and Yi Ning J. Strube2
(1)
Wright Foundation for Pediatric Ophthalmology and Adult Strabismus Medical Center, Los Angeles, CA, USA
(2)
Queen’s University, Kingston, Ontario, Canada
Keywords
Lost muscleSlipped musclePITSPulled in two syndromeStretched scarStrabismus after retinal detachment surgeryPearls for reoperationAmniotic membrane transplantMuscle dehiscenceFor most reoperations, standard recession and resection techniques can be used. The major difference from surgery on a virgin muscle is the need to mobilize the conjunctiva in front of and over the muscle. Reoperation for a lost muscle or for strabismus after retinal detachment surgery, however, tends to be technically more difficult and requires special techniques. This chapter covers surgical approaches to muscle dehiscence, lost muscle, and strabismus occurring after retinal detachment surgery.
21.1 Muscle Dehiscence: Lost Muscle, Slipped Muscle, and Stretched Scar
A muscle dehiscence is a separation of the muscle from its scleral attachment. Three basic types of muscle dehiscence have been identified: slipped muscle, lost muscle, and stretched scar. The medial rectus muscle is the most commonly slipped or lost rectus muscle, and is also the most difficult to find because it has no oblique muscle connections and it is free to retract posterior to the globe. The other rectus muscles have oblique muscle attachments that prevent them from retracting posterior to the globe: the superior rectus muscle to the superior oblique muscle, the lateral rectus muscle to the inferior oblique muscle, and the inferior rectus muscle to the inferior oblique muscle. In cases of slipped rectus muscles (or even most lost rectus muscles), there is usually a pseudotendon or fibrous scar from the previous scleral insertion site back to the slipped or lost muscle.
21.1.1 Slipped Muscle
First described by Parks and Bloom [1] in 1979, the slipped muscle occurs after inadequate suturing of muscle: the muscle capsule is attached to sclera, but the muscle itself retracts posteriorly. Ductions are limited but relatively preserved, as compared with a lost muscle (Fig. 21.1a). Plager and Parks [2] described the crucial finding of the muscle recoiled posteriorly within the capsule, found at the Tenon’s capsule penetration site. They also described specific intraoperative findings of a translucent, “empty, friable avascular capsule attached to the globe” (Fig. 21.1b). A slipped muscle occurs immediately, with limited ductions usually identified within a day or two after strabismus surgery, but the slippage can continue over time. Treatment is retrieval, excision of the capsule attachment, and advancement of the muscle to the intended surgical site with a nonabsorbable suture. Often the antagonist is contracted and tight, adding a restrictive component. If the antagonist is tight, it should be recessed.
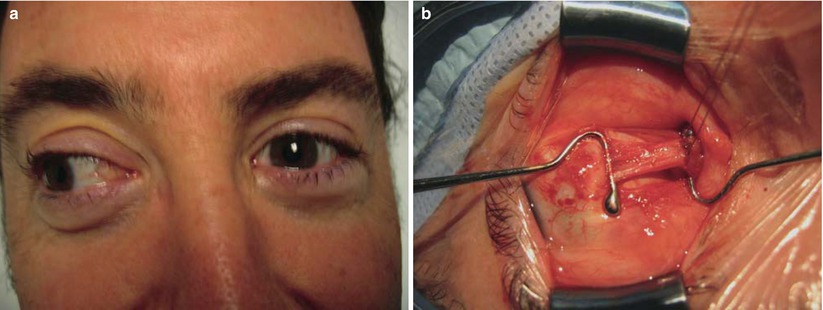
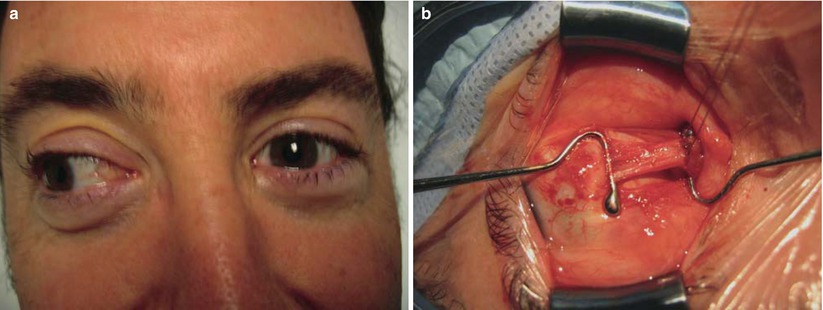
Fig. 21.1
(a) Patient with a slipped left medial rectus muscle after medial rectus recession. This patient is looking to the right, demonstrating a large exotropia with the left eye showing limited adduction and lid fissure widening. (b) Surgical exploration shows a translucent, avascular capsule connecting the globe to the medial rectus muscle. Note that the capsular attachment is so thin that the large Jameson hook can be seen through the overlying capsule
21.1.2 Lost Muscle
The lost muscle has long been a dreaded complication of periocular surgery, including pterygium surgery, retinal detachment surgery, and strabismus surgery. A lost rectus muscle can occur when a muscle is surgically removed from the globe, or it can be associated with the “Pulled in Two Syndrome” (PITS), when the muscle is torn in two by being pulled on too hard. PITS is more common in elderly patients, and can occur with relatively minimal muscle traction. The hallmark of a lost muscle is severely limited ductions and palpebral fissure widening on attempted gaze in the direction of the lost muscle. The treatment is exploration and retrieval of the lost muscle. If the muscle cannot be found immediately during the primary surgery, it is often best to wait 2 weeks to perform the secondary exploration surgery. By waiting to reoperate, the swelling subsides and a fibrous scar usually forms, which extends from the scleral insertion to the site of the lost muscle. This scar can be traced posteriorly to help find the lost muscle (see Figs. 21.2, 21.3, 21.4, 21.5, 21.6, 21.7, 21.8, and 21.9). Once the lost muscle is found, it should be secured and reattached with nonabsorbable suture. The antagonist to the lost muscle is usually contracted and tight. If such tightness is diagnosed tight by forced ductions, recess the tight antagonist. If the lost muscle cannot be found, a rectus muscle transposition is indicated, with a large recession of the antagonist muscle.
21.1.3 Stretched Scar
Stretched scar is a lengthening of the muscle-to-sclera fibrous attachment that occurs several weeks to months after strabismus surgery. The result is posterior retraction of the muscle and reduced muscle function. In 1999, Ludwig [3] first described this phenomenon as a common cause of unfavorable outcomes after strabismus surgery. Using an animal model, Ludwig showed that muscles sutured with an absorbable suture had a significantly higher rate of stretched scar than those sutured with a nonabsorbable suture. Ludwig hypothesized that the mechanism of stretched scar is weakening of the absorbable suture before the muscle-to-sclera healing is complete. As with slipped muscle, patients with stretched scar have an amorphous, fibrous band connecting the muscle to the globe, but the tissue is thicker with a stretched scar (see Figs. 21.10 and 21.11). Also similar to a slipped muscle, ductions are limited, but they are less limited than with a lost muscle. In contrast to a slipped muscle, which occurs immediately, stretched scar occurs late, at least 4–6 weeks after surgery. Treatment is excision of the scar and advancement using a nonabsorbable suture to secure the muscle to the intended insertion site (see Figs. 21.12, 21.13, and 21.14). Add a recession of the antagonist muscle if it is tight on forced duction testing.
21.2 Surgery for a Lost Medial Rectus Muscle
Figures 21.2, 21.3, 21.4, 21.5, 21.6, 21.7, 21.8, and 21.9 show the surgical approach to a lost left medial rectus muscle. The senior author (KWW) has developed a conjunctival incision that is a combination of the fornix and Swan incisions. This incision allows immediate access to the posterior aspect of the quadrant between the muscles to allow hooking of the muscle or its scar, and great exposure of the area over the muscle. This incision also avoids having to mobilize the bulbar conjunctiva in front of the muscle, which is usually scarred to sclera. The postoperative appearance of the conjunctiva is quite good with this technique.
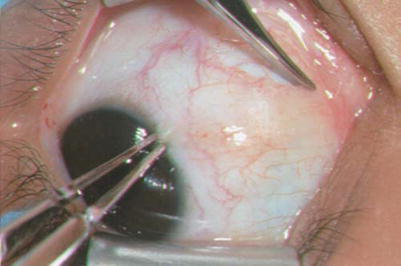
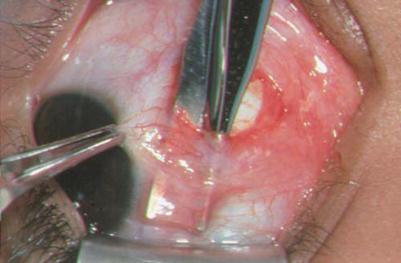
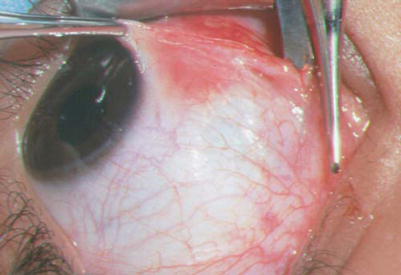

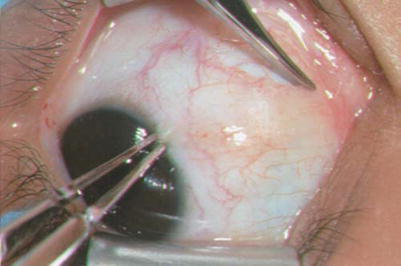
Fig. 21.2
A blunt curved Westcott scissors is used to make an incision in the inferior nasal fornix through conjunctiva. After the conjunctival incision, use the Westcott scissors and spread into the inferior nasal quadrant, keeping the scissors tips down on sclera to remove adhesions to sclera. The conjunctiva may be adherent to sclera, requiring blunt and sharp dissection to mobilize the conjunctiva
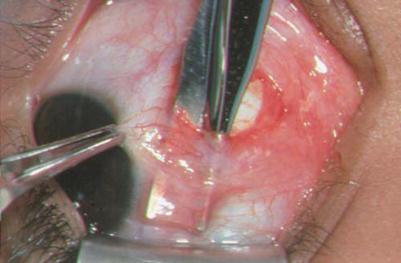
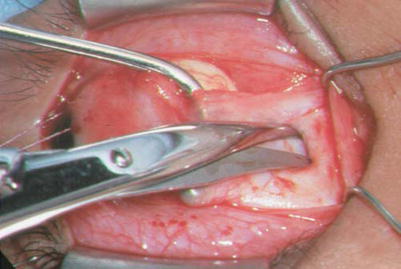
Fig. 21.3
After the quadrant is open and free of adhesions, undermine the conjunctiva in front of the area of the medial rectus insertion site by spreading the blunt Westcott scissors as shown. Firm conjunctival-scleral adhesions are removed with sharp dissection, staying close to sclera
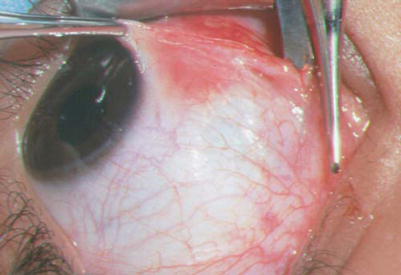
Fig. 21.4
Once the conjunctiva anterior to the original muscle insertion is mobilized, perform a Swan incision by extending the conjunctival incision superiorly over the area of the muscle insertion as shown. Be sure to keep the incision in front of the plica and semilunar folds

Fig. 21.5
Secure the muscle (or muscle scar) by passing a small hook in the inferior nasal quadrant, orienting the hook perpendicular on bare sclera, and then passing the hook underneath the tissue where the medial rectus muscle insertion should be, based on the previous surgery. This pass of the small Stevens hook should be made at least 5 mm posterior to the presumed insertion site. Once tissue is hooked with the small Stevens hook, pass a von Graefe hook behind the small hook, and then remove the small hook. The von Graefe hook has a smooth end (no foot or bulb), so it is easier to pass under a scarred muscle than a Green or Jameson hook. The photograph shows the von Graefe hook behind a fibrovascular tissue that could possibly be the muscle or a scar to the slipped muscle. (A scar that connects and attaches sclera to a slipped muscle is termed a “pseudotendon.”) Note that in this photograph, a Vicryl traction suture has been placed at the limbus, pulling the eye out laterally to aid with exposure. Be sure not to pull too hard on the von Graefe hook, as the pseudotendon can rupture