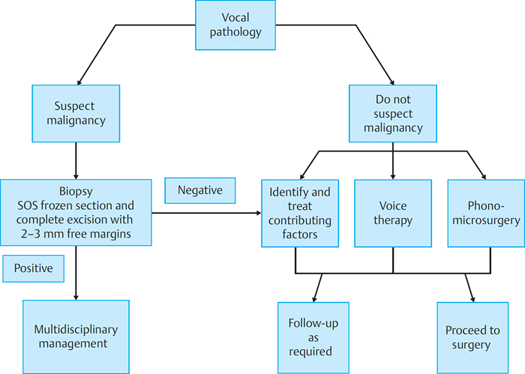
13 Principles of Phonomicrosurgery Phonomicrosurgery is performed endoscopically using a microscope on the vocal folds to restore, improve, or alter a person’s voice and may also be performed in both benign and select malignant laryngeal pathology. A successful surgery is underpinned by a sound knowledge of the anatomy, particularly microanatomy of the vocal folds and understanding of the physiological principles of phonation. Hirano has described the vocal folds as a multilayered structure comprising stratified squamous epithelium overlying a gelatinous superficial lamina propria (SLP) and together comprising the vocal fold cover. This is followed by the intermediate and deep layers of the lamina propria, which constitute the vocal ligament. This vocal ligament serves as a transition layer to the body of the vocal fold composed of the most medial part of the thyroarytenoid muscle, i.e., vocalis muscle.1 The epithelium is secured to the lamina propria by the basement membrane zone (BMZ), which is a collection of protein and nonprotein structures. The basal cells of the BMZ have anchorage filaments and fibers that attach themselves to the lamellar proteins in the lamina propria. Thus, the cellular epidermis is attached to gelatinous lamina propria. Interestingly, fewer anchoring fibers per unit area predispose to vocal nodules.2,3 When cancer has not infiltrated into the BMZ, it is referred to as carcinoma in situ, and chances of local or distal metastasis are highly unlikely. It is consequently essential to dissect below the BMZ when performing a biopsy of a suspicious vocal fold lesion to enable the histopathology experts to make a correct diagnosis regarding depth of invasion of the cancer. The SLP is composed of a loose fibrous tissue network in an extracellular matrix of hyaluronic acid, mucopolysaccharides, decorin, and other proteins. Although the SLP is also known as Reinke space, it is not a space, but a potential space due to the loose arrangement of its integral components. This structure affords the flexibility required for complex vibrations by the vocal fold during vocalization. The intermediate lamina propria acts as a shock-absorbing layer, especially at its anterior and posterior condensation referred to as anterior and posterior macula flava, hence its structure is predominantly made of elastin and hyaluronic acid arranged in a regular longitudinal manner. The deep layer of the lamina propria comprises fibroblasts and collagen. Respect for these different layers and an appreciation of their contribution to the vocal fold function is essential before undertaking phonomicrosurgery. Not only is the SLP integral to the vibratory characteristics of the vocal fold, but it also has a poor propensity toward regeneration following excision or thermal damage and therefore must be handled with care and preserved to ensure optimal healing with minimal scarring and distortion to the mucosal wave. Clinical Insight The superficial lamina propria (SLP) layer is vital for production of the mucosal wave and cannot regenerate; therefore, handle this layer with care while preserving as much normal epithelium as possible. Infiltration of the subepithelial space with 1 to 2 cc of 1: 10,000 of adrenaline in saline before surgery permits expansion of the SLP, although temporarily, allowing for dissection in the most superficial part of the SLP. Subepithelial infiltration technique (SEIT) also helps achieve hemostasis, lesion demarcation, and estimation of depth penetration of the vocal fold lesion.4 A safe approach during vocal fold surgery is to use mini-micro flaps with clean incisions through the epithelium and a gentle dissection through the SLP to excise the pathological lesion.5 Removal of the lesion is then performed by staying in the SLP as superficial as possible. It is important to avoid trauma to the vocal ligament whenever possible because the vocal ligament is a source of fibroblasts that are activated during the postoperative recovery phase. The vocalis muscle should not be routinely instrumented during phonomicrosurgery, as benign lesions are mostly located in the most superficial layers of the vocal fold. Before operating on the vocal folds, it must be established that there is a pathological lesion causing a change in voice. Conservative management, when indicated, must be instituted before planning for surgery. Phonomicrosurgery is indicated when a lesion is present on the vocal folds, which has a detrimental effect on the voice. Lesions such as large hemorrhagic polyps, Reinke edema, and intracordal cysts are most amenable to surgery. However, some lesions may not present such a clear case for excision, such as vocal fold sulci where surgical results are unpredictable and soft vocal nodules before exposure to the benefit of speech therapy. The potential risk of scarring and causing more damage to the voice must be borne in mind during the decision-making process before phonomicrosurgery. Lesions that will not respond, have not responded, or indeed have worsened in response to voice therapy make a strong case for surgery, as do cases of suspected malignancy. A decision-making algorithm highlighting the key steps in the management of vocal pathology is outlined in Fig. 13.1. A patient’s goals and desires must be considered before surgery. A patient with hoarseness may be anxious to exclude a cancer diagnosis with no desire for surgery once there is reassurance that the lesion is benign. Conversely, a patient who is a professional voice user may wish for expedient surgery with the best possible outcome to restore normal voice characteristics. Treatment planning before surgery necessitates thorough history analysis and clinical examination. A voice history must be taken and include details of symptoms impacting the voice and laryngeal function, vocal hygiene, vocal use, and ascertaining the presence of known risk factors for voice pathology. Further questioning with regards to the patients general medical history is important as this may affect their fitness for surgery and specifically impact measured outcomes after phonomicrosurgery. For further details on aspects of history-taking and clinical assessment, refer to Chapter 6. Clinical examination should include fiberoptic evaluation of the vocal folds and larynx. Videostroboscopy is essential to assess the vocal fold in more detail and the mucosal wave during phonation. Videostroboscopy is performed using a rigid endoscope or a flexible laryngoscope with distal chip technology for a clearer picture than previously provided by older flexible laryngoscopes. Objective assessment of voice is dealt with in Chapter 7. Both objective and subjective voice assessments before surgery set a baseline for comparison of future assessments. The former can be recorded using the Grade, Roughness, Breathiness, Asthenia, Strain rating scale.6 The latter can be achieved using several quality of life instruments, such as the voice handicap index.7 The evaluation of voice outcome and quality of life measures are described in Chapter 10. Preoperative assessment permits the acquisition of informed consent. Informed consent mandates a clear explanation of the procedure and its benefits, all alternatives, and the risks and complications. These include a risk of trauma to the orofacial soft tissues, chipping/loosening the dentition, and scarring of the vocal folds with potential worsening of their presenting complaint. The latter is a rare complication in the hands of a voice specialist using the appropriate equipment and instruments. Preoperative voice therapy is essential in the management of voice pathology and is important in establishing rapport between patient and therapist, thereby laying the foundation for a strong therapeutic alliance. In some instances, lesions and voice changes may be reversed by this conservative approach alone, for example, vocal nodules. In other instances, it provides a vital opportunity for patient education that serves to enhance the beneficial outcomes of surgery. During voice therapy, adverse patient-specific habits can be identified, vocal technique can be developed, and postoperative advice disseminated. In those cases where there is ambiguity as to the exact nature of the lesion, for example, early small vocal nodules, its response to voice therapy can indicate whether surgical excision is warranted.8,9 Phonomicrosurgery is one step in the management of voice pathology. Factors specific to the patient and the etiology of the vocal fold pathology must be considered before surgery. Patients must be willing and able to attend preoperative evaluations that may include voice therapy sessions, undergo surgery, and adhere to the postoperative regime to ensure a successful outcome. Surgery may need to be delayed or rescheduled, for example, in the professional voice users where a mandatory performance must be given. Or, for example, patients who are unlikely to follow postoperative voice rest instructions due to family commitments. Patients who have systemic factors prohibiting the provision of safe general anesthesia need those factors to be controlled or corrected before contemplating surgery. Medical conditions that impact the larynx and/or the vocal folds must be optimized before surgery, for example, laryngopharyngeal reflux. For specific vocal fold pathology, as mentioned earlier, vocal fold nodules and small polyps may respond to voice therapy; therefore, the indication for surgery is explored after voice therapy.10 Adequate visualization of the vocal folds is imperative when performing vocal fold surgery. Good access is achieved by correct positioning and exposure of the structures of the larynx. The ideal patient position is to lie in the “sniffing the morning air” position. The patient is placed supine on the table, the head is extended at the atlanto-occipital joint, and the neck is flexed on the chest. One must have prior knowledge of any cervical pathology likely to impact on neck movement and bear this in mind when positioning the patient. Clinical Pearls and Pitfalls Use of cold adrenaline-soaked neurosurgical patties improves visualization manifold. This along with the subepithelial infusion technique minimizes blood loss and avoids trauma underlying structures, for example, vocal ligament—this technique is particularly useful with the subepithelial cysts. The largest laryngoscope that can comfortably fit is inserted into the larynx, and the degree of exposure of the vocal folds and laryngeal structures is checked. The laryngoscope can now be attached to a laryngeal suspension system, of which there are several. Some suspension systems allow a degree of flexibility in viewing the larynx. When a chest piece is being used, placing it on a Mayo’s trolley placed just above the patient’s chest provides extension with no movement of the system during ventilation (Fig. 13.2). Measures to improve visualization of the anterior commissure include the application of “sticky tape” or a cotton bandage across the larynx at the level of the cricothyroid membrane and attaching both ends to the sides of the operating table. In a very anteriorly placed larynx, the flexion–flexion position may prove to be useful for both intubation and laryngeal exposure. Magnification is an essential step during phonomicrosurgery; the operating microscope is now positioned ready for surgery to commence. A 400-mm lens is the ideal lens for laryngeal surgery, as it provides optimum magnification at a reasonable distance from the operating field permitting easy passage of instruments down the laryngoscope. Some phonosurgeons prefer to operate using a laryngoscope that has an inbuilt channel for an endoscope that is attached to a camera. In this situation, the surgeon is operating off the monitor and not through the microscope. Before commencing surgery, a preoperative photo of the lesion is taken using a zero-degree Hopkins telescope.
Key Principle: Understanding the Microanatomy of the Vocal Folds
Key Principle: Preservation of the Superficial Lamina Propria Layer
Key Principle: Appropriate Dissection Techniques—Subepithelial Infiltration Technique and Microflap Dissection
Key Principle: Avoiding Collateral Damage and Minimizing Trauma to Vocal Ligament
Key Principle: Why Operate, When to Operate, and When not to Operate
Preoperative Evaluation
Role of Preoperative Speech and Language Therapy
Timing of Surgery
Intraoperative Factors
Access and Exposure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree