Rickettsial Organisms in Ocular Disease
Woodford S. Van Meter
James D. Crandall
Douglas G. Katz
Rickettsial disease historically has not been considered a major ocular pathogen, although the incidence and severity of the ophthalmic manifestations of rickettsial disease are becoming increasingly understood. The most common rickettsial diseases seen in general medicine are Rocky Mountain spotted fever (RMSF) and typhus, but the ophthalmologist is most likely to be confronted with cat scratch disease. The ocular manifestations of rickettsial disease are nonspecific inflammatory findings and are generally related to inflammation in the eye caused by proliferation of the organism. Because of the nonspecific nature of the ocular manifestations of the disease, ophthalmologists should be aware of the possibility of rickettsial disease when localized and systemic symptoms of inflammation and vasculitis present in a patient at risk.
Epidemiology
Rickettsiae are small pleomorphic gram-negative bacilli that are obligate intracellular parasites. They can in general survive only briefly outside the host; the exception, Coxiella burnetii, which causes Q fever, is a hearty organism that resists desiccation, heat, and sunlight and is transmitted mainly by airborne spread.1 Rickettsial organisms have been broadly divided into spotted fever and typhus groups based on antigenic similarities and intracellular growth characteristics.1 An overview of common rickettsial diseases and organisms is given in Table 1.
Table 1. Characteristics of Selected Rickettsioses | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Rickettsial organisms are maintained in nature through a cycle involving reservoirs in mammals and vectors in insects. Humans are incidental hosts, and in general, humans are not useful in propagating the organism in nature.1 Rampant outbreaks of potentially fatal disease, such as typhus or trench fever in humans, have occurred when people are crowded together in conditions of poor hygiene. Most rickettsial disease in the United States today occurs when humans have incidental contact with insect vectors in the organism life cycle.
Rickettsial organisms exist in a classical commensal fashion with their insect vectors. One exception is Rickettsia prowazekii, which causes murine typhus; this organism causes the death of its vector, the human body louse, in 1 to 3 weeks. The mammalian reservoirs rickettsiae are many and varied but are generally composed of small animals and livestock.
Rickettsial diseases endemic in the United States today are RMSF (tick), Q fever (tick), and murine typhus (flea).2 Sporadically occurring in the United States still are rickettsialpox (mite) and epidemic typhus (body louse). Brill-Zinsser disease (recrudescent louseborne typhus) in immigrants who lived in Europe during World War II (Table 1) was endemic for a time but has effectively been eliminated.
Clinical Diagnosis
The findings of fever, headache, fatigue, lymphandenopahty, and rash in the appropriate season (usually spring and summer) should alert the physician to consider rickettsial etiology. A careful clinical history with attention to possible vector exposure (e.g., camping, hiking, tick or flea exposure) can identify patients who may be at risk. The pathogenesis of rickettsial disease is vasculitis that manifests as a cutaneous rash caused by the proliferation of organisms on the endothelial lining of small arteries, veins, and capillaries; Q fever, however, produces no rash.1 Rickettsial organisms can be found in the cytoplasm of vascular endothelial cells in histopathologic biopsy specimens in most cases; one exception is that RMSF organisms can be found in the nuclei of infected cells. Intracellular organisms transmitted by tick bites can also be identified by immunofluorescence, which aids in diagnosis by using skin biopsy specimens during the skin rash stage. The most common confirmatory test is measurement of serum antibody titers (see section on Laboratory Diagnosis).
Rickettsial Diseases
Cat Scratch Disease
Cat scratch disease, caused by Bartonella henselae, is the rickettsial disease most likely to be seen by ophthalmologists. B. henselae is the etiologic agent of both bacillary angiomatosis and cat scratch disease. Cat scratch disease (benign reticuloendotheliosis) is characterized by regional lymphadenitis that may be suppurative, secondary to skin lesions attributed to a cat scratch. A scratch or close contact with a cat is followed in 3 to 4 days by unilateral regional lymphadenopathy, which is usually benign3,4 but may progress to more severe systemic manifestations.5
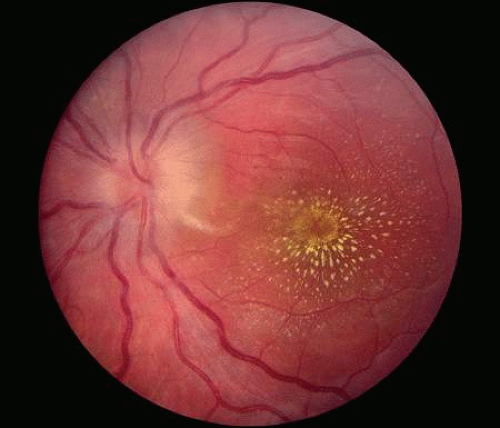
The most common ophthalmic manifestation of cat scratch disease is Parinaud’s oculoglandular syndrome (i.e., granulomatous conjunctivitis with preauricular adenopathy).6,7 Decreased vision in patients with cat scratch disease can be caused by neuroretinitis or Leber’s stellate neuroretinitis (optic disc edema with a macular star of exudate [ODEMS]8 (Fig. 1). Massive posterior uveitis, vitreous opacities, and resultant retinal detachment have been reported with positive vitreous cultures for the B. henselae bacillus.9 Peripapillary angiomatosis can also be seen on retinal examination.10
Bacillary angiomatosis is a systemic disease characterized by multiple subcutaneous nodules that histologically show vascular proliferation with the nodules. Bacillary angiomatosis is caused by B. henselae or Bartonella quintana, is seen over a wide age range, and initially presents as small nodules in the conjunctiva11 or on the skin.12 The nodules contain proliferating endothelial cells and bacteria. Bacillary angiomatosis is a potentially life-threatening disease that can affect many other organ systems; however, it does respond well to systemic antibiotic treatment (i.e., quinoloues). The specific relationship between the bacteria and the endothelial cell proliferation is not known.
B. henselae is closely related to B. quintana, the agent responsible for the epidemic outbreak of trench fever among the Allied forces in France in World War I.13 Trench fever was the most prevalent disease among allied forces in France in World War I, then became dormant and reemerged in World War II. It is characterized by fever, headache, malaise, arthralgia, conjunctivitis, and splenomegaly; the disease can range in severity from nearly asymptomatic to persistent fever lasting for 3 months. It is rarely seen today and exists only in inner-city pockets of homeless persons, refugees, and chronic alcohol abusers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree