Retinopathy and Distant Extraocular Trauma
Isaac A. Loose
Robert P. Schroeder
The retinal manifestations of distant trauma may be asymmetric and vary among patients depending on the type of trauma. Discrepancies in retinal findings relate to an incompletely understood pathogenesis of the retina’s response to distant trauma, as well as the type of trauma sustained. For example, retinal changes resulting from long bone fractures are manifest differently than the retinal changes resulting from whiplash injuries.
The pathophysiologic mechanisms of retinal damage after distant trauma have been debated. Three mechanisms have been proposed to explain the resulting fundus findings: (1) increased intraluminal pressure may damage the retinal vascular endothelial cells; (2) emboli from sources including air, blood products, or fat may also damage the retina, a theory that has been supported in experimental models; and (3) mechanical forces acting at the vitreoretinal interface may damage the retina.
In this chapter we describe six clinical entities: Purtscher’s retinopathy, traumatic asphyxia, fat embolism retinopathy, Valsalva retinopathy, whiplash maculopathy, and shaken baby syndrome. With the exception of whiplash maculopathy, the five retinopathies have some overlap in either clinical presentation or pathophysiology and the categorization of the retinopathies relates more to the type of trauma than to a unique retinal appearance.
PURTSCHER’S RETINOPATHY
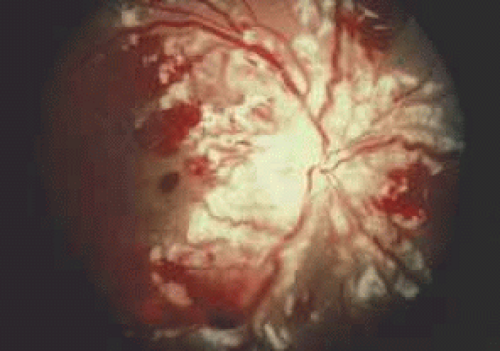
Purtscher’s retinopathy is characterized by retinal hemorrhages, exudates, and decreased vision associated with nonocular trauma (Fig. 1). In 1912, Otmar Purtscher described multiple, white retinal patches and retinal hemorrhages surrounding a normal-appearing optic disc in five patients with visual loss after severe head trauma.1 Most commonly, Purtscher’s retinopathy develops as a sequela of chest-compressing trauma. The severity of the traumatic event is variable, ranging from minimal external trauma to crushing chest wall injuries. The onset of symptoms usually occurs within 2 days after trauma. Both eyes are typically involved, but unilateral cases have been reported.2,3 Patients complain of decreased vision, often from 20/200 (6/60) to counting fingers. Fundus examination usually reveals numerous white retinal patches or confluent cotton-wool spots around the disc, as well as superficial retinal hemorrhages. Other findings include serous macular detachments, dilated and tortuous vasculature, and disc edema. The peripheral retina is commonly spared. Fluorescein angiography can reveal focal areas of arteriolar obstruction, patchy capillary nonperfusion, disc edema, and dye leakage from retinal arterioles, capillaries, and venules.3 Purtscher1 originally proposed that the etiology of the white retinal lesions resulted from lymph extravasated from retinal vessels during a sudden increase in intracranial pressure. In 1962, Marr and Marr4 wrote that the retinopathy resulted from reflux venous shock waves produced from intrathoracic chest compression. Several authors have implicated arteriolar emboli including air and fat as the cause.3,5,6 Other authors have suggested an etiologic role for granulocyte or other blood product emboli formed after complement activation, arguing that microembolization is a mechanism common to the varied clinical settings of Purtscher’s retinopathy.7,8 Interestingly, a Purtscher’s-like fundus picture may occur in several nontraumatic settings, such as acute pancreatitis, chronic renal failure, thrombotic thrombocytopenic purpura lupus erythematosus, and childbirth.7,9,10,11,12 Clinically, the retinal lesions resolve over a period of weeks to a few months.4 After resolution, the fundus may appear normal, but pigment migration and optic atrophy can occur.13 Although visual acuity can remain reduced, the acuity may return to normal or near normal.4
TRAUMATIC ASPHYXIA
Traumatic asphyxia usually results from severe compression of the thorax and is characterized by a striking, ecchymotic mask, or blue discoloration of the upper chest and the face. External ocular involvement is virtually universal in cases of traumatic asphyxia. Patients have ecchymotic eyelids and hemorrhagic conjunctiva but retinal changes occur less commonly. Trampling, suicide attempts by hanging, seizures, vomiting, and childbirth have caused traumatic asphyxia.14 Visual acuity can be unaffected by traumatic asphyxia but may be reduced to no light perception.4 Fundus examination may reveal intraretinal hemorrhages, as well as cotton-wool spots and disc edema. Often the retina may be ophthalmoscopically normal.4,13 In one case of traumatic asphyxia, fluorescein angiography revealed in one eye blockage of fluorescence by retinal hemorrhage, blurring of the background choroidal pattern associated with cotton-wool spots, and hyperfluorescence with dye leakage associated with hemorrhage at the nasal edge of the disc. The other eye was angiographically normal.15 The fundus changes of this patient improved over a period of weeks, but the visual acuity of the right eye had decreased from 20/30 (6/9) to 20/100 (6/30), presumably as a result of mottling and disruption of the retinal pigment epithelium.15 The pathogenesis of traumatic asphyxia retinopathy and Purtscher’s retinopathy may be similar but the ecchymotic appearance associated with traumatic asphyxia separates the two entities. Purtscher’s retinopathy usually has no associated external findings.15 Also, the development of Purtscher’s retinopathy may be slower than the retinopathy of traumatic asphyxia. Again, patients with traumatic asphyxia are treated supportively.
FAT EMBOLISM RETINOPATHY
Fat embolism retinopathy is usually secondary to fat embolism syndrome (FES). Retinal findings variably include cotton-wool spots, intraretinal hemorrhages, and visible emboli. FES was first described in 1861 in patients suffering fractures of medullated bones.16 The most likely fractures producing the syndrome are fractures of the lower extremities and the pelvis.17,18,19 Typically, the manifestations of FES ppear within 24 to 48 hours after the injury, but the syndrome is only recognized in approximately 5% of patients with long bone fractures. Some of these manifestations include petechial rashes, respiratory insufficiency, retinal lesions, and altered mental status.20 In patients with manifest FES, 50% to 60% may have retinal findings.19,20,21 Chuang et al.22 reported that of 100 consecutive long bone fracture cases, four patients demonstrated retinal pathology resulting from subclinical FES. In this series three patients had normal vision and one patient complained of a visual field defect. Fundus examination classically reveals cotton-wool spots and intraretinal hemorrhages. Additional fundus findings include intravascular fat emboli and central retinal artery occlusion.6,22,23,24 This retinopathy has occurred after facial autologous fat injection.25,26 Various alterations in lipid homeostasis are probably involved in the pathogenesis of FES. Retinal microinfarcts from fatty emboli have been demonstrated histopathologically, and this may reveal, at least in part, the etiology of the retinal findings.6 The retinal lesions resolve after resolution of the FES. With resolution, most patients are asymptomatic, although permanent scotomas can occur.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree