor is involving the dura, the dura is resected with adequate margins
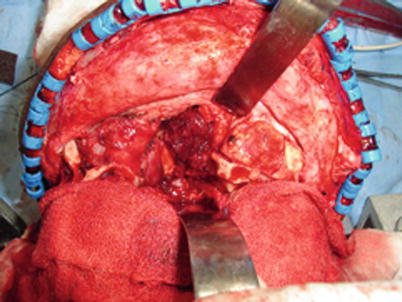
Fig. 12.10
The tumor is separated from all around. The skull base bone is cut from one side of orbital wall to another side of orbital wall and from the frontal sinus to anterior wall of the sphenoid sinus. This manoeveur pushes the tumor and skull base down and exposes the frontal and sphenoid sinuses

Fig. 12.11
The lateral rhinotomy approach is planned for this case

Fig. 12.12
The flaps are being raised

Fig. 12.13
Medial wall of the maxilla with lateral nasal wall is exposed

Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


