Retinitis Pigmentosa and Allied Retinal Diseases
Eliot L. Berson
Introduction
Retinitis pigmentosa and allied retinal diseases are a significant cause of visual loss around the world. The problem is magnified when considering that many young patients are affected and that most patients are legally blind by age 40. Considerable progress has been made in the understanding of these conditions, and medical treatments are now available for some of these disorders. This chapter provides a framework for the diagnosis and treatment of patients with these conditions. The diseases discussed are listed in Table 24-1.
Table 24-1. Retinitis Pigmentosa and Some Allied Retinal Diseases | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
RETINITIS PIGMENTOSA
Retinitis pigmentosa is the name applied to a group of hereditary retinal degenerations with a prevalence of about 1 in 4,000 worldwide.1,2,3,4,5,6 An estimated 50,000 to 100,000 people are affected in the United States. Most cases are inherited by an autosomal-dominant, autosomal-recessive, or X-linked mode of transmission. This condition can also be transmitted by a digenic7 or mitochondrial mode.
Most patients have no associated systemic disease and, therefore, are considered cases of nonsyndromic retinitis pigmentosa. A few cases have associated nonocular disease (syndromic retinitis pigmentosa). The most common syndromic form is Usher syndrome. Some 15% of all cases of retinitis pigmentosa have an associated partial, early onset hearing loss that is nonprogressive (Usher syndrome, type II) and another 2% to 6% have associated profound congenital deafness and vestibular ataxia (Usher syndrome, type I). Others (<1%) have retinitis pigmentosa in combination with onset of hearing loss usually in adulthood that is progressive with or without vestibular ataxia (Usher syndrome, type III).
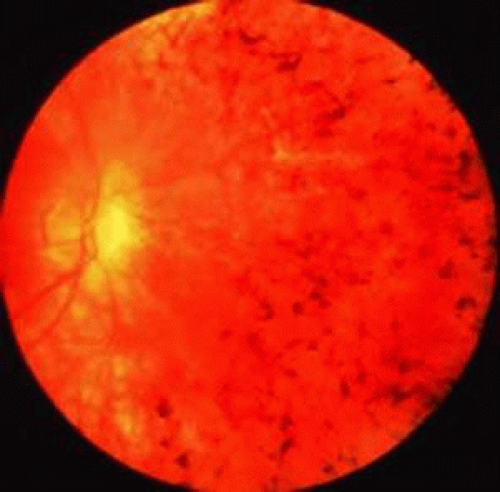
Patients with retinitis pigmentosa typically report difficulty with adaptation and night blindness in adolescence. They lose mid-peripheral and then far peripheral visual field in adulthood. As their condition deteriorates, they develop tunnel vision and a tendency to blue blindness. Most have reductions in central vision between ages 50 and 80. Signs on ophthalmoscopic examination include attenuated retinal arterioles, waxy pallor of the optic discs, and intraretinal bone spicule pigment around the mid-periphery (Fig. 24-1)8,9,10,11,12,13,14,15,16,17,18,19,20 The bone spicule pigment is usually distributed 20° to 40° eccentric to the foveola in the zone where rods are normally in maximal concentration. Most show vitreous cells and a posterior vitreous detachment14 Most develop posterior subcapsular cataracts in adulthood21 An estimated one-third of patients develop cystoid macular edema when evaluated with optical coherence tomography22,23 Refractive errors, such as astigmatism and myopia, are common24,25 Histologic studies of autopsy eyes have shown that loss of vision is caused by degeneration of both rod and cone photoreceptors cells.26,27,28,29,30,31,32,33,34
ELECTRORETINOGRAMS
In 1945, Karpe35 reported that patients with advanced retinitis pigmentosa have very small or nondetectable (<10 μV) ERGs. Subsequently, it has been shown that patients with early retinitis pigmentosa can have reduced but easily detectable ERGs.36,37,38,39 Responses are not only reduced in amplitude but are also delayed with respect to the time interval between stimulus flash onset and corresponding response peaks (i.e., b-wave implicit time).38,39,40,41,42 These ERG changes can be detected in some instances many years before diagnostic abnormalities are visible on fundus examination.41
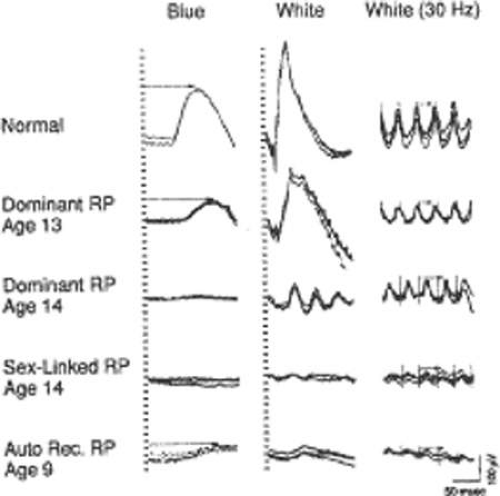
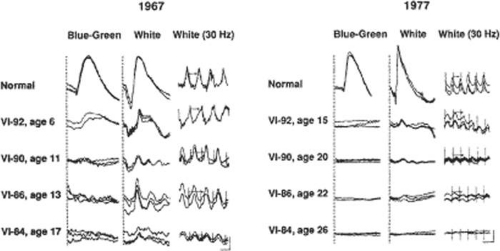
Figure 24-2 illustrates representative full-field ERGs from a normal subject and four children with early retinitis pigmentosa. Rod responses to single 0.5-Hz flashes of blue light (left column) are reduced and, when detectable, are delayed in b-wave implicit times. Cone responses to 30-Hz white flickering light (right column) are normal or reduced in amplitude and normal or delayed in b-wave implicit time. In most cases, cone b-wave implicit times are so delayed that a phase shift occurs between the stimulus flash onset (designated by the vertical lines) and the corresponding response peaks; each stimulus flash elicits the next-plus-one response in contrast to the normal. Mixed cone–rod responses to single 0.5-Hz flashes of white light (middle column) show that the cornea-negative a-wave generated by the photoreceptors is reduced in amplitude in all genetic types; this reflects the early involvement of the photoreceptors in this condition.41
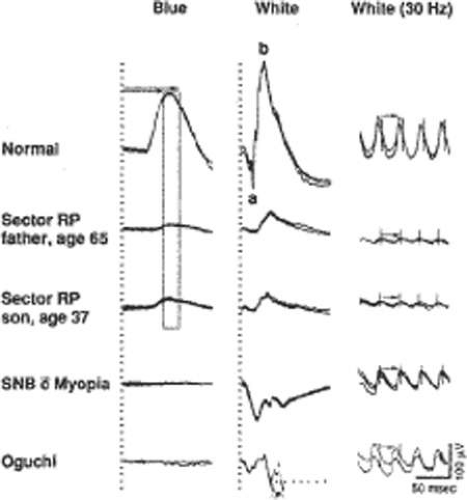
The reduced and delayed ERGs observed in patients with widespread progressive forms of retinitis pigmentosa contrast with the reduced ERGs with normal b-wave implicit times recorded from patients with self-limited sector retinitis pigmentosa. Figure 24-3 illustrates full-field responses from a father and son with dominantly inherited sector retinitis pigmentosa separated in age by almost 30 years; they have comparably reduced amplitudes with normal b-wave implicit times. Patients with sector retinitis pigmentosa usually have patches of intraretinal pigment confined to one or two quadrants of the peripheral fundus with consequent loss of peripheral rods and cones and consequent reductions in both rod and cone full-field ERG amplitudes. ERGs recorded from patients with sector retinitis pigmentosa are similar to those recorded from patients who have large chorioretinal scars in the periphery.41
Full-field ERG testing can be used both to identify which patients have widespread progressive forms of retinitis pigmentosa and to establish which relatives are normal. Relatives of patients with retinitis pigmentosa, age 6 or older, with normal rod and cone ERG amplitudes and implicit times, have not been observed to develop widespread progressive forms of retinitis pigmentosa at a later time.41,42,43
CARRIERS OF X-LINKED RETINITIS PIGMENTOSA
Females with the carrier state of X-linked retinitis pigmentosa can present with a patch of bone spicule pigmentation in the periphery or an abnormal tapetal reflex in the macula. Less than 50% of carriers of child-bearing age show diagnostic findings on ophthalmoscopic examination, whereas more than 90% have abnormal ERGs.44 Abnormal ERGs in obligate carriers are either reduced in amplitude or delayed in cone b-wave implicit time, or both, in one or both eyes (Fig. 24-4).44,45 Daughters of obligate carriers can have either normal ERGs or abnormal ERGs similar to those recorded from obligate carriers.44
Female carriers of X-linked retinitis pigmentosa can have a slowly progressive retinal degeneration, although the natural course remains to be clarified. Some carriers have had considerable loss of visual field and substantial reductions in ERGs by age 70.44 The abnormal ERGs of carriers of X-linked retinitis pigmentosa contrast with the normal ERGs and normal fundi found in obligate female carriers of autosomal-recessive disease.44 Carriers of X-linked retinitis pigmentosa have a 50% chance of having an affected son and a 50% chance of having a carrier daughter with each childbirth.
NATURAL COURSE OF RETINITIS PIGMENTOSA
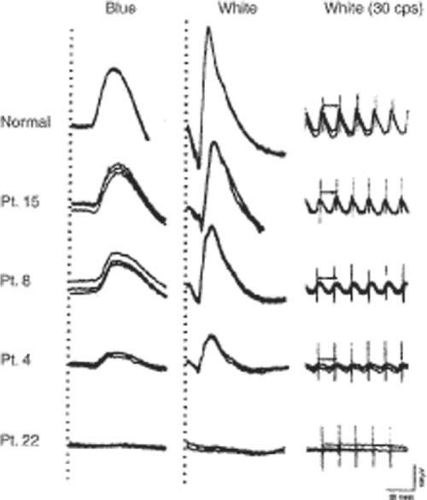
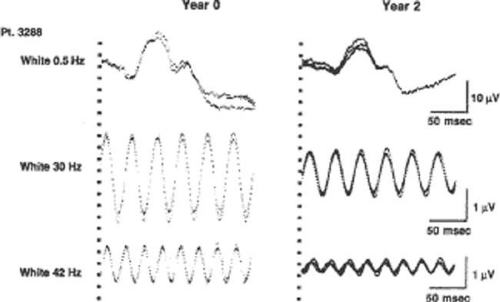
The ERG provides a quantitative measure of remaining retinal function in patients with retinitis pigmentosa. Figure 24-5 illustrates ERGs from affected patients followed over a 10-year period; responses become smaller as the condition progresses. Responses less than 10 μV are not detectable with conventional recording techniques (i.e., without signal averaging). Narrow-bandpass filtering and computer averaging have extended the range of detectability of responses from affected patients almost 100-fold so that responses can be quantitated throughout almost the entire course of the disease. ERGs can now be recorded that are as low as 1.0 μV to 0.5 Hz flashes of white light (norm ≥350 μV) with signal averaging alone and, with narrow-bandpass filtering and signal averaging combined, as low as 0.05 μV to 30 Hz white flicker (norm ≥50 μV). In an adult male with X-linked retinitis pigmentosa (whose ERGs could not be quantitated without signal averaging) computer-averaged ERGs show changes in ERG function over a 2-year period (Fig. 24-6). Whereas about 70% of patients have nondetectable or flat ERGs (i.e., <10 μV) with conventional ERG testing, narrow-bandpass filtering with computer averaging has made it possible to detect retinal function in more than 90% of an outpatient population with retinitis pigmentosa who have some remaining vision.46,47 Patients become virtually blind (i.e., loss of capacity to walk out of a well-lighted room without assistance) when their cone ERG amplitudes decline to 0.05 μV or less.48
A cone ERG actuarial table (Table 24-2) has been developed to provide estimates of long-term visual prognoses for patients with typical retinitis pigmentosa. The table is derived from data on 6,553 visits among 1,039 patients age 2 to 71 years followed for 3 to 29 years.48 The table is based on the proposal that the average rate of decline of cone retinal function in retinitis pigmentosa can be described by an exponential function, which, in practical terms, can be used to estimate the long-term course of disease in most patients with this condition. It has been hypothesized that patients who lose vision in later life have more cone ERG function near birth, whereas those who lose useful vision at a younger age have less cone ERG function near birth but cone ERGs in both are declining at a similar rate.48 The table can be used to calculate the expected number of years for an average patient with a 30-Hz cone ERG at a given age to decline to 0.05 μV. If patients wish to have a more precise estimate, they should have narrow-bandpassed filtered, computer-averaged cone ERG testing preferably at 2-year intervals for three to four times to clarify to what extent the rate of their ERG decline corresponds to the average rate. It has been reported that as many as 25% of adult patients with nondetectable conventional ERGs (i.e., <10 μV) have sufficient cone ERG function (i.e., ≥3.5 μV at age 40 with narrow-bandpassed filtering and computer averaging) to suggest that they will retain some useful vision until age 80 or beyond without treatment.48 Knowledge of long-term visual prognoses often reduces patient anxiety and helps patients plan for their future.
Table 24-2. Cone ERG Actuarial Table for Retinitis Pigmentosa | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
MOLECULAR GENETIC STUDIES OF RETINITIS PIGMENTOSA
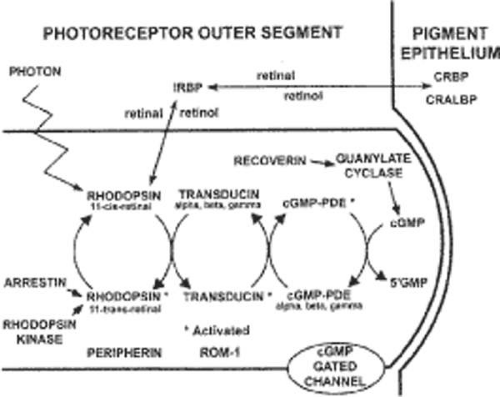
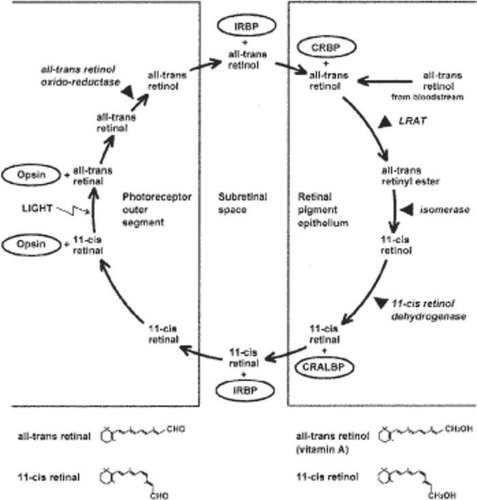
Substantial genetic heterogeneity exists among patients with retinitis pigmentosa with abnormalities in over 50 genes identified as of 2009; an updated list is maintained on the RetNet site at http://www.sph.uth.tmc.edu/Retnet/sum-dis.htm. Genes so far identified as causes of nonsyndromic retinitis pigmentosa as well as Usher syndrome are given in Table 24-3.49 Some genes can affect the phototransduction cascade (Fig. 24-7) or the retinoid cycle (Fig. 24-8).
Table 24-3. Estimated Proportions of Cases of Retinitis Pigmentosa (RP) Caused by Identified Genes (Excluding Syndromic RP Except for Usher Syndrome) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Causative genes have been subclassified based on the known or presumed function of encoded proteins as follows: (a) phototransduction cascade (e.g., RHO, rod PDE6A, rod PDE6B, CNGA1, CNGB1, SAG); (b) vitamin A metabolism (e.g., ABCA4, RLBP1, RPE65, LRAT, RGR); (c) photoreceptor structure (e.g., RDS, ROM1, FSCN2, TULP1, CRB1, RP1); (d) signaling or cell-cell interactions (e.g., SEMS4A, CDH23, PCDH15, USH1C, USH2A, MASS1, USH3A, RP2); (e) RNA intron splicing factors (e.g., PRPF31, PRPF8, PRPF3, RP9); (f) trafficking of intracellular proteins (e.g., MYO7A, USH1G); (g) maintenance of cilia or ciliated cells with a possible role in intracellular trafficking (e.g., BBS1, BBS2, ARL6, BBS4, BBS5, MKKS, BBS7, TTC8, PTHB1, RPGR); (h) regulation of the carbon dioxide-bicarbonate balance (e.g., CA4); (i) phagocytosis (e.g., MERTK); and (j) other yet to be defined functions of the photoreceptors and retinal pigment epithelium (e.g., CERKL, IMPDH1, BBS10).49
The most common genes causing retinitis pigmentosa are the rhodopsin (RHO) gene, the USH2A gene, and the retinitis pigmentosa GTPase regulator (RPGR) gene. The course of disease in these three types has been described.50,51,52 The genes listed in Table 24-3 account for about 50% to 60% of cases of retinitis pigmentosa in the United States.
It should be noted that defects in the same gene can result in different phenotypes; for example, most rhodopsin mutations lead to retinitis pigmentosa, but some cause stationary night blindness. Defects in the ABCA4 gene can result in juvenile macular degeneration or a generalized cone-rod degeneration (i.e., an atypical form of retinitis pigmentosa discussed later in this chapter). Variable clinical expression can exist among patients with the same gene defect, suggesting that factors other than the gene defect itself (e.g., diet; environment; modifier genes) affect the course of the disease with possible implications for therapy.18
TREATMENT TRIALS FOR RETINITIS PIGMENTOSA
Many treatments have been attempted for the common forms of retinitis pigmentosa, including various vitamins and minerals, vasodilators, tissue therapy with placental extract, cortisone, cervical sympathectomy, injections of a hydrolysate of yeast RNA, ultrasound, transfer factor, dimethyl sulfoxide (DMSO), ozone, muscle transplants, and subretinal injections of fetal retinal cells.53,54,55,56,57,58,59,60 None of these has been shown to have proven therapeutic benefit. A study of patients evaluated before and after receiving electric stimulation, autotransfused ozonated blood, and ocular surgery in Cuba showed that this intervention provided no benefit and raised the possibility that this intervention was aggravating the course of the disease.60 None of these attempts at treatment was conducted with a randomized, controlled, double-masked protocol, which is necessary to avoid possible patient or examiner biases. Most of these studies were performed without electroretinographic data as an end point for evaluating efficacy, so that the amount of remaining retinal function could not be quantitated in an objective manner.
Claims of success with one or another treatment for patients with retinitis pigmentosa that are based solely on subjective reporting of improved visual function are to be interpreted with caution. Spontaneous fluctuations in visual acuity and visual field are well known in this condition. Given the slow course of retinitis pigmentosa without treatment, it will usually require several years to assess whether or not any proposed treatment has an effect on stabilizing or slowing the course of the disease. The problem of assessing treatments may be further complicated by the genetic heterogeneity of this condition and the stage of disease at which treatment is initiated.
The common, typical forms of retinitis pigmentosa have now yielded to treatment. Patients with typical retinitis pigmentosa have retinal arteriolar narrowing, elevated final dark adaptation thresholds, reduced and delayed ERGs, and, in most cases, intraretinal bone spicule pigment around the periphery. In a randomized, controlled, double-masked trial among 601 patients ages 18 to 49, the course of retinal degeneration as monitored by the ERG was slower on average among patients taking a daily supplement of vitamin A palmitate, 15,000 IU/day than among those not on this dose. Furthermore, the course appeared to be significantly faster on average among patients taking a daily supplement of 400 IU/day of vitamin E than those not on this dose.61 Mean annual rates of decline of remaining 30-Hz cone ERG amplitude by treatment group are shown in Table 24-4 for all randomized patients (left) and for a subset with slightly higher initial cone ERG amplitudes (≥0.68 μV designated as the higher amplitude cohort) who could be followed with greater precision (right). Among a subset of 125 patients who could perform Goldmann visual field testing with great precision (i.e. ≤ 5% intervisit variability), those on vitamin A showed a significantly slower rate of decline of visual field than those in the control group.62 The optimal total intake of vitamin A palmitate in this study population appeared to be ∼18,000 IU/day (i.e., 3,000 IU of vitamin A in a regular diet and 15,000 IU/day of vitamin A as a supplement); higher intake did not provide greater benefit (Fig. 24-9). These findings have led to the recommendation that most adult patients with the common forms of retinitis pigmentosa should take a daily supplement of 15,000 IU of vitamin A in the palmitate form under the supervision of their ophthalmologist and avoid high-dose supplementation with vitamin E. For the average patient in the trial, it has been estimated that treatment with vitamin A could add 7 additional years of useful vision61; that is, the average patient with 1.3 μV of cone function who starts vitamin A at age 32 would retain useful vision until age 70 rather than age 63 if left untreated. For some patients with larger pretreatment ERGs, vitamin A supplementation could provide additional benefit.
Table 24-4. Mean Rates of Decline in Visual Function by Treatment Group Among Patients with the Typical Forms of Retinitis Pigmentosa Supplemented with Vitamins A and Ea | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vitamin A may provide its benefit through the rescue of remaining cones, thereby, explaining how one supplement can help patients with many different rod-specific gene defects. The daily intake of a vitamin A supplement may provide protection against possible transient decreases in serum retinol concentrations that may adversely affect photoreceptor function. With respect to vitamin E, it has been hypothesized that a daily dose of 400 IU may adversely affect the course of retinitis pigmentosa at least in part by inhibiting the absorption or transport of vitamin A because it was observed that the patients receiving vitamin E had slight but significant decreases in serum retinol concentration compared with those not receiving vitamin E.61
Because doses of≥ 25,000 IU/day or more of preformed vitamin A can be associated with liver disease when taken over the long term, patients should have a fasting serum vitamin A and liver function profile before starting this treatment and measures of these parameters annually thereafter while on this treatment. Beta-carotene, the precursor of vitamin A, is not predictably converted to preformed vitamin A (i.e., retinol) and therefore should not be considered as a substitute for vitamin A palmitate in the context of this treatment. Because of the risk of birth defects associated with high-dose vitamin A supplementation, women who are pregnant or planning to become pregnant should not take this supplement. Postmenopausal women and men over age 49 taking vitamin A should monitor their bone health because of the slight (0.5% to 1.0%) increased risk of hip fracture among patients who take vitamin A over the long term. Patients after renal transplant should not take high-dose vitamin A supplements because they have excessive renal reabsorption of vitamin A and are therefore more susceptible to toxicity. Patients taking chronic doxycycline should not take vitamin A because the combination has been associated with increased intracranial pressure. Among adults, doses of vitamin A palmitate less than 15,000 IU/day have not been shown to be therapeutic, and doses greater than 25,000 IU/day are potentially toxic over the long term. No toxic side effects have been observed in adults with retinitis pigmentosa in good general health on 15,000 IU/day of vitamin A who have been followed for up to 12 years.63
Because patients under age 18 were not included in this trial, no formal recommendation can be made for patients with retinitis pigmentosa under this age.61,62 However, with the agreement of the parents and pediatrician, if children are above the lower fifth percentile of weight for their height and gender and if liver function is normal, a trial of vitamin A palmitate 5000 IU/day can be considered for those age 6 to 10 years; 10,000 IU/day for those age 10 to 15 years; and 15,000 IU/day for those age 15 and over. A list of sources of vitamin A palmitate is maintained by the Foundation Fighting Blindness (www.fightblindness.org).
During the vitamin A and E trial, a subset of patients with higher red blood cell (RBC) docosahexaenoic acid (DHA) levels were found to have a significantly slower rate of progression of retinitis pigmentosa than a subset with lower RBC DHA levels. This prompted a second randomized, controlled, double-masked trial for 221 patients (age 18 to 55 years) with typical retinitis pigmentosa who were assigned to either 1,200 mg/day of DHA or to a group given control fatty acid capsules. All participants received vitamin A palmitate 15,000 IU/day. This trial showed that DHA supplementation 1,200 mg/day did not, on average, slow the course of this condition over 4 years, as monitored primarily by the Humphrey Field Analyzer (Carl Zeiss Meditec, Dublin, CA). This precludes any general recommendation of DHA supplementation for this condition.64
However, a subgroup analysis among 70 of these patients on vitamin A before entry in this trial and during the trial as well, but not on DHA supplementation, revealed that those eating ≥.2 g/day or more of omega-3–rich oily fish (i.e., equivalent to one or two 3-oz servings of oily fish per week) showed significantly (P = .02) less loss of central visual field sensitivity as monitored with the Humphrey Field Analyzer (total point score with a size V white target) than those eating <0.2 g/day (Table 24-5). This observation supports the additional recommendation that adults already taking vitamin A palmitate should also eat one to two 3-oz servings per week of omega-3–rich fish (i.e., salmon, tuna, mackerel, herring, or sardines), of which DHA is a major constituent.65 If patients cannot eat oily fish, they are advised to take 200 mg/day of DHA by capsule as a substitute, but they are reminded that the efficacy data are based on combining vitamin A palmitate with naturally oily fish.
Table 24-5. Annual Decline in Visual Field Sensitivity in the Control Group as a Function of Dietary ω-3 Fatty Acid Intake Among Patients on Vitamin A Before Entrya | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Three to 4 months after starting the omega-3–rich fish diet (i.e., to allow sufficient time for red blood cell turnover), patients should have a fasting RBC DHA as a measure of intraretinal DHA to see if the level is at least 4% of total RBC fatty acids, because this level has been associated with significant slowing of the condition as monitored by visual field sensitivity.65 RBC DHA levels are measured in only a few laboratories, a list of which is maintained on the Foundation Fighting Blindness web site. If the level is less than 4%, then the patient is not eating sufficient oily fish and should increase his or her intake by an additional serving per week; their RBC DHA should be rechecked in 3 to 4 months. Once the RBC DHA is at the level of 4% to 7% of total RBC fatty acids, it should be monitored annually along with fasting serum vitamin A and liver function. It has been estimated that the combination of vitamin A with an oily fish diet would, on average, provide a 60% to 70% slowing per year that would result in a total of almost 20 years of visual preservation for patients who start this regimen in their mid 30s; this should make it possible for many patients with retinitis pigmentosa to retain useful vision for their entire lives.65
This second trial also showed that adults starting vitamin A palmitate 15,000 IU/day for the first time should also be treated with DHA supplementation 1,200 mg/day for 2 years to shorten the interval for vitamin A to achieve its benefit. After 2 years, patients should continue the vitamin A palmitate, stop DHA capsules (because of a possible adverse effect of vitamin A plus high-dose DHA over the long term), and then eat one or two 3-oz servings per week of omega-3–rich fish. Some 3 to 4 months after stopping the DHA capsules, these patients should check their fasting RBC DHA level as described above.65 Sources of DHA capsules are also provided on the Foundation Fighting Blindness web site.
RETINITIS PIGMENTOSA ASSOCIATED WITH HEREDITARY ABETALIPOPROTEINEMIA
In 1950 Bassen and Kornzweig66 described an 18-year-old girl, born of first cousins, who had a malabsorption syndrome, a generalized retinal degeneration, a diffuse neuromuscular disease similar to Friedreich’s ataxia, and a peculiar crenation of the red blood cells, now called acanthocytosis.67,68 In 1958, low serum cholesterol (<50 mg/dL) was observed.69 Soon thereafter, an absence of low-density plasma lipoproteins or so-called ß-lipoproteins was found, and the term abetalipoproteinemia was assigned to this recessively inherited disorder.70,71,72 Other classes of lipoproteins have also been found to be abnormal.73
Patients with hereditary abetalipoproteinemia can assimilate fat into the intestinal mucosa, but a defect exists in its removal from this site because of the lack of chylomicra. Intestinal biopsies have revealed normal-sized villi filled with lipid droplets that are essentially triglycerides. Mutations in the gene encoding a microsomal triglyceride transfer protein have been found in patients with this condition.74 It appears that the liver and then the retina become depleted of vitamin A. Abnormal ERGs have been reported in a 15-month-old child75 and a 6-year-old patient76 in whom the fundi were still normal. The original case described by Bassen and Kornzweig showed multiple white dots in the early stages, but by age 31, the patient developed multiple areas of retinal pigment epithelial cell atrophy. In other cases, the typical intraretinal pigment associated with retinitis pigmentosa has been noted in the retinal periphery.
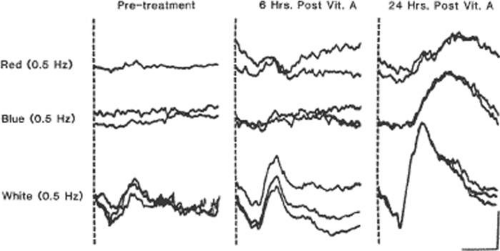
Patients with this condition are treated with a low-fat diet and supplements of the fat-soluble vitamins A, E, and K. Vitamin A supplementation has been shown to restore elevated dark adaptation thresholds and reduced ERG responses to normal in patients with the early stages (Fig. 24-10).77,78 More advanced cases have not responded: however, in one such case in which the retina was examined after the death of the patient, widespread loss of photoreceptor cells was observed.79 Vitamin A therapy may not maintain retinal function over the long term, because patients have been reported in whom vitamin A levels have been restored to normal and yet the retinal degeneration has appeared to progress.80,81 Because these patients have low serum vitamin E levels, supplementation with vitamin E in addition to vitamin A has been advocated, with reported stabilization or slowing of disease progression.82,83,84,85,86,87
RETINITIS PIGMENTOSA ASSOCIATED WITH REFSUM DISEASE
Refsum disease is a recessively inherited condition in which the patient accumulates exogenous phytanic acid.88,89 Findings include a peripheral neuropathy, ataxia, an increase in cerebrospinal fluid protein with a normal cell count, and retinitis pigmentosa. All have elevated serum phytanic acid. Some cases have anosmia, neurogenic impairment of hearing, electrocardiogram (EKG) abnormalities, and skin changes resembling ichthyosis. Patients show a granular fundus with areas of depigmentation around the periphery and have a subnormal ERG in the early stages or show more typical retinitis pigmentosa with a nondetectable ERG in more advances stages.90
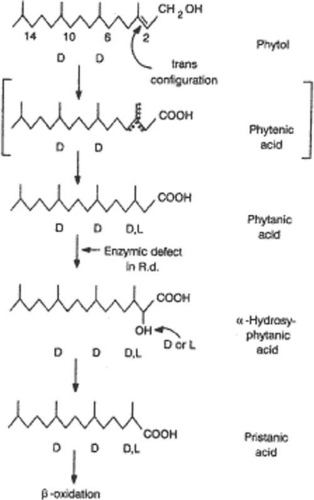
A defect exists in the conversion of phytanic acid to alpha-hydroxy phytanic acid, specifically in the introduction of a hydroxyl group on the alpha carbon of phytanic acid (Fig. 24-11).91 The pathogenesis appears to involve accumulation of phytanic acid in a variety of tissues, including the retinal pigment epithelium (RPE).92
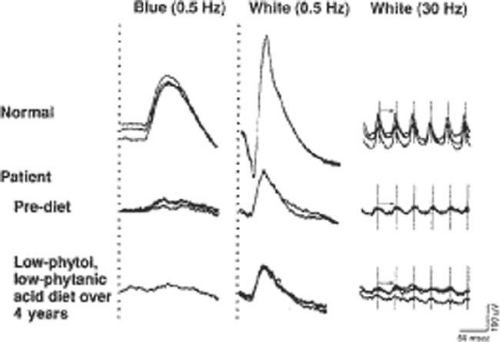
Treatment consists of restricting not only animal fats and milk products (i.e., foods that contain phytanic acid), but also green leafy vegetables containing phytol.93 Treatment success depends on the patient maintaining his or her body weight; if body weight becomes reduced, phytanic acid is released from tissue stores, resulting in an increase of phytanic acid in serum and exacerbation of symptoms. Refsum94 reported two patients whose serum phytanic acid levels were lowered to normal and who showed improvement in motor nerve conduction velocity, some relief of ataxia, and return of the cerebrospinal fluid protein to normal. Moreover, the retinitis pigmentosa and hearing impairment did not progress; one of these patients was followed for 10 years and the other for many years.94 One young adult with a mild form of this disorder has been followed on a low-phytol, low-phytanic acid diet for 4 years; full-field ERGs, reduced about 75% below normal before commencement of this diet, have remained about the same over this period (Fig. 24-12).42 Long-term effects of this diet on retinal function continue to be studied.
FAMILIAL ISOLATED VITAMIN E DEFICIENCY WITH RETINITIS PIGMENTOSA
Another rare recessively inherited form of ataxia associated with retinitis pigmentosa has been called familial isolated vitamin E deficiency. These patients present in adulthood with Friedreich-like ataxia, dysarthria, hyporeflexia, and decreased proprioceptive and vibratory sensation as well as markedly decreased serum vitamin E levels. In later stages, patients can develop the fundus changes of retinitis pigmentosa and abnormal ERGs. Molecular genetic analysis has revealed a mutation in the α-tocopherol-transfer protein (α-TTP) gene. Oral administration of vitamin E restored serum vitamin E levels to normal and appeared to halt or slow the progression of the neurologic abnormalities and retinitis pigmentosa in three patients followed for 1, 4, and 10 years, respectively.95,96
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree