The retrograde technique of cholesteatoma exposure attempts to combine the favorable attributes of canal wall-down and canal wall-up tympanomastoidectomy. The rationale behind this technique is to create a temporary canal wall–down situation by following the cholesteatoma’s growth back from its origin in the tympanic membrane toward the mastoid. This removes the superior aspect of the canal wall to completely expose the critical epitympanum and supratubal recess for disease extirpation. The canal wall is then reconstructed with auricular cartilage from the concha cymba that is securely inset into grooves drilled into the remnant canal wall buttresses. Primary ossicular reconstruction serves as a scaffold for the posterior drum reconstruction, both of which are performed as a single-stage surgery. To prevent recurrent disease, the mosaic cartilage technique is employed to reconstruct the tympanic membrane in close approximation to the reconstructed canal wall. If the anterior drum is also involved, then total cartilage reconstruction is performed with the island technique.
37.2 Patient Selection
The assessment of a patient with cholesteatoma should start at the nose and end at the ear. As most acquired cholesteatomas are believed to be related to some form of Eustachian tube dysfunction, which in turn may be related to sinonasal disease, the patient history should begin here and treatment initiated if indicated. In a child, one should address previous surgical intervention, such as pressure equalizing tubes, adenoidectomy, and allergy or sinus surgery. In adults, sniffing behavior should be assessed as well as sinonasal disease and smoking history. Any vertigo should be noted, which could indicate the possibility of a labyrinthine fistula. The patient should be asked to perform the Valsalva maneuver, with the response in both ears recorded. The physical exam should begin with the opposite ear to determine if the condition is bilateral, perhaps due to more pervasive Eustachian tube dysfunction, and to determine the shape of the normal canal, which can be helpful in the examination of the diseased ear as the latter could show distorted landmarks.
The origin of the cholesteatoma should be noted so that the pattern of cholesteatoma spread can be anticipated. Primary acquired cholesteatomas typically begin as retraction pockets in the pars flaccida (epitympanic cholesteatoma) or posterior pars tensa (mesotympanic cholesteatoma). One should anticipate more extensive involvement of the anterior epitympanum and supratubal recess with epitympanic cholesteatoma, but because the disease enters the mastoid lateral to the incus, the facial nerve and sinus tympani are usually involved less extensively or only later in the course of the disease. Mesotympanic cholesteatoma, on the other hand, involves the facial nerve and sinus tympani very early in the course of the disease, and a more difficult dissection should be anticipated.
A complete audiogram should be performed, including speech discrimination testing. The findings should be supported by the tuning fork exam using at least the 512-Hz fork. A significant sensorineural component to the hearing loss could suggest labyrinthine fistula, especially when associated with any balance disturbance.
Although a computed tomography (CT) scan is not absolutely essential, it can be very helpful with the retrograde technique and is recommended. The CT scan allows development of the mastoid to be noted, but, more importantly, the position of the tegmen tympani can be visualized. The lateral portion of the temporal lobe can be displaced quite inferiorly in some cases, which can make retrograde drilling more challenging, necessitating use of a smaller burr. The extent of the cholesteatoma can usually be ascertained with a CT scan, especially in adult cases, which usually show an expansile mass and destruction of the bony septae. However, even with CT, the extent of involvement in the mastoid can be underestimated, especially in pediatric cholesteatoma where well-developed air cells can be invaded by numerous “octopus tentacles” of cholesteatoma without obvious destruction of the septae.
37.3 Surgical Technique
37.3.1 Cholesteatoma Removal
The mastoid cortex is widely exposed through a traditional postauricular skin incision. A tympanomeatal flap is then developed, and the middle ear is entered inferiorly, away from the cholesteatoma, to determine the extent of disease in the middle ear. As this technique involves extensive drilling in close proximity to the lateral aspect of the head of the malleus and the body of the incus, it is necessary to visualize the incudostapedial joint and the integrity of the lenticular process of the incus as an initial step. Except in cases of very limited retraction pockets, the incudostapedial joint is disarticulated to avoid trauma to the inner ear from the subsequent drilling. A canalplasty is performed posteriorly until air cells can just be visualized through the intact cortical bone of the ear canal. This improves the view of the posterior mesotympanum and facilitates subsequent drilling of the superior canal wall as the cholesteatoma is followed throughout the epitympanum and into the antrum. A prominent tympanosquamous suture and spine are taken off at this point to increase exposure of the pars flaccida.
Drilling for cholesteatoma removal begins on the canal side with a 3-mm to 4-mm cutting bur or a rough-cut diamond bur at the upper posterior quadrant of the posterior canal wall, leaving a thin layer of bone at the scutum to protect the neck of the cholesteatoma, which is removed later with a smooth diamond bur. This drilling differs from a traditional atticotomy in that it extends all the way to the lateral external canal as a groove, with exposure of the tegmen tympani. Anatomical landmarks that can be used to gauge the proper extent of canal wall removal would be the area between the anterior tympanic spine and, inferiorly, the approximate exit of the chorda tympani from the bone (9 o’clock to 1 o’clock in a right ear).
There are two important points to keep in mind during this portion of the drilling. One is that if more than 30% of the canal wall is removed, reconstruction becomes difficult. The most common mistake is to initiate drilling at too inferior a point relative to the anterior tympanic spine, underestimating the extent of anterior-superior involvement. Subsequent drilling to expose the supratubal recess then leaves a larger canal wall defect than initially expected. Therefore, it is always better to initiate drilling superior at the anterior tympanic spine, as approximated by the short process of the malleus. The other important point to remember is that the tegmen at the lateral external canal frequently is more inferior than the more medial tegmen at the level of the epitympanum, so care must be taken to avoid injury to the dura laterally. As mentioned previously, a pre-operative CT can be very helpful to predict the height of the tegmen on the coronal view.
As bone removal continues posteriorly, the antrum is opened and the extent of the cholesteatoma can be appreciated. The goal is to remove only the bone necessary to expose the back edge of the sac, and a complete mastoidectomy is not necessary. Some recent evidence suggests that preserving the mucosa in the mastoid might improve subsequent middle ear/mastoid aeration.1 With a small cholesteatoma in a sclerotic mastoid, the surgeon may frequently find the cholesteatoma extends only to the antrum, so minimal drilling is needed. The sac is followed back as posteriorly as is necessary until normal air cells or cholesterol granuloma is encountered behind the sac. This technique differs from that described by Tos,2 in which a small cavity is created should extensive cholesteatoma be encountered. Instead, the sac is followed toward the mastoid tip, referred to as “turning the corner,” leaving the inferior two-thirds of the posterior canal wall intact to facilitate reconstruction (▶ Fig. 37.1). This modification allows the removal of extensive cholesteatoma in a well-aerated mastoid, as frequently found in children, thus avoiding a canal wall-down situation.
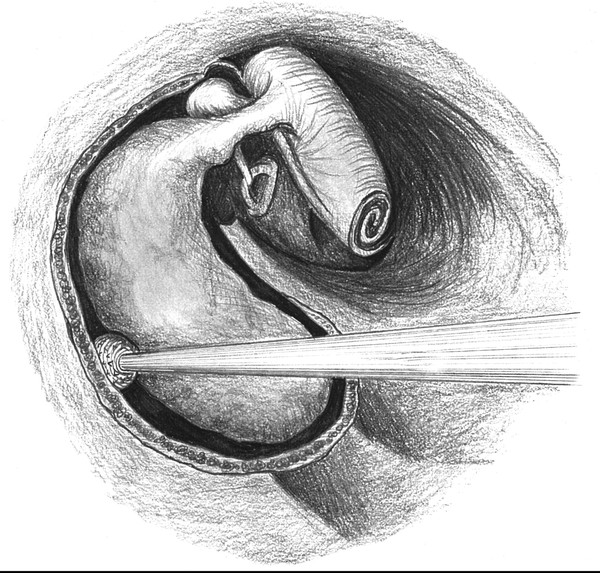
Fig. 37.1 Cholesteatoma is followed back posteriorly, with exposure of the entire sac at its origin from the tympanic membrane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


