Pupil
BASICS
ANATOMY
The pupil receives both sympathetic and parasympathetic innervation. The sympathetic input dilates the pupil and the parasympathetic input constricts it. Therefore, a sympathetic paresis will produce pupillary miosis while a parasympathetic paresis will cause mydriasis.
SYMPATHETIC SYSTEM
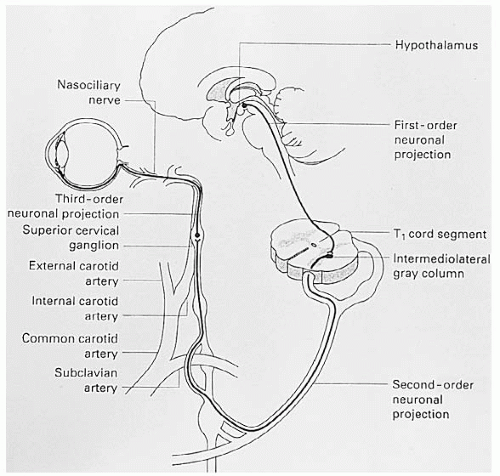
The sympathetic innervation of the pupil is a three-neuron chain that begins in the posterior hypothalamus with the first-order neuron that extends down through the brainstem to the spinal cord and synapses at the ciliospinal center of Budge (C8-T2 level) (Fig. 12-1). In the midbrain the sympathetic pathway runs close to the cranial nerve (CN) IV nucleus. The second-order neuron leaves the spinal cord and enters the paravertebral sympathetic chain ascending in the abdomen and thorax to come into contact with the apex of the lung, and in the neck it is associated with the carotid artery. At the angle of the jaw, it synapses in the superior cervical ganglion from which the third-order neuron originates. The first and second order neurons are also known as preganglionic; the third order neuron is termed postganglionic. It ascends within the adventitia of the internal carotid artery to enter the skull. It then travels through the cavernous sinus where it is in close association with CN VI and joins the ophthalmic division of CN V to enter the orbit. The oculosympathetic fibers innervate the iris dilator muscle, Muller muscles, and inferior tarsal muscle. The sympathetic fibers are responsible for facial sweating and vasodilation following the external carotid artery branching off at the superior cervical ganglion.
Any abnormality along this three-neuron chain produces Horner syndrome that consists of relative ipsilateral pupillary miosis, upper lid ptosis, and lower lid elevation (Fig. 12-2).
PARASYMPATHETIC SYSTEM
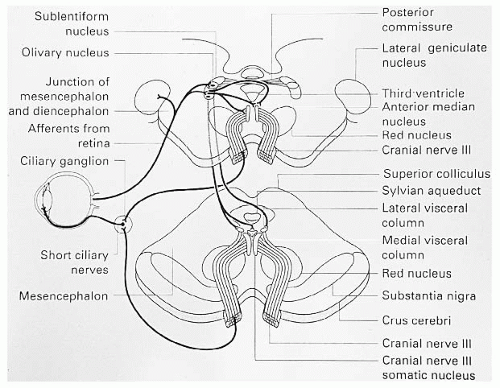
The parasympathetic system (Fig. 12-3) begins at the retinal ganglion cells with the fibers destined to innervate the pupil
coursing with the visual fibers. The pupillomotor fibers leave this pathway before the lateral geniculate body is reached via the brachium of the superior colliculus to reach the pretectal area. Both pretectal nuclei receive input from both eyes via intercalated neurons. Each pretectal nucleus sends axons to both Edinger-Westphal nuclei. Parasympathetic efferent fibers leave the Edinger-Westphal nucleus and are incorporated into CN III to the ipsilateral ciliary ganglion within the orbit. The postganglionic fibers innervate the iris sphincter muscle for pupillary constriction and the ciliary muscle for accommodation. The proportion of fibers to the iris sphincter to the ciliary muscle is 30:1. Acetylcholine released at the neuromuscular junction of the iris sphincter results in pupillary constriction, and an abnormality of the efferent parasympathetic input to the iris results in pupillary mydriasis.
coursing with the visual fibers. The pupillomotor fibers leave this pathway before the lateral geniculate body is reached via the brachium of the superior colliculus to reach the pretectal area. Both pretectal nuclei receive input from both eyes via intercalated neurons. Each pretectal nucleus sends axons to both Edinger-Westphal nuclei. Parasympathetic efferent fibers leave the Edinger-Westphal nucleus and are incorporated into CN III to the ipsilateral ciliary ganglion within the orbit. The postganglionic fibers innervate the iris sphincter muscle for pupillary constriction and the ciliary muscle for accommodation. The proportion of fibers to the iris sphincter to the ciliary muscle is 30:1. Acetylcholine released at the neuromuscular junction of the iris sphincter results in pupillary constriction, and an abnormality of the efferent parasympathetic input to the iris results in pupillary mydriasis.
Pupillary constriction to a near stimulus (nearreflex) bypasses the pretectal nuclei in the dorsal midbrain and descends directly to the area of the Edinger-Westphal nuclei from higher cortical centers. Hence, in light near dissociation the dorsal midbrain and pretectum are damaged, but the near-reflex pathway and Edinger-Westphal nuclei are not damaged.
EXAMINATION TECHNIQUES
Examination of the pupil is an integral part of the ophthalmologic examination.
The technique of pupillary examination is as follows:
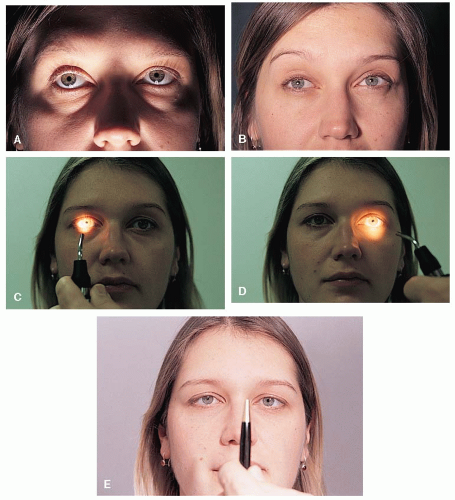
The pupillary size of each eye is determined first in a dimly lit room with the patient fixating a distant target. The pupils are diffusely illuminated from below (Fig. 12-4A). The pupillary size is examined in bright light by turning on the examination room lights (Fig. 12-4B) or by using either a halogen muscle light or indirect ophthalmoscope turned up to its highest brightness level.
Reactivity of each pupil is tested in a dimly lit room with the patient fixing on a distance target. A bright light is shone in each eye and the briskness of the pupillary reactions is recorded (Fig. 12-4C and D).
The swinging light test is then performed looking for the presence of a relative afferent pupillary defect (RAPD) (see Chapter 1).
The pupillary near response is tested by having the patient fix on a target at near (approximately 12 inches or 30 cm) while the pupils are diffusely illuminated (Fig. 12-4E). Effort is an important aspect of this test so if convergence does not occur, it is difficult to tell if the problem is pathologic or effort related.
Slit-lamp assessment of iris and pharmacologic testing is carried out in specific instances (see sections, Adie (Tonic) Pupil, Mydriasis, Horner Syndrome).
PUPILLARY SIZE
Under normal circumstances, the pupils are equal in size, although some people have smaller pupils (particularly older patients) and some have larger pupils (particularly younger, anxious patients). Therefore, anisocoria, that is, a difference in size between the two pupils, must always be suspected of being potentially a pathologic finding. Not all anisocoria, however, is pathologic. Physiologic anisocoria (Fig. 12-5) is seen in approximately 10% to 20% of the patients. To determine if anisocoria is physiologic, as opposed to being due to a pathologic process, the pupillary size is determined as just described in both bright and dim illumination. In physiologic anisocoria, the degree of anisocoria between the pupils is relatively the same in both illumination levels. For example, if there is a 30% difference in pupillary size in dim light,
a 30% difference also will be present in bright light. Any change in the degree of the anisocoria in bright and dim light indicates pathologic anisocoria.
a 30% difference also will be present in bright light. Any change in the degree of the anisocoria in bright and dim light indicates pathologic anisocoria.
Pathologic anisocoria can be due to an abnormality of either the sympathetic or the parasympathetic pathway. If the anisocoria is greater in dim light, the abnormal pupil is the smaller one and a sympathetic paresis should be suspected. The most likely manifestation of this sympathetic paresis is Horner syndrome, which is usually accompanied by ptosis (Fig. 12-6).
If the anisocoria is greater in bright light, the abnormal pupil is the larger one, which does not constrict normally. There are a number of causes for this, including abnormalities in the pupillary parasympathetic innervational system. Adie pupil and a parasympathetic paresis due to CN III palsy are the most likely causes of a parasympathetic abnormality. Likewise, pharmacologic blockade of one pupil will produce anisocoria that is greater in bright light (Fig. 12-7). In this condition, the larger pupil is of greater diameter than produced in other neuro-ophthalmic causes of anisocoria.
In any patient who has anisocoria, it is critical to examine
• the lids and
• ocular motility
This will enable the physician to identify the more important causes of anisocoria, that is, Horner syndrome and CN III palsy.
REACTIVITY OF THE PUPIL
Even in the presence of isocoria (pupils of equal size), pupillary reactivity should be assessed. The pupils may be abnormal in reactivity and yet be of equal size. Such abnormalities are usually due to parasympathetic disorders and may be seen in the Guillain-Barré syndrome, dorsal midbrain syndrome, or botulism. Adie pupil, which has a tendency to become bilateral, may also produce bilateral poorly reactive pupils that at times may be isochoric.
RELATIVE AFFERENT PUPILLARY DEFECT
At this point the patient is examined for the presence of a RAPD. The method of examination and its significance is outlined in Chapter 1.
NEAR RESPONSE
Testing for the near response is not performed routinely but is important to document in specific clinical situations, usually to detect light-near dissociation. This pupillary disconnect, where the pupil does not react to light but does to near, is seen in Adie pupil, Argyll Robertson (AR) pupils, and in the dorsal midbrain syndrome among others.
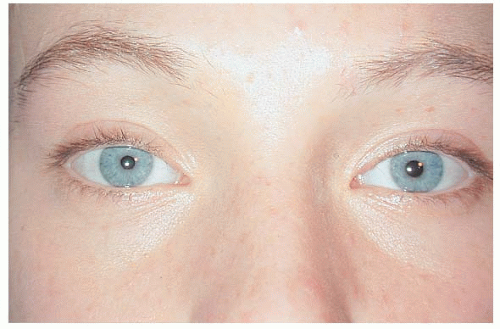 FIGURE 12-2. The patient has right upper lid ptosis with the right pupil being smaller than the left. The right lower lid is elevated compared to the left. |
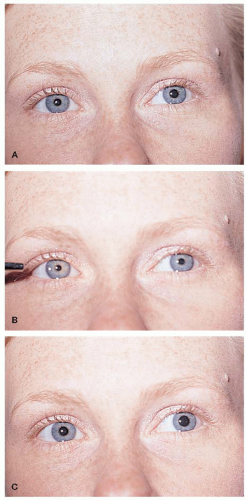 FIGURE 12-5. Physiologic Anisocoria. The left pupil is larger than the right in ambient light (A). The degree of anisocoria is the same in bright (B) and dim illumination (C). |
 FIGURE 12-6. Anisocoria is more prominent in dim illumination (Top photo), indicating the smaller pupil is abnormal. |