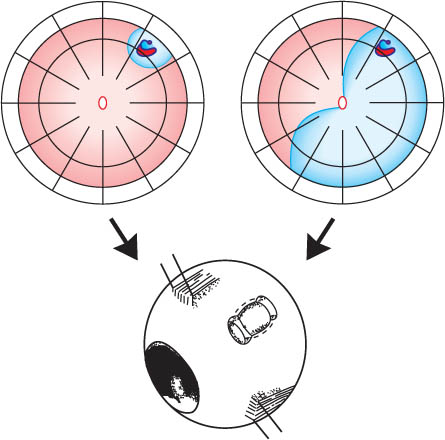
14 Reoperation of Retinal Detachments without Drainage: Minimal Extraocular Surgery as Rational Approach As will be recalled, the treatment of a primary retinal detachment consists of searching the break and closing it ab externo by localized buckling without drainage of subretinal fluid. As a consequence, a cerclage, pneumatic retinopexy, or a vitrectomy are avoided as primary procedures. – Therefore, as in a primary detachment, you have to search for the cause of this detachment, i.e., the retinal break (see Part 1, Chapter 2.2, pp. 13–18). – It has to be tiny, because otherwise it would not have been overlooked at the 1st operation. Then this break can be treated in the same way as if it were in a primary detachment. Now you might recall the logo of our Detachment Course (Fig. 14.1) and the rationale behind it concerning treatment of a retinal detachment. Fig. 14.1 Minimal extraocular buckling surgery: The treatment is limited to the area of the break and not determined by the extent of the detachment. The small (Top left) and the more extensive detachment (Top right) are caused by the same horseshoe tear at 1 o’clock. The treatment of both is the same, consisting of buckling the tear either by a radial sponge or temporary balloon without drainage of subretinal fluid. Consequently, the treatment of a surgical failure can also imply a rational approach representing a small procedure. To obtain a better insight into the development of reoperations, let us review the sequence of procedures that have evolved over the last 40 years as presented in a publication by Lincoff and Kreissig [2]. Scleral buckling was the most frequent surgery for a primary retinal detachment. If the 1st buckle was a segmental, the 2nd operation after a failed procedure was a larger segmental buckle. If this failed, the 3rd operation was a cerclage and if this failed too, the 4th operation was another circular band, but this time more posterior and more constricting. The 2 encirclements, combined with 360° of coagulation, represented the limit of reoperations in those years. Therefore, “creating a new ora serrata” became current and the described reoperations had become a routine series of procedures, representing an automatic sequence. However, in the meantime, the techniques for retinal examination became more precise and the concession of not finding the hole was no longer valid. The availability of binocular indirect ophthalmoscopy and biomicroscopy with direct and indirect contact lenses, combined with simultaneous depression, made the retina visible up to the ora serrata. Since the advent of vitrectomy [3] and the long-acting gases [4,5] in 1970, the vitreous has no longer been inviolate, and a new automatic sequence of procedures for reoperation has evolved. The 1st operation is a gas injection into the vitreous and, if this fails, the 2nd operation is a vitrectomy. The described sequence of reoperations has become automatic. As a consequence, the patients who are referred for reoperation have mostly already had a gas injection and are being referred for a vitrectomy. The thought which occured to us, and probably to you as well, is therefore: – Which type of repair will represent a rational approach? – Has reoperation to be a maximal procedure per se? A total of 752 detachments were treated with segmental buckling and without drainage [6]. In this series giant tears and perforating injuries were excluded. The detachments were caused by 1 to 3 breaks or a tear with a maximal extension of 1 clock hour. Actually they were relatively uncomplicated detachments and represented 8 out of 10 detachments that the average retinal surgeon might have to repair.
14.1 Introduction
 However, what should be done if the retina does not reattach after external buckling, i.e., after segmental buckling or even after a cerclage?
However, what should be done if the retina does not reattach after external buckling, i.e., after segmental buckling or even after a cerclage?
 Is there now an indication for an intraocular approach as repair, such as a gas injection or a vitrectomy with gas or silicone oil?
Is there now an indication for an intraocular approach as repair, such as a gas injection or a vitrectomy with gas or silicone oil?
 At this point you should recall the greater morbidity of these alternatives (see Chapter 13, pp. 299–308).
At this point you should recall the greater morbidity of these alternatives (see Chapter 13, pp. 299–308).
 Why not aim first at a minimal and extraocular approach—in spite of being confronted with a reoperation?
Why not aim first at a minimal and extraocular approach—in spite of being confronted with a reoperation?
For example, a procedure the rationale of which you are already familiar with?
 Let me provide for you some facts [1].
Let me provide for you some facts [1].
 – To begin with, analyze the borders and surface of the surgical failure and determine whether it is a rhegmatogenous detachment. This is the situation, if the detachment has convex borders and surface.
– To begin with, analyze the borders and surface of the surgical failure and determine whether it is a rhegmatogenous detachment. This is the situation, if the detachment has convex borders and surface.
 Therefore, also in a detachment being up for reoperation you will look for the break, because then it will become feasible to limit the treatment to the area of the break, i.e., not extending it over the entire extent of the detachment.
Therefore, also in a detachment being up for reoperation you will look for the break, because then it will become feasible to limit the treatment to the area of the break, i.e., not extending it over the entire extent of the detachment.
14.2 History
 From 1960 to 1970
From 1960 to 1970
 What was the rationale behind the sequence of reoperations between 1960 and 1970?
What was the rationale behind the sequence of reoperations between 1960 and 1970?
 To wall away undetected retinal breaks in the periphery that were presumed to be leaking.
To wall away undetected retinal breaks in the periphery that were presumed to be leaking.
 As a consequence questionable holes in the retinal periphery could no longer be a reason for applying a prospective cerclage.
As a consequence questionable holes in the retinal periphery could no longer be a reason for applying a prospective cerclage.
 After 1970 to 2000
After 1970 to 2000
 But what is the rationale behind the new sequence of reoperations after 1970 and up to 2000?
But what is the rationale behind the new sequence of reoperations after 1970 and up to 2000?
 This time the failure is supposed to be due to vitreous traction and an intraocular tamponade of gas or, if gas fails, a vitrectomy should overcome it.
This time the failure is supposed to be due to vitreous traction and an intraocular tamponade of gas or, if gas fails, a vitrectomy should overcome it.
 Where does the cause of a surgical failure lie?
Where does the cause of a surgical failure lie?
Within the retina or within the vitreous?
 To answer this question, the causes for failure were analyzed in a series of detachments.
To answer this question, the causes for failure were analyzed in a series of detachments.
 At the same time 2 questions, often posed, should be answered:
At the same time 2 questions, often posed, should be answered:
14.3 Patients and Methods
| n | % |
Another break | 39 | 5 |
Inadequate buckle | 27 | 4 |
“It must be traction“ | 17 | 2 |
Choroidals | 3 |
|
Removal of buckle | 1 |
|
Total | 87 |
|
After buckling, 87 retinas had failed to reattach. This was due to an overlooked break in 39 eyes (5%), an inadequate buckle in 27 (4%), and “it must be traction” in 17 eyes (2%) (Table 14.1).
If we now consider these 87 surgical failures alone, then
 76% of failures were due to an iatrogenic error
76% of failures were due to an iatrogenic error
(Table 14.2):
What does this imply?
 45% (39/87) were caused by another break.
45% (39/87) were caused by another break.
31% (27/87) were caused by an inadequate buckle.
Only in 17 of the 87 eyes we were unable to find out the reason for failure. Therefore, it was suggested the term “it must be traction.” In the light of this, the secondary cerclage of the 60’s and 70’s, that aimed at undetected breaks, was more pertinent and not so wrong. But, applying a cerclage conceded that the break could not be found, a concession that is nowadays no longer valid with the availability of the improved spectrum of diagnostic techniques (see Part 1, Chapter 2, pp. 8–25).
We should realize, at the same time, that the above findings imply the following:
 In about 8 out of 10 eyes being up for reoperation, the cause of failure lies in:
In about 8 out of 10 eyes being up for reoperation, the cause of failure lies in:
An undetected break or a leaking break on a buckle. What is the consequence of this with respect to reoperation?
| n | % |
Another break | 39 | 44.8 |
Inadequate buckle | 27 | 31.0 |
“It must be traction“ | 17 | 19.5 |
Choroidals | 3 |
|
Removal of buckle | 1 |
|
Total | 87 |
|
 You should:
You should:
– Determine the contour of the surgical failure.
– Compare it with the contour of the detachment prior to surgery.
– Search for an undetected break in the most likely area as defined by the pattern of the detachment up for reoperation [1, 2, 7].
14.4 Results
14.4.1 First Category of Surgical Failure: An Undetected Break. The 4 Rules to Find the Undetected Break in Reoperation
When the 1st category of failure, i.e., an undetected break, was examined, 4 patterns could be defined [2].
To begin with, here is an important finding which was made.
 The buckle operation that failed can provide a clue for finding the undetected break: What does this mean?
The buckle operation that failed can provide a clue for finding the undetected break: What does this mean?
 There has been:
There has been:
– Either a change in borders of the detachment
– Or not.
As you will see, both circumstances are valid to find the undetected break.
 1st pattern of surgical failure due to an undetected break
1st pattern of surgical failure due to an undetected break
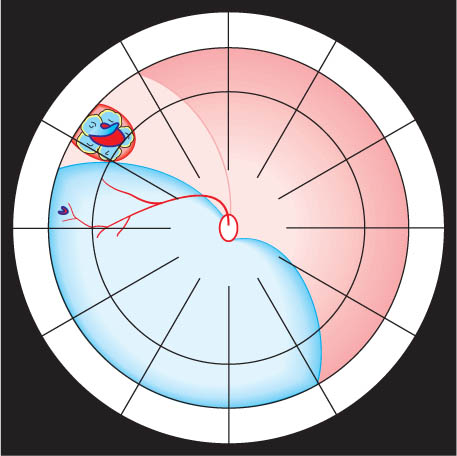
Here a detachment is shown with a horseshoe tear at 10:15, which responded incompletely to a buckle beneath the break (Fig. 14.2a).
 The superior border of the detachment had dropped from 11 o’clock to 9:45:
The superior border of the detachment had dropped from 11 o’clock to 9:45:
The inferior border had remained unchanged, indicating that the remaining fluid was not residual, but was there to stay because of another break within 1½ clock hours of the new superior border, located inferior to the buckle.
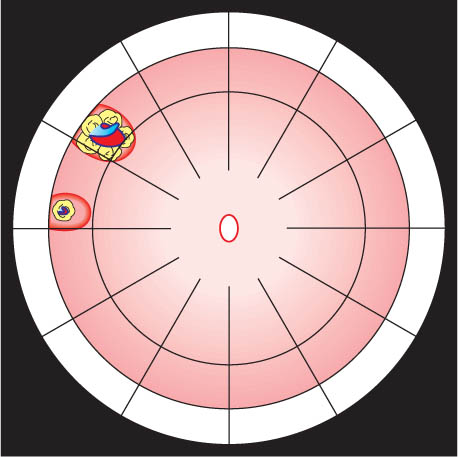
For your recollection, Rule 1 of how to find the primary break in a primary detachment of this type is presented in Figure 14.2b. Bio-microscopic examination directed at this area in the detachment up for reoperation, depicted in Fig. 14.2a, detected a small tear at 9:15, that was undetected at the 1st operation. The hole was too small to be seen by indirect ophthalmoscopy. For this reason, the vessel pattern around it was drawn at the biomicroscope so that we could localize this area at the operating table. Of course the break was smaller than depicted in Figure 14.2a. However, it should be borne in mind that when performing the reoperation, you may not find the tiny break with indirect ophthalmoscopy, but the area in which it is localized, as defined by the adjacent vessel pattern or any other retinal clue. Therefore, it is appropriate to buckle this area. When the next day the retina was reattached without drainage, it implied that the hole was buckled effectively (Fig. 14.2c).
 But what might you still have to do?
But what might you still have to do?
 If you have not cryopexied the break, you will have to apply laser lesions to the buckle postoperatively to secure the break.
If you have not cryopexied the break, you will have to apply laser lesions to the buckle postoperatively to secure the break.
Fig. 14.2 1st pattern of surgical failure due to an undetected break. a A superior lateral detachment 1 day after a radial buckle was placed to close a horseshoe tear at 10:15: The upper border of the detachment had dropped from 11:00 to 9:45, the inferior border had remained unchanged. The remaining detachment had a rhegmatogenous convex contour and extended from ora to disk. Another hole had to be present. The conclusion reached was to search for it within the area 1½ clock hours beneath the new superior border which is inferior to the buckle. A tiny horseshoe tear—depicted larger with a surrounding vessel—was found at 9:15. This location of the hole fitted Rule 1 of how to find the primary break in a detachment (see Fig. 14.2b).
Fig. 14.2b Rule 1 for Primary Break in a Detachment.
Superior temporal or nasal detachments: In 98% the primary break lies within 1½ clock hours of the higher border.
This was the 1st category of surgical failure due to an undetected break, which permits the following conclusion:
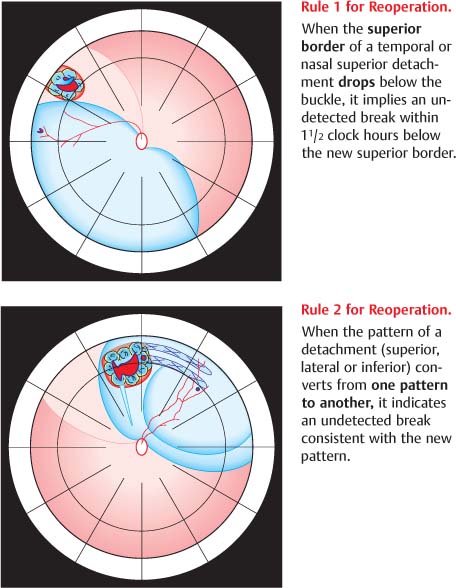
Reoperation | Rule 1 |
When the superior border of a temporal or nasal superior detachment drops below the buckle, it implies an undetected break within 1½ clock hours below the new superior border (Fig. 14.3a).
Fig. 14.2c After buckling the break at 9:15 (overlooked in the detachment depicted in Fig. 14.2a), the retina was reattached the next day: During surgery the area of the break was only found by the documented vessels and the tiny horseshoe tear detected after cryopexy of this area. The cryopexy lesion was pigmented 8 days after surgery.
Fig. 14.3a Rules 1 and 2: How to find the undetected break in reoperation of a retinal detachment.
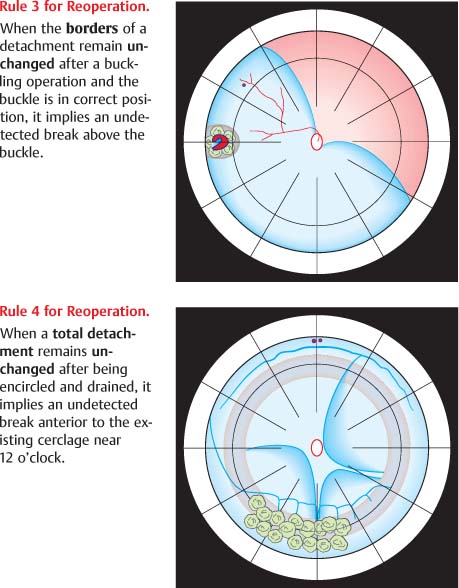
Fig. 14. 3b Rules 3 and 4: How to find the undetected break in reoperation of a retinal detachment.
 2nd pattern of surgical failure due to an undetected break
2nd pattern of surgical failure due to an undetected break
Here you see an acute superior bullous detachment distributed on both sides of the 12 o’clock meridian. It was apparently secondary to the small hole at 12 o’clock and the larger tear temporal to it (Fig. 14.4a). Both tears fitted Rule 2 of how to find the break in a primary detachment (Fig. 14.4b). In this situation it means that the 2 identified holes are within 1½ clock hours on either side of 12 o’clock. The retina is almost symmetrically detached on both sides. If you allowed this detachment patient to go home without double patching, this would become a total detachment just by these 2 breaks alone. Consequently, these breaks were buckled on a large radial sponge and the next day the detachment looked about the same. After 2 additional days you can recognize the minor change that is going on: There is a slight change around 11 o’clock which is hardly perceptible.
 But something else has happened, i.e., to the pattern of the detachment:
But something else has happened, i.e., to the pattern of the detachment:
– Suddenly it starts to descend further on the 1 o’clock side, but on the 11 o’clock side the border of the detachment has slightly ascended.
– In addition, the bullous quality at the 12 o’clock area has diminished, but increased on the 1 o’clock side (Fig. 14.4c).