8 Secondary Glaucoma
PRETRABECULAR OUTFLOW OBSTRUCTION
SECONDARY ANGLE CLOSURE WITH PUPIL BLOCK
Possible reasons for pupil block are:
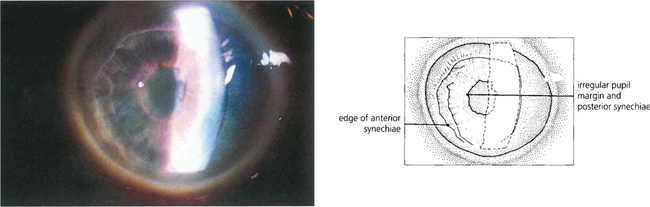
1. Posterior synechiae from inflammation in the anterior segment
2. Occlusion of the pupil in pseudophakic and aphakic eyes by the implant or vitreous gel
Inflammation in the anterior segment
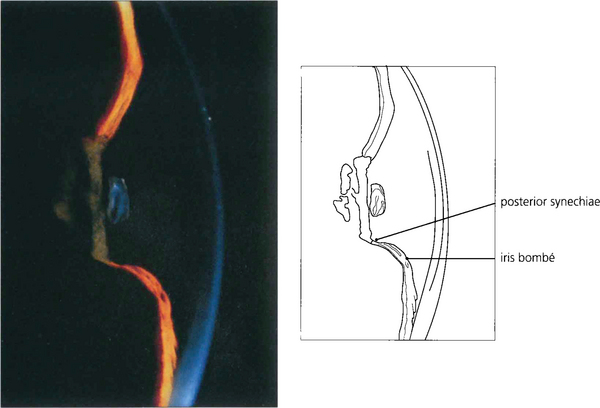
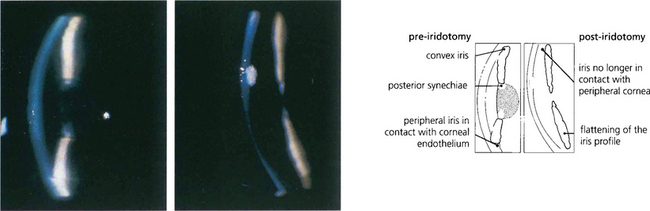
Fig. 8.1 In this patient with uveitis pupil block due to seclusion of the pupil is evident from the forward convexity of the iris resulting in a shallow peripheral anterior chamber, whereas the central chamber remains deep. The deep central anterior chamber distinguishes pupil block from malignant glaucoma with forward movement of the iris–lens diaphragm secondary to posterior segment pathology or pupil block from intumescent cataract.
Pupil block in pseudophakic and aphakic eyes
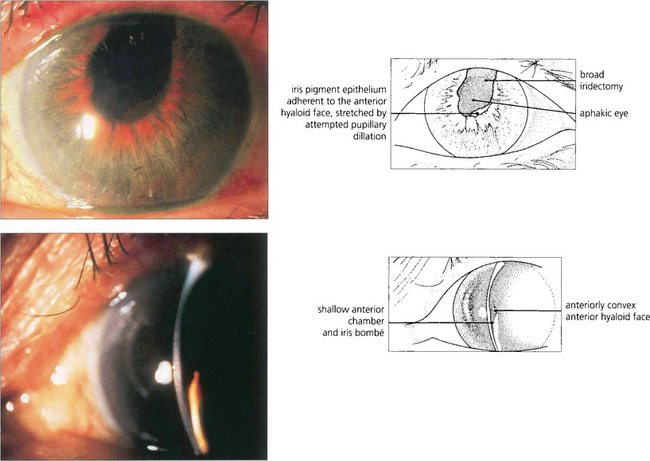
Fig. 8.3 In this patient there is pupil block from posterior synechiae to the vitreous face in an aphakic eye. The slit-lamp image shows peripheral shallowing of the anterior chamber. The extent to which the gel prolapses into the anterior chamber determines the central depth.
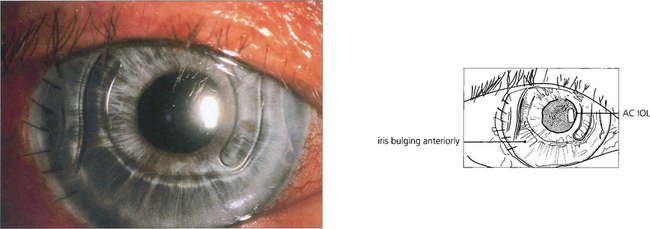
Fig. 8.4 Anterior chamber intraocular lens implantation without peripheral iridectomy is likely to cause pupil block. In this case the iris can be seen bulging forwards around the implant. Although the angle can often be reopened by a laser iridotomy this readily reoccludes with vitreous and so does not reliably prevent recurrence. Surgical iridectomy is definitive but difficult to achieve through a corneal phacoemulsification wound unless it is placed temporally. Temporal iridectomies may cause glare or monocular diplopia, however, and so surgical entry by a separate superior corneal incision is preferable.
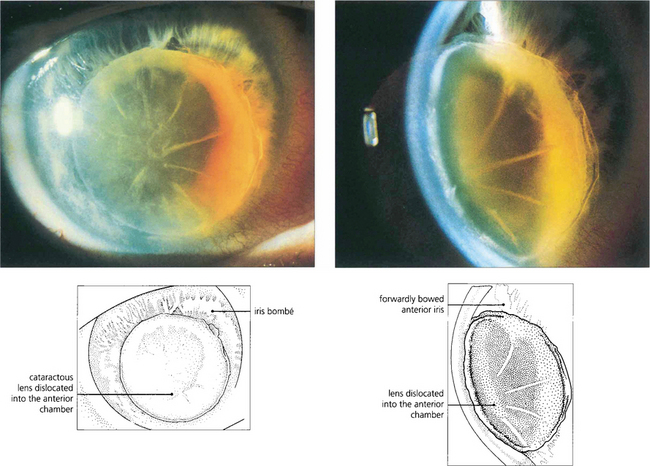
Forward movement of the anterior lens surface
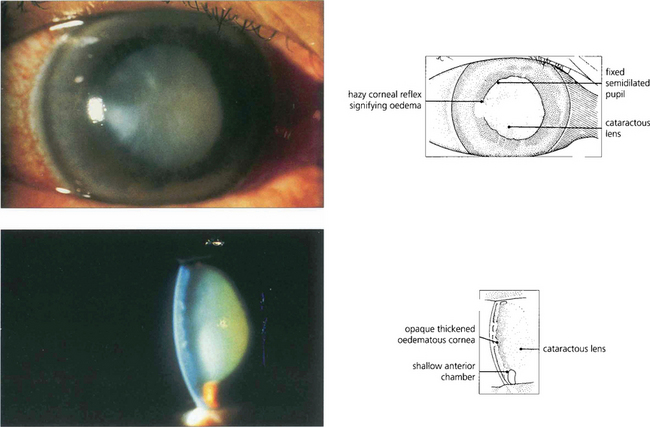
Fig. 8.6 Acute angle closure due to an intumescent cataractous lens. The eye is red with a hazy view of the anterior segment from corneal oedema, with a fixed irregular semidilated pupil from iris infarction. The slit image shows the corneal oedema and a very shallow anterior chamber. Some uveitis may be present because of ischaemia, and this must be differentiated from the larger accumulations of lens material and macrophages seen with phacolytic glaucoma (see Fig. 8.49).
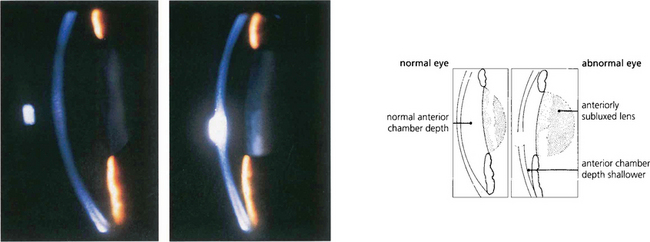
Fig. 8.7 Slit-image photography of the left and right eye of this patient demonstrates a subluxed lens in the left eye. The anterior chamber is shallow and further examination shows that the anterior lens surface is closer to the posterior corneal surface inferiorly than superiorly occluding the pupil and producing pupillary block.
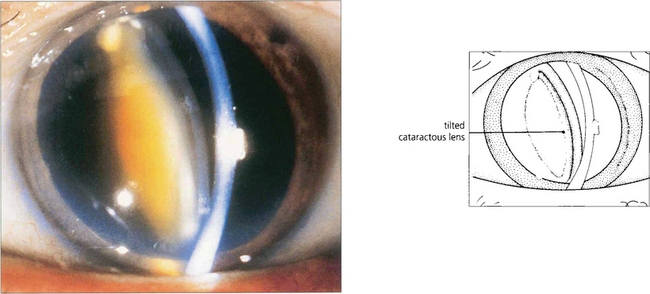
Fig. 8.8 Occasionally pupillary dilatation allows a subluxed lens to swing into the pupillary plane and block communication between the posterior and anterior chamber. Careful positioning of the patient and the use of miotics usually allow the lens to be repositioned safely until definitive treatment can be arranged which in this case is removal of the lens.
SECONDARY ANGLE CLOSURE WITHOUT PUPIL BLOCK
Angle closure may occur without pupil block in four ways:
1. Changes in the posterior segment that push the lens–iris diaphragm forwards
2. Changes in the anterior segment that result in loss of the anterior chamber and iris–trabecular contact with synechial closure
4. Cellular proliferation within the angle of the anterior chamber resulting in iris–trabecular adhesions.
Angle closure from changes in the posterior segment
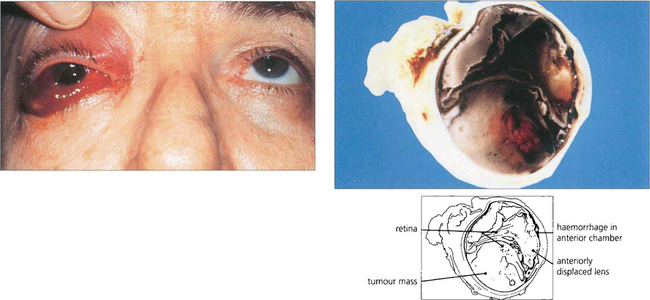
Fig. 8.10 A patient with a long-standing blind eye presented with recent onset of pain, conjunctival oedema and anterior chamber haemorrhage. Posterior segment ultrasonographic examination showed a large choroidal melanoma. Hemisection of the enucleated eye demonstrates a large haemorrhagic choroidal melanoma together with an anteriorly displaced lens and loss of the anterior chamber.
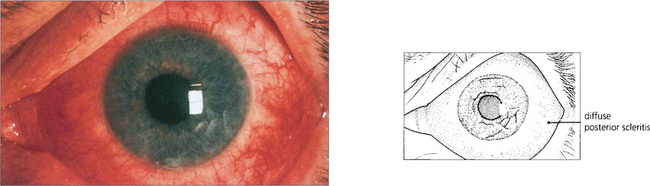
Fig. 8.11 Posterior scleritis may be associated with an annular choroidal effusion that causes the ciliary body to rotate forward about the scleral spur and the iris–lens diaphragm to move forward to produce angle-closure glaucoma. Ciliary body detachment may result in a normal or low IOP, even in the presence of angle closure. This photograph shows a red eye with diffuse anterior and posterior scleritis, although many of these eyes are completely white with inflammation limited to the posterior sclera alone.
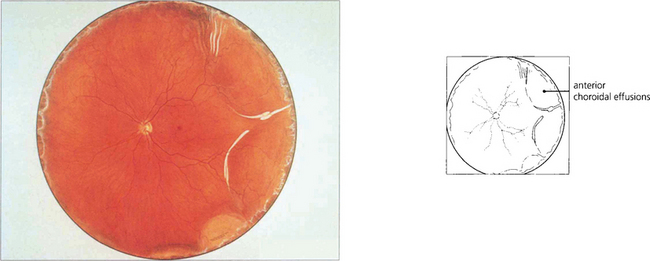
Fig. 8.12 A fundus painting of the same patient reveals an annular choroidal effusion (see also Ch. 5).
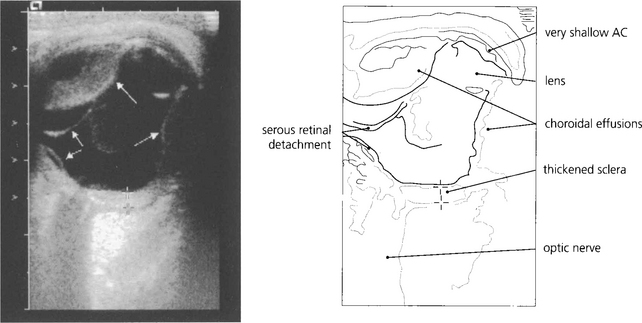
Fig. 8.13 In less obvious cases than the case illustrated, such effusions are easily missed unless the peripheral fundus is inspected carefully under full mydriasis. B-scan ultrasonography is very useful.
By courtesy of Ms M Restori.
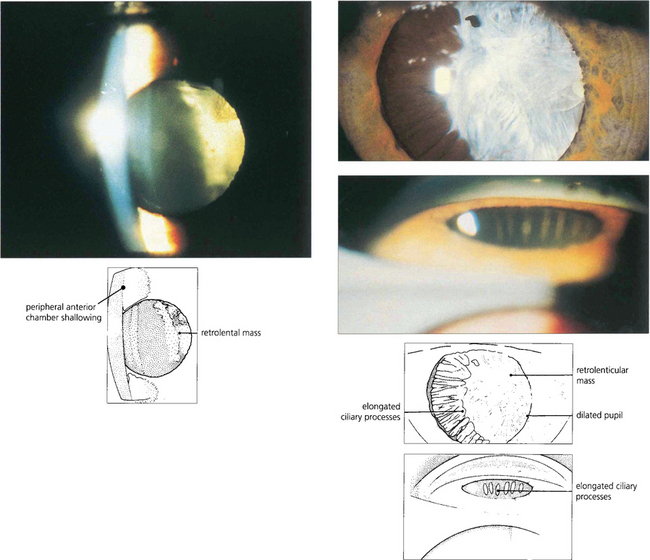
Fig. 8.14 Persistent hyperplastic primary vitreous can produce a contracting fibrotic retrolental mass with forward rotation of the ciliary body and lens–iris diaphragm pushing the iris forwards to occlude the angle. The anterior chamber is often shallow in these eyes making angle occlusion more likely. (Top left) This slit-image photograph shows a shallow anterior chamber and retrolental mass. (Top right) Following mydriasis elongated ciliary processes can be seen being pulled into the mass. (Bottom right) Gonioscopy demonstrates traction and elongation of the ciliary processes.
Malignant glaucoma (ciliolenticular block or aqueous misdirection syndrome)
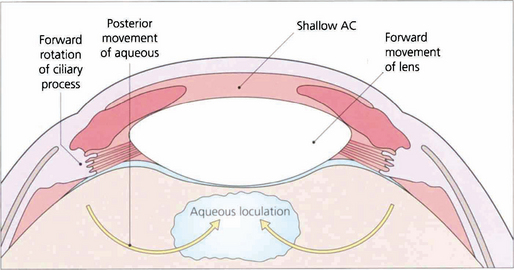
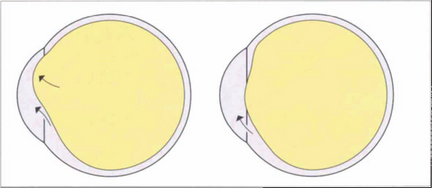
Fig. 8.15 This diagram illustrates how aqueous passes posteriorly and then pushes the lens–iris diaphragm forwards.
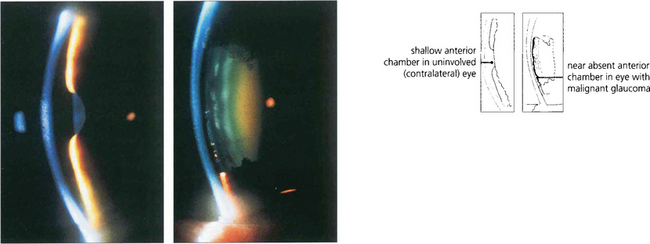
Fig. 8.16 These two slit-lamp photographs of the anterior segments of each eye of a patient demonstrate a shallow anterior chamber in the right eye (left), whereas the left eye (right) has virtually no anterior chamber. The left eye had recently undergone a trabeculectomy followed by loss of the anterior chamber from malignant glaucoma. It is worth using topical atropine in higher-risk eyes at the end of filtration surgery to prevent this.
Synechial closure of the angle
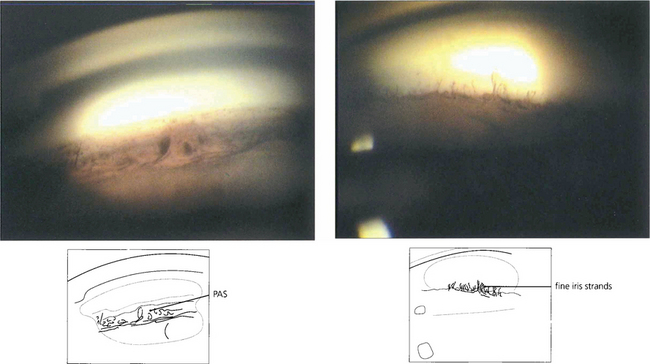
Fig. 8.17 PAS (left) should be distinguished from fine strands from the anterior iris surface to the trabecular meshwork which may be seen in normal eyes (right).
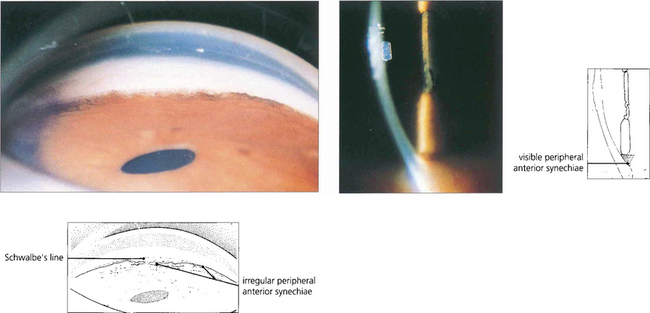
Fig. 8.18 Slit-image and gonioscopic photographs demonstrate the development of PAS in chronic uveitis. Although often confined to the inferior angle such synechiae can extend circumferentially. With sarcoidosis, trabecular granulomas occasionally form as focal lesions around the circumference of the angle and, if untreated, may produce small areas of PAS (see Ch 10).