Sclera
Maite Sainz De La Maza
C. Stephen Foster
The sclera is a dense connective tissue that accounts for five-sixths of the outer coat of the eyeball. The sclera, remarkable for its strength and firmness (the word sclera is derived from the Greek sklera mannix, which means hard membrane), protects intraocular components from trauma, light, and mechanical displacement; withstands the considerable expansive force generated by the intraocular pressure maintaining the shape of the globe; and provides attachment sites for the extraocular muscles.
A real understanding of scleral development, anatomy, and immunohistochemistry is essential to the study of scleral functions, growth, nutrition, and diseases.
DEVELOPMENT OF THE SCLERA
PRENATAL DEVELOPMENT
Almost all the sclera develops from the neural crest, except a small temporal portion which develops from mesoderm.1,2 (Table 1). The neural crest, mesoectoderm, or ectomesenchyme is the cellular mass situated on either side of the invaginating neural folds. Interestingly, other connective tissues are also of neural crest–mesodermal origin including cartilages, bones, ligaments, tendons, dermis, leptomeninges, and perivascular smooth muscles; this may explain, at least in part, the frequent association of scleritis and arthritis in many systemic connective tissue diseases.3
TABLE 1. Embryology of Ocular Structures | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The developmental process of the human sclera progresses from anterior to posterior and from inside to outside.4 The human eye develops early in week 4 as an evagination from the ventral lateral aspect of the neural tube or neuroectoderm at the level of the forebrain in the diencephalon. The end of the evagination becomes slightly dilated to form the optic vesicle. At the same time a small area of surface ectoderm overlying each optic vesicle thickens, forming the lens placode, which invaginates to become the lens vesicle. At this time there are three waves of neural crest mesenchymal invasion. The first is responsible for the corneal endothelium and trabecular meshwork, the second for the corneal and scleral fibrocytes, and the third for iris and choroidal stroma. By week 5 of development each optic vesicle invaginates to form the double-layered optic cup or neuroectoderm that is surrounded by neural crest which is also of ectodermal origin. The differentiation of neural crest cells into sclera and choroid occurs by week 6 of development in humans in the region anterior to the equator (about day 43 of development),5 progresses backward to the equator by week 8, and reaches the posterior pole by week 12.1 This differentiation is induced by the retinal pigment epithelium.6,7,8 The sclera as well as the choroid and the retinal pigment epithelium requires the presence of the developing lens for normal growth and change in shape, structure, and function.1 By the 4th month circularly oriented scleral fibers form the scleral spur, and by the 5th month scleral fibers around the axons of the optic nerve form the lamina cribrosa.1,4 Arrest of fetal development at this stage or the failure to lay down new collagen on the inner aspect of the posterior sclera might well account for some of the staphylomatous changes found in congenital myopia and disc changes found in some patients with congenital glaucoma.
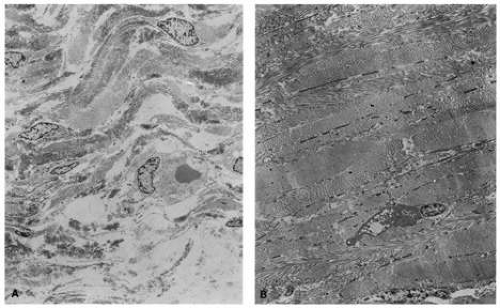
Ultrastructural studies show that developmental events of the sclera begin in the region anterior to the equator at approximately day 43.4,5 The late mesenchymal cells or very early fibroblasts of the anterior portion possess elongated nuclei and many glycogen granules and lipid vacuoles whereas those of the posterior portion possess round-to-oval nuclei and few glycogen granules and lipid vacuoles. The late mesenchymal cells or very early fibroblasts of the anterior and posterior portions contain many free ribosomes and polyribosomes, as well as immature rough-surfaced endoplasmic reticulum and Golgi complex. The early fibroblasts begin the synthesis of glycoproteins, glycosaminoglycans (especially hyaluronic acid), collagen, and elastin between day 43 and 50, thus filling the intercellular space. Developmental events directed from inside outward begin at week 7.2 with a marked increase in the inner portion in glycogen granules and lipid droplets of the cells, and in number and average diameter of collagen fibrils. Cytodevelopment of the sclera is characterized by decrease of ribosomes, polyribosomes, glycogen granules, and lipid vacuoles, and by increase of rough-surfaced endoplasmic reticulum and Golgi complex components. Development of intercellular substances is characterized by an increase in the number and average diameter of collagen fibrils (Fig. 1) and in the amount of elastic deposits with electron-translucent central cores. By week 10.9 there are no more differences between the inner and outer portions. By week 13 there are no more differences between the anterior and posterior portions. By week 24, fetal sclera has the same ultrastructural characteristics as adult sclera. Between week 6 and week 24 there is a threefold increase in thickness, possibly by progressive laying down of collagen fibrils on its inner aspect as more mature collagen fibrils are found in the outer part of the sclera and the younger smaller collagen fibrils on its inner aspect; thereafter the rate of increase diminishes rapidly.
Defects in synthesis of extracellular matrix components during scleral development may account for conditions such as Marfan syndrome, osteogenesis imperfecta, pseudoxanthoma elasticum, Ehlers-Danlos syndrome, congenital myopia, and nanophthalmos.
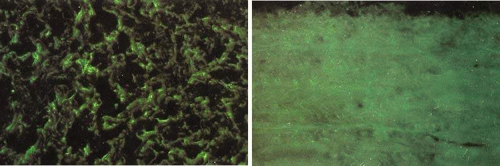
Immunohistochemical studies show that the extracellular matrix of fetal sclera has the collagens I, III, IV, V, and VI, the glycosaminoglycans dermatan sulfate, heparan sulfate, hyaluronic acid, and chondroitin sulfate, and the glycoproteins fibronectin, vitronectin, and laminin.9 Collagens II and VII are not present. Collagens play a major role in strength (collagen I), resiliency (collagen III) and structural integrity (collagens IV, V, VI); glycosaminoglycans in distensibility; and glycoproteins in cell adhesion, growth, differentiation and migration, as well as in other extracellular matrix component organization. Collagen VIII may also be present in human fetal sclera.10 Development of scleral extracellular matrix from fetus into the adult includes increase of collagens I, III, and VI, and decrease of collagen IV and VIII, hyaluronic acid (Fig. 2), fibronectin, vitronectin, and laminin.9,10 By the time the tissue is mature, collagen IV, although abundant in fetal tissue, has almost completely disappeared, except in blood vessels. Heparan sulfate is identified in fetal and adult sclera in small amounts. Increase of collagens I, III, and VI may account for the increase in strength, resiliency, and structural integrity of adult sclera. Decrease of hyaluronic acid may explain the decrease of distensibility of adult sclera. Decrease of fibronectin, vitronectin, and laminin may suggest they play a major role in directing developmental events during the younger gestational periods, including cell and extracellular matrix organization.
POSTNATAL DEVELOPMENT AND AGE-RELATED CHARACTERISTICS
Scleral development is determined by the genetic signaling to the fibrocytes of the sclera, and by the concomitant development of the adjacent structures such as lens, retina, choroid, and the production of aqueous by the ciliary body. During this period of growth there is an increase in axial length in order to acquire a state of emmetropia. This increase in axial length occurs in two stages, an infantile phase which is up to 3 years and then a slower juvenile phase which is up to 13 years; after this age the eye is fully developed.
The postnatal sclera is relatively thin, allowing the pigment cells of the choroid to show through, giving a bluish color. It is also somewhat distensible, allowing the sclera to stretch as a result of increased intraocular pressure in infantile glaucoma (buphthalmic globe). The relatively thin, bluish, distensible, small, and translucent postnatal sclera gradually becomes thicker, whiter, less distensible, larger, and more opaque as the eye goes through childhood and puberty.
Although the adult sclera is poorly distensible, ectasias (localized protrusions of thin sclera) or staphylomas (localized protrusions of thin sclera lined by uveal tissue) can appear at any age after damage (trauma or inflammation). The water content of the adult sclera ranges from 65% to 75%.11 The sclera appears opaque if the water content is between 40% and 80% but becomes translucent if it falls below 40% or rises above 80%.12 This is especially evident in surgical procedures such as strabismus surgery or retinal detachment in which conjunctiva and extraocular muscles are temporally removed from the underlying sclera. The exposed sclera becomes dry and therefore appears translucent unless it is continuously moistened. Similar changes occur after removal of perilimbal conjunctiva in surgical procedures such as excision of pterygium or other limbal lesions. The exposed sclera, adjacent to small elevations of conjunctiva, becomes dry because of the interference in the lubricating effect of the tear film. The dry spots, called dellen, dissappear after rehydration of the area with artificial tears or eye patching.
The increase in transparency after inflammation is the result of rearrangement of the fibrils of the sclera and physiochemical changes; it is only rarely caused by true thinning of the sclera.
In the elderly, the sclera is even less distensible, has decreased water content, and contains fewer glycosaminoglycans.13 This is the result of a progressive cross-linking of the lysine residues of collagen and a decrease in the size of the interfibrillar spaces, possibly as the result of changes within the proteoglycans. Other age-related changes are the subconjunctival deposition of lipids such as cholesterol esters, free fatty acids, triglycerides, and sphingomyelin, which give the sclera a yellowish color.14,15 Calcium phosphate may also be deposited in small rectangular or ellipsoid areas with a vertical axis longer than the horizontal one (approximately 6 mm high and 1 mm wide) just anterior to the insertions of medial or lateral rectus muscles. These slate-gray areas are called senile scleral plaques and usually occur in individuals over 70 years of age.16,17 The cause is uncertain but some etiologic possibilities taken either individually or in combination include ischemia secondary to atherosclerosis of the anterior ciliary arteries,18 dehydration,19 constant stress by the rectus muscles,20 and actinic damage from solar irradiation.17 The collagen fibrils themselves become thicker and less uniform, especially in the region of the muscle insertions. Here the sclera becomes progressively thinned, increasing the color contrasts between one part of the sclera and the next.
ANATOMY
GROSS AND MICROSCOPIC ANATOMY
The surface of the eyeball is formed by two spherical connective tissue segments of different sizes, one posterior and the other anterior.21 The posterior opaque one is the sclera, accounting for five-sixths of the eyeball with a radius of curvature of 12 mm. The anterior transparent one is the cornea, accounting for one-sixth of the eyeball, with a radius of curvature of 8 mm. Scleral thickness varies: the thickest part is near the optic nerve (1 mm); it decreases gradually at the equator (0.4 to 0.5 mm), reaching a minimum immediately behind the rectus muscle tendinous insertions (0.3 mm), and increases at the rectus muscles tendinous insertions (0.6 mm) and in the area adjacent to the limbus (0.8 mm). The collagenous fibrils of the rectus muscle tendons interweave with the collagenous fibrils of the sclera making the fusion inseparable. The traumatic scleral rupture usually occurs immediately behind the insertion of the recti, at the equator or in an area parallel to the limbus opposite from the site of the impact.13,22 It is important to remember how thin the sclera is behind the insertions of the recti when tendons must be sutured to the sclera in tendon recessions or advancements as part of strabismus surgery.
The rectus muscle insertions are progressively more posterior and follow a spiral pattern described by Tillaux and hence called the spiral of Tillaux (Fig. 3). The medial rectus inserts 5.5 mm posterior to the limbus; the inferior rectus, 6.5 mm; the lateral rectus, 6.9 mm; and the superior rectus, 7.7 mm. The insertions of the superior oblique and inferior oblique muscles are posterior to the equator. The long tendon for the superior oblique muscle inserts superiorly and slightly laterally, inferior to the superior rectus muscle; the line of insertion is convex posteriorly and laterally. The inferior oblique muscle inserts posterolaterally. Because this muscle has no tendon, the muscular fibers attach directly; the line of insertion is convex superiorly and laterally. The most posterior point lies 5 mm temporal to the optic nerve, external to the macula.
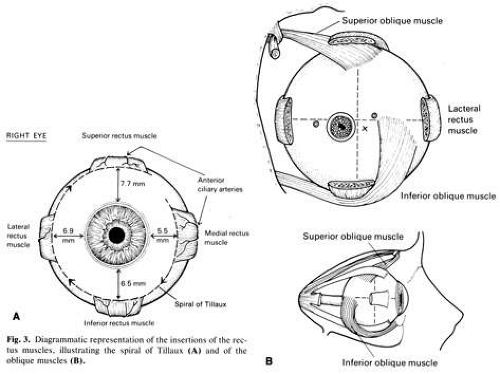 Fig. 3. Diagrammatic representation of the insertions of the rectus muscles, illustrating the spiral of Tillaux (A) and of the oblique muscles (B). |
Tenon’s capsule, the fascial sheath of the eyeball, supports the eyeball within the orbit separating it from the orbital fat and permits the eyeball movement produced by the extraocular muscles.21 Tenon’s capsule is a membrane that extends anteriorly from the limbus backwards to ensheath the extraocular rectus muscles. Posteriorly, it envelopes the globe and fuses with the optic nerve dural sheath and with the sclera around the exit of the optic nerve. Close to the optic nerve, Tenon’s capsule is penetrated by the long and short ciliary nerves and vessels, and by the vortex veins. It is closely connected to the underlying outer portion of the sclera or episclera by delicate lamellae, particularly at the limbus and at the muscle tendon insertions anteriorly and at the optic nerve dural sheath posteriorly. Tenon’s capsule is thin at the limbus but becomes thicker about 3 mm backward until over the muscle tendon insertions. After being penetrated by the tendons of the six extraocular muscles, Tenon’s capsule reflects on each tendon, forming a tubular sleeve. The tubular sleeves for the medial and lateral recti attach to the lacrimal and zygomatic bones, respectively; because they limit the action of these muscles on the eyeball they are called the medial and lateral check ligaments. Behind the muscle insertions Tenon’s capsule becomes thinner except in the inferior part of the eyeball from one check ligament to the other where it thickens to form the suspensory ligament of Lockwood. Tenon’s capsule is very thin posteriorly, especially at the optic nerve where it fuses with the dural sheath and with the sclera.
Scleral Foramina
Anatomically the sclera forms an incomplete sphere interrupted by two foramina, one anterior for the cornea and the other posterior for the optic nerve.
ANTERIOR SCLERAL FORAMEN.
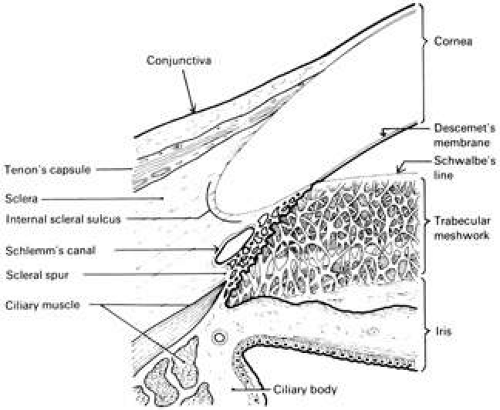
The anterior scleral foramen is an anatomic concept of the sclera without the cornea. It is funnel shaped with an elliptical appearance externally (horizontal diameter of 11.6 mm and vertical diameter of 10.6 mm) and a circular appearance internally (diameter of 11.6 mm). The sclera merges with the cornea at the anterior scleral foramen forming the corneoscleral junction or limbus, an area measuring approximately 1.5 to 2 mm wide that has a convex corneal side and a concave scleral side; the scleral side is formed by the external scleral sulcus in its outer surface, and by the internal scleral sulcus in its inner surface (Fig. 4). The external layers of the internal scleral sulcus merge with the stroma of the cornea. The internal layers of the internal scleral sulcus contain the trabecular meshwork and Schlemm’s canal anteriorly, and the scleral spur posteriorly; the trabecular meshwork merges with Descemet’s membrane. Because the scleral spur attaches to the meridional ciliary muscle, tension on the scleral spur by the muscle opens the trabecular meshwork.23
POSTERIOR SCLERAL FORAMEN.
The sclera allows the exit of the optic nerve through the posterior scleral foramen. The posterior scleral foramen also is funnel shaped but in the sense opposite to the anterior scleral foramen: the external diameter is of 3 to 3.5 mm and the internal diameter is of 1.5 to 2 mm. The site of this perforation is located 3 mm medial to the midline and 1 mm below the horizontal meridian. In this region the outer two thirds of the sclera continue backward along the nerve to blend with the dural and arachnoid sheaths of the optic nerve. The inner third of the sclera provides small perforations covered by glial tissue that allow the passage of the axons of the optic nerve. This sievelike area, which is slightly concave and faces inward, is known as the lamina cribrosa.24 After piercing the lamina cribrosa, the axons of the optic nerve become myelinated. One of the small perforations is larger than the rest and permits the passage of the central retinal artery and vein. Because the lamina cribrosa is a relatively weak area, it tends to bulge outward with an increase of intraocular pressure, forming a cupped disc. Here also, since the axons of the optic nerve and the vessels are enclosed within tiny perforations covered by glial tissue, inflammatory swelling easily leads to axonal and vessel strangulation.
Layers of the Sclera
The sclera may be divided into three layers: the episclera, the scleral stroma, and the lamina fusca.
THE EPISCLERA.
The episclera is the superficial aspect of the sclera that is continuous superficially with Tenon’s capsule and merges with the underlying scleral stroma. Unlike Tenon’s capsule, it has the bundless of collagen circumferentially arranged; and unlike the scleral stroma, it has a rich blood supply anteriorly. The loosely and circumferentially arranged bundles of collagen intermingle with fibroblasts, melanocytes, elastic fibers, proteoglycans, and glycoproteins. The rich blood supply anteriorly is derived from the anterior ciliary arteries and has tight attachments to the subconjunctival tissue, the rectus muscle insertions, and Tenon’s capsule. The scanty blood supply equatorially and posteriorly is derived from the posterior ciliary arteries and has loose attachments to the subconjunctival tissue and Tenon’s capsule. The episclera is thickest anterior to the rectus muscle insertions and becomes progressively thinner toward the back of the eye.
THE SCLERAL STROMA.
The scleral stroma also consists of bundles of collagen intermingled with fibroblasts, melanocytes, elastic fibers, proteoglycans, and glycoproteins. However, the bundles of collagen are thicker, the fibroblasts are thinner, and the proteoglycans and glycoproteins are scantier than those in the episcleral collagen bundles. Unlike corneal collagen bundles, the thickness of the fibrils in scleral stroma varies in each bundle. The bundles of collagen interlace greatly with each other, giving to the sclera strength and resiliency. In the superficial layers of the scleral stroma the anterior circular arrangement and the posterior meridional arrangement are interrupted by whorls and loops, especially around the rectus and the oblique muscles. This arrangement resists the stresses imposed by the pull of the extraocular muscles while at the same time accommodating changes in the intraocular pressure. In the deep layers of the scleral stroma, where the influence of the stresses imposed by the extraocular muscles is absent, the bundles of collagen run meridionally from the corneoscleral junction to the optic nerve. A combination of variability in collagen fibril diameter, interlacing in bundles of collagen, and relative deficiency in water-binding substances accounts for the scleral dull white color.
THE LAMINA FUSCA.
The lamina fusca (the word fusca is derived from the Latin fuscus, which means dark) is the innermost portion of the sclera and receives its name from the large number of melanocytes that have migrated from the underlying choroid, giving to this portion a brown color. Because the lamina fusca has grooves for the passage of ciliary vessels and nerves (emissary canals), melanocytes may pass through, producing dark spots on the episclera. The spots are most commonly seen 3 to 4 mm from the limbus in the superior episclera. An exaggerated number of melanocytes may pass through the emissary canals and invade scleral stroma and episclera. This invasion may be either diffuse in individuals of races whose skin is darkly pigmented or patchy in cases of congenital melanosis oculi and oculodermal melanocytosis (nevus de Ota). Neoplasms, such as malignant melanomas of the uvea, also may emerge through the emissary canals. The lamina fusca is attached to the choroid by fine collagen fibrils, which are easily separated in choroidal detachments or effusions. The bundles of collagen in the lamina fusca become much thinner and are characterized by a great increase of elastic fibers. The ciliary muscle is very strongly attached to the deep surface of the sclera.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree