Rhinoplasty: Introduction
The term rhinoplasty is derived from the Greek word “rhinos” which means nose and “plastikos” which means “to shape.” Rhinoplasty is surgery that changes the appearance of the nose. More recently, the term “functional rhinoplasty” has been used to describe surgery that, in addition to changing appearance, also improves the function. Nasal reconstruction was first described in Ancient India by Sushruta in his text Sushruta Samhita circa 500 BC. Sushruta, considered to be the father of plastic surgery, used a variety of techniques to reconstruct nasal amputations, a common form of capital punishment at the time. These included pedicled, rotation flaps of the cheek and forehead. In the late 1500s, Professor Gaspare Tagliacozzi published a surgical textbook in Bologna showing nasal reconstruction using a flap from the upper arm. In the mid-1800s, Johann Freiderich Dieffenbach further refined the plastic surgical procedures of his time in his textbook titled Operative Surgery. He described techniques to reduce the size of the nose, such as excising a portion of abnormally enlarged nasal ala and making cruciate excisions of skin and cartilage. Aesthetic rhinoplasty though an intranasal approach was first described by American otolaryngologist John Orlando Roe in 1887 in his landmark article “The deformity termed ‘pug nose” and its correction by a simple operation.” In the late 1800s, Jacques Joseph arose as one of the most important figures in facial plastic surgery and was the pioneer of modern rhinoplasty. Joseph gave numerous lectures and practical courses on rhinoplasty that were attended by surgeons like Gustave Aufricht, Joseph Safian, Jacques Maliniac, John Maurice Converse, and Samuel Fomon. Fomon then began teaching a rhinoplasty course based upon Joseph’s techniques. Two notable otolaryngologists who attended the courses were Maurice Cottle and Irving Goldman. As these surgeons trained other surgeons and surgical techniques became more refined, modern rhinoplasty was developed.
Anatomy
- The nose is made up of nine subunits—nasal dorsum, tip, columella, the paired nasal sidewalls, ala/sills, and soft triangles
- The three major tip support mechanisms are the strength and integrity of the lower lateral cartilages, and their attachments to the septum and to the upper lateral cartilages
- The internal and external nasal valves account for much of the nasal resistance to airflow and must be accounted for when performing rhinoplasty.
The external surface of the nose is divided into nine subunits. They consist of the nasal dorsum, tip, columella, the paired nasal sidewalls, ala/sills, and soft triangles. The subunit principle described by Burget and Menick is based upon the notion that the human eye detects the shadowed valleys and lighted ridges of the nasal surface. This principle applies equally in nasal cosmetic surgery and in nasal reconstruction. In cancer or trauma, if more than 50% of a nasal subunit is lost, the remainder of the subunit should be removed. Thus, the whole subunit is replaced with scars designed to lie in the shadowed borders between subunits.
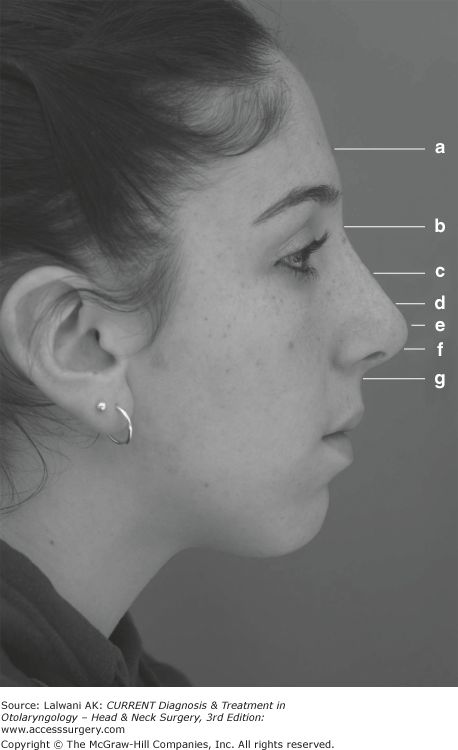
There are numerous facial and nasal anatomic landmarks that must be understood prior to performing an appropriate analysis (Figure 75–1). The ideal facial height divides the face into equal thirds between the trichion, glabella, subnasale, and menton. The ideal facial width divides the face into equal fifths. Thus, the width of one eye should be one fifth of the total facial width and equal to the intercanthal distance and nasal base width. Deviations from these ideals due to racial and ethnic differences are common.
The nose is composed of a bony-cartilaginous framework that is enveloped by a skin-soft tissue covering. This covering is thick at the nasion and tip and thin over the rhinion. This is important when reducing the bony and cartilaginous nasal dorsum as the varied skin thickness will influence the ultimate dorsal contour. Deep to the dermis, there are five soft-tissue components: a superficial fatty panniculus, a fibromuscular layer, a deep fatty layer, a longitudinal fibrous sheet, and an interdomal ligament. The fibromuscular layer consists of the nasal mimetic muscles that are encased and interconnected by the nasal superficial musculoaponeurotic system (SMAS). This nasal SMAS is continuous with the SMAS of the face. The proper plane when elevating nasal tissue whether for a rhinoplasty or nasal reconstruction is in the sub-SMAS plane.
The upper third of the nose consists of the paired nasal bones. These bones articulate superiorly with the frontal bone at the nasofrontal suture, superolaterally with the lacrimal bone, inferolaterally with the frontal process of the maxilla, and inferoposteriorly with the perpendicular plate of the ethmoid bone. The nasion refers to the bony nasofrontal suture, whereas the sellion denotes the soft tissue overlying that area. The radix is the root of the nose that encompasses both the nasion and sellion. The glabella is the prominence of the frontal bone between the eyebrows and is above the radix.
The cartilaginous septum makes up the middle third of the nasal dorsum. It is quadrangular in shape and articulates posteriorly with the bony septum (perpendicular plate of the ethmoid bone and vomer) and inferiorly with the maxillary crest. The caudal aspect of the cartilaginous septum has a defined anterior septal angle and posterior septal angle that play a significant role in the position of the nasal tip.
The upper cartilaginous vault is composed of the paired upper lateral cartilages (ULCs). These structures are triangular or trapezoidal in shape and fuse in the midline to the cartilaginous dorsum. The ULCs are also supported cephalically by their attachments to the nasal bones. The region where the ULCs attach to the under-surface of the nasal bones is called the keystone area. The cephalic aspect of the ULCs may overlap the caudal part of the nasal bones by up to 11 mm. It is imperative to maintain this relationship to prevent collapse of the ULCs and subsequent nasal obstruction. Caudally, the ULCs articulate with the lower lateral cartilages (LLCs) at the scroll.
The lower cartilaginous vault consists mainly of the paired LLCs or alar cartilages. The LLCs, which are extremely variable among individuals, determine the shape and configuration of the nasal tip. The refined tip is described by the double-break appearance, which consists of a supratip and infratip break. The supratip is defined by the junction of the nasal dorsum and the nasal tip, and the infratip is defined by the junction of the tip and columella.
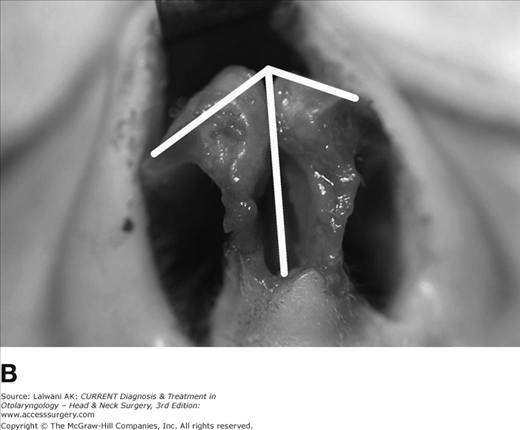
The LLCs are C-shaped and may be divided into three parts: the medial crus, intermediate or middle crus, and lateral crus (Figure 75–2). The medial crura are the narrowest segment of the LLC. Each consists of a footplate segment that flares posterolaterally and an anterior segment that defines the contour of the columella. The medial crura are attached to the caudal septum by fibrous tissue and are separated from each other by loose connective tissue.
The intermediate crura join the medial crura to the lateral crura. The intermediate crura flare posterolaterally away from each other at the angle of divergence. The angle of divergence contributes to the infratip lobule and normally measures approximately 50–60°. Angles greater than 60° typically lead to a wide or boxy tip. The dome is a point where the intermediate crus joins the lateral crus and is the highest and most anterior point of the tip. The domes are joined medially by the interdomal ligaments. The domes correspond topographically to the tip-defining points and as such, surgical maneuvers to modify the domes are used to refine the nasal tip.
The lateral crura are typically convex in shape and extend posteriorly from the intermediate crura. The lateral crura initially parallel the alar rim, but then turn posteriorly, superiorly, and laterally toward the pyriform aperture. There is a variety of anatomic relations between the cephalic margin of the lateral crura and the caudal margin of the ULCs at the scroll region. Variations in width, shape, and strength of the lateral crura influence both the appearance and strength of the nasal tip.
Many surgeons would argue that the key to rhinoplasty is controlling the nasal tip. It is imperative to understand tip support and dynamics in order to achieve predictable results. Two related models have developed to help explain the complexities of the nasal tip cartilages: the tripod theory and the tip support mechanisms.
In the tripod concept, the anatomy of the LLCs is compared to that of a tripod where the conjoined medial crura formed one leg and each of the lateral crura represented the remaining two legs (Figure 75–3). Hence, in theory, changes in the length of the limbs of the tripod lead to predictable changes in the nasal tip position. Decreasing the lengths of all three limbs equally results in tip deprojection whereas increasing the lengths would increase projection. Shortening the length of the medial crura and/or lengthening the lateral crura would result in caudal tip rotation, whereas the opposite maneuvers would lead to cephalic tip rotation.
The nasal tip classically has nine support mechanisms: three major and six minor. The major tip support mechanisms are: (1) the size, shape, and resiliency of the LLC; (2) the attachment of the LLCs to the caudal septum; (3) the attachment of the LLCs to the ULCs at the scroll region. The minor tip support mechanisms are: (1) the interdomal ligament; (2) the cartilaginous dorsal septum; (3) the sesamoid complex; (4) the attachment of the LLC to the overlying SMAS and skin; (5) the nasal spine; (6) the membraneous septum. When performing nasal surgery, tip support mechanisms need to be respected, and if weakened must be reconstituted to ensure a good functional and aesthetic outcome.
The nose is responsible for about two-third of the body’s total resistance to airflow during breathing. There are two main valves in the anterior aspect of the nose that account for the majority of resistance: the internal nasal valve (INV) and the external nasal valve (ENV).
The INV is the narrowest segment of the nasal cavity and is the greatest resistance to nasal airflow. The INV is bordered by the septum, the head of the interior turbinate, the caudal edge of the ULC, and the pyriform aperture. The attachment of the ULC to the septum normally occurs at an angle of 10–15° in Caucasians. A connection at a more acute angle may lead to nasal obstruction. INV static narrowing or dynamic collapse and subsequent nasal obstruction may be caused by previous surgery, trauma, septal deviation, inferior turbinate hypertrophy, scarring, synechiae, or congenital malformations. The ENV is formed by the nasal floor/sill, the columella, and the caudal border of the LLC. ENV static narrowing or dynamic collapse may be caused by prior surgery, weak LLCs, a widened columella, thick skin-soft tissue envelope, deviated caudal septum, or nasal stenosis due to trauma or burns.
Preoperative Planning
- There are numerous ideal aesthetic proportions that are used in the preoperative evaluation
- The standard views for preoperative rhinoplasty include: frontal, three-quarters, lateral, and base.
Although beauty is truly in the eye of the beholder, various formulas and calculations have been derived to determine the ideal aesthetic nasal proportions. Preoperative analysis of the nose and how it relates to the rest of the facial units is the cornerstone of rhinoplasty. Table 75–1 shows the parameters that may be evaluated and analyzed in the frontal, lateral, and basal views.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree