Retinal Arterial Macroaneurysms
Neal H. Atebara
Retinal arterial macroaneurysms, first systematically studied by Robertson in 1973, are fusiform or saccular dilations of the retinal arteries, usually associated with systemic hypertension and atherosclerotic vascular disease. They may follow a benign clinical course, but if they leak fluid or hemorrhage, they can result in significant loss of central visual acuity. Management options depend on the nature of the exudative or hemorrhagic complications of the macroaneurysm. This chapter reviews the clinical presentation, pathophysiology, and management of retinal arteriolar macroaneurysms.
CLINICAL PRESENTATION
The typical patient who presents with a retinal arterial macroaneurysm is older than 60 year of age with a history of systemic hypertension and arteriosclerotic vascular disease. Women are affected three times more often than men.1,2 There may be a sudden loss of central or peripheral vision due to hemorrhage, a gradual blur in central visual acuity due to cystoid macular edema, or the macroaneurysm may be found ophthalmoscopically on a routine examination if there is no exudation or hemorrhage that encroaches upon the fovea. The incidence of retinal arterial macroaneurysms increases with age.
FUNDUSCOPIC APPEARANCE
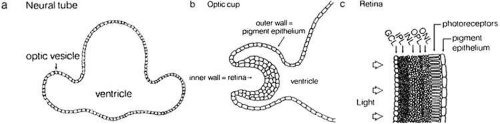
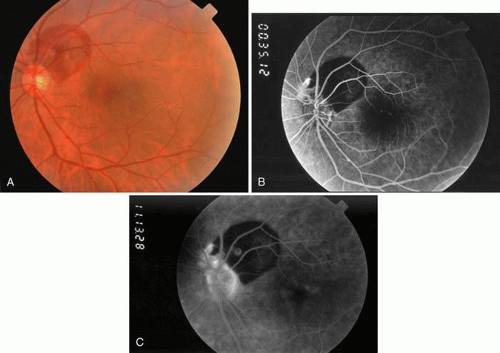
The hallmark for diagnosis of the retinal arterial macroaneurysm is visualization of the macroaneurysm itself (Fig. 1). Because of their relatively large size, macroaneurysms are not usually confused with the microaneurysms of diabetic retinopathy or branch retinal vein occlusion. Microaneurysms typically have a diameter of only 50 to 75 microns and arise from the deeper retinal capillaries; macroaneurysms on the other hand range in size from 100 to more than 500 microns in diameter and arise from the larger retinal arterioles.
Retinal arterial macroaneurysms usually arise within the first three orders of bifurcation from the optic disc (Fig. 2), often at a point of arteriovenus crossing. Sometimes they occur directly on the optic nerve head3 or on a cilioretinal artery.4 About 20% of affected eyes have multiple aneurysms, and about 10% demonstrate macroaneurysms in both eyes.
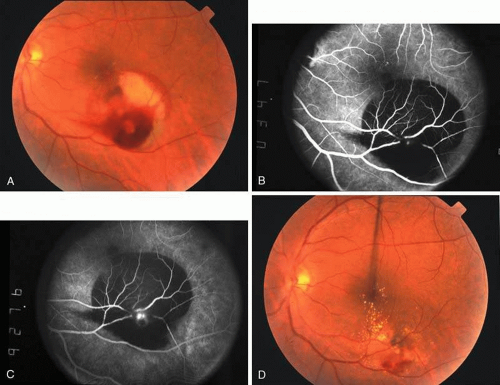
Retinal arterial macroaneurysms often produce retinal edema, circinate hard exudates, and hemorrhage (Fig. 3) into multiple layers of the retina: beneath the retinal pigment epithelium, beneath the retina, within the retina, beneath the internal limiting membrane, between the retina and the posterior hyaloid, and within the vitreous cavity. When the macroaneurysm is obscured by overlying blood, its diagnosis can be challenging.
FLUORESCEIN ANGIOGRAPHIC APPEARANCE
Because of rapid blood flow through retinal arterial macroaneurysms, they typically fill quickly in the early phase of the fluorescein angiogram. In the mid- and late-phases of the angiogram, the macroaneurysm tends to leak to varying degrees, depending on its perfusion and endothelial integrity (Fig. 3C). If there is subretinal fluid surrounding the aneurysm, there may be pooling of dye into the subretinal space. In some cases, a characteristic Z-shaped kink may be identified at the site of the aneurysm.
Perfusion abnormalities caused by the macroaneurysm cause changes in the surrounding retinal vasculature as well, and this is best visualized on fluorescein angiography (Fig. 3B). Ischemia from stagnation of blood flow results in capillary telangiectasis, microaneurysm formation, and capillary nonperfusion.
Some or all of these angiographic features may be obscured by blood or lipid exudation from the aneurysm. If blood collects in front of the retinal vessels (vitreous hemorrhage, preretinal hemorrhage, subinternal limiting membrane hemorrhage, or intraretinal hemorrhage), then blockage of hyperfluorescence may be partial or complete. Subretinal blood blocks hyperfluorescence from the choroid but not the retinal circulation, resulting in dramatically distinct retinal vessels against a dark background (Fig. 3B,C). Lipid exudation and retinal edema may cause partial blockage of hyperfluorescence.
PATHOPHYSIOLOGY
Chronic systemic hypertension is often seen in patients with retinal arterial macroaneurysms, and it is believed this condition has an important role in its pathogenesis. It is hypothesized that chronic vascular wall damage secondary to systemic hypertension and arteriosclerosis leads to focal dilation of the vascular wall, and this leads to macroaneurysm formation.5 There is no adventitia where arteries and veins cross, and this is a point at particular risk for aneurysm formation.
There is also evidence that retinal arterial macroaneurysms may be caused by focal damage to the blood vessel wall from conditions such as embolus,6 toxoplasmosis infection,7 or branch retinal vein occlusion.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree