19
19 
Principles and Complications of Surgical Therapy for Glaucoma
William H. Lee, III
This chapter is intended to be used by beginning surgeons as a summary guide in their preparation to work under the direction of an experienced glaucoma surgeon. Although this chapter includes a specific step-by-step summary of variations on many surgical techniques, it is not intended to be used as a “field guide” for novice surgeons to independently perform these procedures. Any such attempt would be unrealistic given the difficulties of glaucoma surgery.
Definition
Why Should Surgical Therapy Be Considered For Glaucoma?
When medical therapy is insufficient in lowering intraocular pressure (IOP) enough to protect a patient’s optic nerve over their estimated lifetime, then surgical therapy is indicated.
What Is the Goal of Surgical Therapy?
The goal of surgical therapy is to lower IOP enough to minimize the risk of further optic nerve damage. Surgical therapy is usually reserved for those who remain at high risk for further optic nerve damage despite maximally tolerated medical therapy. As with medical therapy, surgical procedures lower IOP by either increasing outflow or reducing aqueous production (Tables 19–1 and 19–2).
| Argon laser trabeculoplasty (ALT) |
| Laser peripheral iridotomy (LPI) |
| Laser gonioplasty |
| Trabeculectomy |
| Setons |
| Cyclocryotherapy |
| Nd:YAG cyclophotocoagulation (YCP) |
| Diode cyclophotocoagulation |
| Endocyclophotocoagulation |
Note: These procedures destroy ciliary body tissue and are less commonly used. Nd:YAG = neodymium:yttrium-aluminum-garnet. |
When Is An Outflow Procedure Planned Versus a Procedure that Reduces Aqueous Production?
Generally speaking, procedures to increase outflow (Table 19–1) are the first-line surgical treatment for glaucoma. These procedures are considered safer, more successful in preservation of vision, and less painful. Procedures to reduce aqueous humor production (Table 19–2) are reserved for cases that are refractory to interventions that increase outflow because reducing aqueous humor production means destroying ciliary body tissue, which is often difficult to titrate and thereby carries a higher complication rate of phthisis bulbi and blindness. Transient pressure spikes and pain are also not uncommon complications. Furthermore, with the exception of endolaser treatment, the cyclo-destructive procedures cause varying degrees of damage to the trabecular meshwork and other outflow channels, which is another factor in the unpredictability of these procedures. Practically speaking, the cyclodestructive procedures (Table 19–2) are reserved for near end-stage eyes. These patients usually have extensive subconjunctival scarring and are poor candidates for other surgeries. With the advent of the Baerveldt and other more improved shunt devices, there are fewer indications for resorting to cyclodestructive procedures.
Epidemiology and Importance
Why Are Surgical Therapies Considered Earlier in Glaucoma Nowadays?
Over the last 10 years, there has been a trend toward earlier treatment with laser and surgery.1,2 We are beginning to understand that to fully protect the optic nerve over a patient’s lifetime, lower IOPs than previously thought may be required.3 In addition, our surgical techniques have improved. With guarded trabeculectomies and planned postoperative suture lysis, there are fewer serious complications. With antimetabolites such as 5-fluorouracil (5-FU) and mitomycin C (MMC), there are higher bleb success rates as well as lower average postoperative pressures. These developments have led some to advocate earlier surgical intervention.4–8
At the same time, however, medical therapy has likewise improved. Combination drug therapy is now often capable of producing fairly low IOPs, fewer side effects, and higher compliance rates. In this country, primary surgical treatment as opposed to medical therapy is still controversial, even among the experts.9
Does the Incidence and Success Rate of Glaucoma Surgery Vary in Different Countries and Races?
In Europe there has been an even greater trend toward earlier surgery.5–8 This may be because of the more homogeneous population of fair-skinned people, who tend to have fewer surgical failures than the darker races. Consequently, surgical success rates seem to be higher abroad, and higher success rates favor correspondingly earlier surgical intervention.
Another factor is that many of the countries in Europe have a more socialized form of medicine with even greater financial restraints. Early surgery seems to be more cost-effective in the long run than lifelong multimedical therapy.10
Interestingly enough, a similar situation occurs in Africa, where the high cost and poor availability of medications makes primary surgical intervention a more likely treatment.11 Also, although blacks have a higher rate of scarring and thus a higher rate of bleb failure, their increased risk of blindness and earlier onset of disease would suggest that a higher prevalence of surgical intervention would be needed.12 One study found the recently popular procedure of viscocanalostomy highly successful in this group.13
In the United States, however, one study suggests that blacks have a correspondingly lower prevalence of surgical intervention than one would predict on the basis of the prevalence of glaucoma.14 According to this study, the prevalence of glaucoma in the United States is four to six times higher in blacks than in whites and yet the rates of surgery are only 2.2 times higher for blacks than whites. This means that there is a 45% lower than expected rate of glaucoma surgery for blacks than would be predicted by the rates for whites. This finding may not be as surprising considering the lower success rates of trabeculectomy for blacks.
A similar situation was found in a study of the elderly population in the United States. Surgical treatment rates for this group were proportionately less than expected when compared to the prevalence of severity of glaucoma in this age group.15
Other racial differences have also been observed. A recent study found blacks did better with initial argon laser trabeculoplasty (ALT) before resorting to trabeculectomies.16 Whites, on the other hand, fared better in the long-term by proceeding initially with trabeculectomies and using ALT (and subsequent repeat trabeculectomy) as the backup protocol. ALT has also been used quite successfully as initial primary therapy in Egypt, where socioeconomic factors make other treatments more impractical.17 No doubt, socioeconomic factors and the availability of eye care greatly influence treatment patterns both in the United States and elsewhere.
Diagnosis and Differential Diagnosis
When Does Surgical Intervention Become Essential in Glaucoma?
If medical therapy fails to prove adequate for protection of the optic nerve and visual fields, it is important to reevaluate the patient’s target IOP and overall condition. Is the patient compliant? Has the maximally tolerated medical therapy been completely explored? Could high blood pressure, atherosclerosis, nocturnal hypotension (from excessive nighttime systemic beta-blocker agents), anemia, a long-forgotten past hypovolemic/hypoxic episode, or even an undiagnosed intracranial tumor have been contributing factors?
How Is the Decision Made to Intervene Surgically in Glaucoma?
If high IOP is thought to be a major problem, it is always a good idea to repeat gonioscopy prior to considering laser or surgical intervention. It is not uncommon for what was once thought to be primary open-angle glaucoma (POAG) to slowly progress to an accompanying component of chronic narrow-angle glaucoma (especially in blacks) or phacomorphic glaucoma (especially in elderly hyperopes with nuclear sclerotic lens changes). Occasionally, neovascular glaucoma (NVG) is initially overlooked in its earlier stages in patients with diabetes, carotid artery occlusion, or retinal vein occlusion.
Treatment and Management
How Does One Decide Which Procedure to Do First?
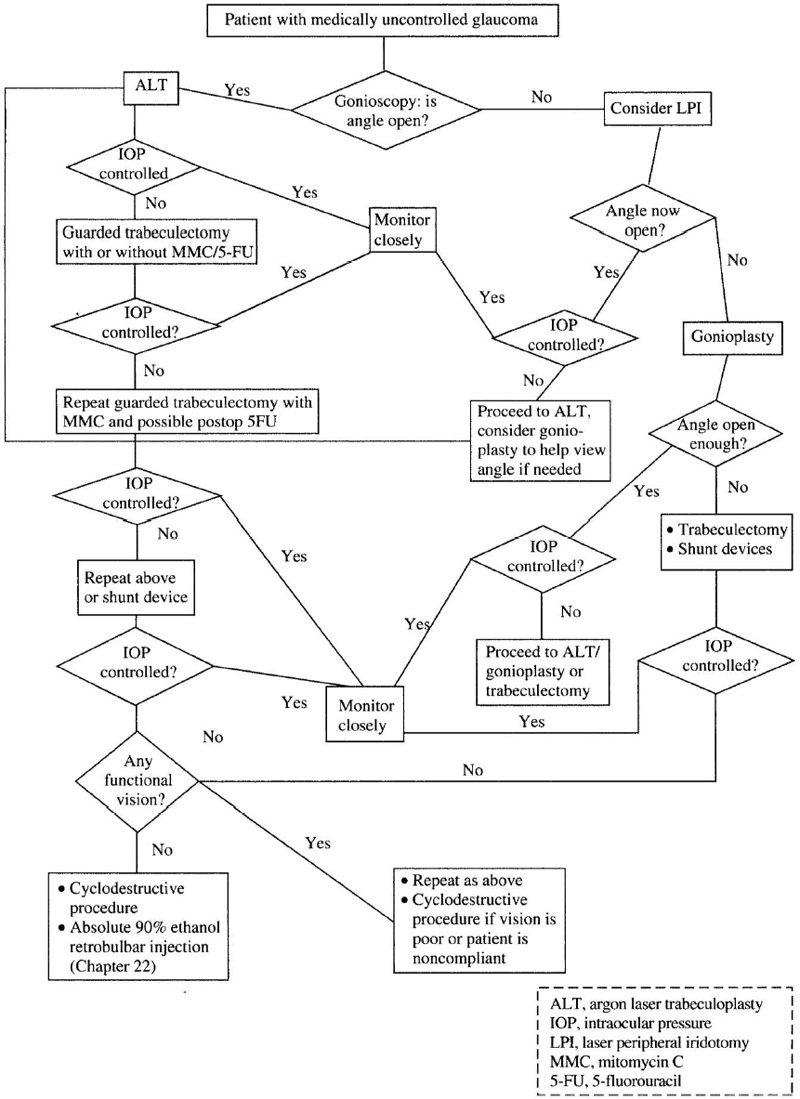
Figure 19–1 outlines the management of patients when maximal medical therapy fails to adequately control IOP. If gonioscopy reveals an open angle, ALT is the first procedure of choice. If this fails, surgical guarded trabeculectomy is indicated. Antimetabolites are used in conjunction with primary trabeculectomy in many patients who are at high risk for failure (younger patients, blacks, patients with a history of prior eye surgery, etc.). Antimetabolites are strongly indicated in patients who have had a prior failed trabeculectomy. If two or more guarded trabeculectomies have failed, or if a patient has neovascular glaucoma, a seton device is usually indicated. Antimetabolites probably should not be used with seton devices.18
Figure 19–1. Management of patients with medically uncontrolled glaucoma.
If gonioscopy reveals the angle to be closed, then compression gonioscopy can be helpful. If the angle compresses open, a laser peripheral iridotomy (LPI) will likely be helpful. If after iridotomy the angle opens but the IOP remains elevated, consider ALT or guarded trabeculectomy (probably with an antimetabolite). If the angle is not open following LPI, then the patient may have plateau iris (rare) or phacomorphic narrowing (more common). Phacomorphic narrowing will have a convex or volcano iris plane in contrast to the flatter iris plane of plateau iris. Gonioplasty is often helpful in patients with phacomorphic narrowing and may be useful in facilitating visualization prior to ALT in these patients. If this fails to open the angle, and especially if cataracts are present, lensectomy with or without trabeculectomy is then indicated for phacomorphic glaucoma. If peripheral iridotomy and gonioplasty fail to open the angle, and a phacomorphic component is not present (the lens is clear and relative eye size is proportionate), then the patient likely has plateau iris or other angle deformity and may require trabeculectomy.
Surgical intervention is indicated, and seton procedures are likely favored over trabeculectomy when the angle is “zippered shut.” Old NVG or extensive peripheral anterior synechiae (PAS) from trauma or iritis are other examples of chronic closed-angle cases that do not respond to LPI or gonioplasty. Seton devices in these patients may be a better choice than trabeculectomy if the surgeon has experience with these devices. If a trabeculectomy is performed instead, then an antimetabolite should be used in most of these cases, unless contraindicated.
What Are the More Common Types of Laser Therapy for Glaucoma?
The common types of laser therapy for glaucoma are enumerated in Table 19–1.
What Are the Indications for ALT?
ALT is the most common surgical treatment for POAG and has also been advocated as an initial therapy for POAG.17,19 Indications for proceeding with ALT vary according to the subtype of glaucoma. Older patients seem to respond more favorably and with fewer side effects than younger patients. Traumatic glaucoma cases respond less favorably. Generally speaking, laser intervention is indicated when medical therapy is inadequate or poorly tolerated due to side effects or noncompliance. When properly applied in appropriate candidates, ALT is generally considered as safe and effective as any single glaucoma medication. Although many laser types have been used, the argon laser is by far the most common laser. Diode lasers are effective and becoming more common.20
What Is the Mode of Action of ALT?
Theoretically, ALT stimulates division, as well as metabolism, of the trabecular meshwork (TM) endothelial cells responsible for active transport of aqueous.21 Historically, a second theory mentions the possibility of a mechanical opening of the TM fibrils.22 This may occur between the areas where the laser is applied (i.e., shrinkage of some tissue may stretch open collateral tissue). Also, shortening of the trabecular band over 360 degrees may open up the collapsed meshwork and/or Schlemm’s canal.
What Are the Principles of ALT?
Generally, we treat half of the functioning angle per session. Usually, ALT is limited to one or two applications per eye over a patient’s lifetime. If the first treatment has little effect, and assuming it was properly applied, then it is less likely that a second treatment will help. If the first treatment involving 180 degrees of the angle was successful, but over time the IOP has again risen, then it is reasonable to attempt another treatment in the remaining 180 degrees of TM. Do not treat if you do not have a clear shot at the TM; hitting the peripheral iris in the angle will lead to extensive formation of PAS. Avoid treating an area of scarred angle or an area of PAS. Try to treat only the functioning angle as identified by an area with some pigmentation in the TM. Atrophic parts of the TM are distinctively nonpigmented. They take up laser poorly and, even if treated, provide minimal if any effect. It is not worth treating these areas.
Is There a Need for Medical Prophylaxis Before ALT?
If not otherwise contraindicated, pre- and postlaser treatment with Iopidine 1% (apraclonidine 1%) can significantly reduce chances of pressure spikes following both ALT and LPI.23 Alternatively, some surgeons are using Alphagan (brimonidine tartrate 0.2%) as a substitute, although one must be aware that the pressure-lowering effect may not be as great. Cooling the eye (ice packs) is also effective, but most find this less practical.
What Is the Procedure for ALT?
The procedure for ALT is as follows:
- Preoperative apraclonidine 1% is given at least one half-hour before the procedure.
- Focus both oculars so aiming beam is parfocal.
- Topical anesthesia is delivered and the Goldmann lens is used to view the angle.
- The dye laser is “tuned” to the all-green mode or the argon laser is set on the green mode.
- Spot size is 50 μm.
- Time is 0.1 seconds.
- Power settings vary with different lasers and degrees of angle pigmentation. A common initial power setting in a medium pigmented eye with a dye laser in the green mode is between 200 and 400 milliwatts (mW). The power is adjusted to just produce a white blanch at the juncture of the anterior TM (nonpigmented) and posterior TM (pigmented). If a bubble is produced for a microsecond, then the laser power is turned down. Conversely, if no blanch is seen, then the power is turned up. This assumes the surgeon is in a functioning (not atrophic) angle. It also assumes that the argon aiming beam is well focused and centrally located within the gonioscopic mirror of the Goldmann lens, and that the target is the juncture of the nonpigmented and pigmented trabecular meshwork. If the desired effect is not seen, the laser is turned up or down by 50-mW increments until the desired target intensity is reached.
- Darker pigmented TM will absorb more laser and therefore requires less energy.
- Lighter pigmented TM will absorb less laser and therefore requires more energy.
- The atrophic angle will not have pigment and will not take up laser.
- Aim for the junction of the anterior TM (nonpigmented) and the posterior trabecular meshwork (pigmented). This normal anatomy is seen in areas of functioning angle. If it is not well demarcated, then it is likely not worth treating that area!
- The number of shots varies according to how much functioning angle is viewable. Most surgeons leave a space equal to the width of the aiming beam between each laser application. Assuming the total angle is viewable and normal in appearance, the average number of applications per 180 degrees of treated angle is approximately 45 shots.
- Apraclonidine 1% is given immediately postop; prednisolone acetate 1% (Pred Forte) or loteprednol elabonate (Lotemax) are given q.i.d. for 4 days, or as needed.
- IOP is checked at 1 hour and at 1 to 7 days postoperatively.
- The number of shots varies according to how much functioning angle is viewable. Most surgeons leave a space equal to the width of the aiming beam between each laser application. Assuming the total angle is viewable and normal in appearance, the average number of applications per 180 degrees of treated angle is approximately 45 shots.
How Effective is ALT?
Eighty percent of eyes initially respond with a significant reduction in IOP. After 5 years, 50% of eyes are thought to still have a measurable pressure lowering effect.24
What Are the Complications of ALT?
The most common side effect of ALT is a transient increase in IOP (pressure spike) and/or inflammation (cells and flare). Preoperative and postoperative apraclonidine 1% and postop antiinflammatory agents have greatly reduced the chance of these side effects.
What Are the Indications for LPI?
LPI is the primary treatment of choice for acute narrow-angle glaucoma and chronic narrow-angle glaucoma due to pupillary block. It has a more subjective use in the prophylaxis for prevention of narrow-angle glaucoma in patients at high risk. Likewise, there is some indication for prophylaxis in patients with relative pupillary block (intermittent narrowing of the angles). More recently, LPI has been found useful in select patients with pigment dispersion syndrome.25 It does not resolve plateau iris configuration, but this diagnosis is usually not made until LPI has already been attempted because it is a diagnosis of exclusion.
What Is the Mechanism of Action of LPI?
LPI relieves the buildup of pressure in the posterior segment due to relative or absolute pupillary block. By providing an alternate route for aqueous humor to pass from the posterior segment to the anterior segment, there is no longer pressure buildup behind the iris from an occluded pupil. In the pigment dispersion syndrome, a transient increase in the pressure of the anterior chamber compared to the posterior chamber can push the midperipheral iris back onto the zonules and cause dispersion of pigment in some patients. An iridotomy theoretically equalizes the pressure gradient in these cases.
How Is LPI Performed?
LPI can be accomplished with the yttrium-aluminum-garnet (YAG) or argon laser. The YAG laser penetrates the iris quicker and is the most common type used. The argon laser is still sometimes used to pretreat (before the YAG laser), to cut down on the incidence of iris bleeding. This may be especially helpful in patients on Coumadin or aspirin therapy. Argon lasers are quite poor for penetrating lightly pigmented irides and YAG lasers will often be necessary in these eyes.
What Are Some Principles to Consider in Site Selection of LPI?
- Avoid any surface iris vessels.
- Look for deep crypts to reduce the amount of tissue through which the laser has to penetrate.
- Apply the laser at 11 o’clock or 1 o’clock on the peripheral iris. The purpose of having the iridotomy superiorly is so that the upper lid will cover the iridotomy and prevent monocular diplopia or glare. The purpose of treating at 11 o’clock or 1 o’clock as opposed to 12 o’clock is that lasers sometimes form bubbles. Bubbles can obscure the view of the area being treated. Bubbles will usually float up to the 12 o’clock peripheral iris.
- Site selection is of major importance. The goal is to be peripheral enough to avoid hitting the lens. (In fact, an LPI that has underlying lens apposition is useless.) At the same time, if you are too peripheral, the view will be clouded by the peripheral haze of the cornea. The cornea runs more obliquely and is thicker (and therefore more opaque) at the far periphery, and so visualization at the far periphery is poor. Also, because of the shallowness of the chamber in this location, corneal endothelial damage is more common at the far periphery.
What Are Some of the Specifics in Performing LPI?
- Apply apraclonidine 1.0% preoperatively.
- Apply pilocarpine 1.0% preoperatively to flatten iris.
- Apply Abraham eccentric lens.
- Set YAG power to 4–5 millijoules (mJ) on double burst mode and apply laser.
- Refocus deeper and reapply laser until penetration achieved.
- Give apraclonidine 1.0% again postoperatively.
- Check IOP at one hour and then as needed.
- Start topical steroids postoperatively for 4–7 days.
What Are Some Other Considerations When Performing LPI?
If the laser penetrates full thickness, then a pigmented fluid wave will be visualized coming forward through the iridotomy site. If this is not seen, refocus at a new depth of the same site and reapply laser. Remember that as one goes posterior into the iris and approaches the posterior segment, the power setting should be reduced to avoid posterior segment damage.
What Are the Complications Associated with LPI?
Hemorrhaging and pressure spikes are the most common complications. If a hemorrhage occurs during laser treatment, then gentle pressure to the globe with the Abraham lens will often stop the bleeding. Continue holding pressure for a minute and then recheck to see if it is still bleeding. This can be repeated several times. If this fails to stop the bleeding, it is best to proceed with argon laser cautery to the area.
Pressure spikes are usually controlled medically (may require mannitol). Patients should be warned, however, that rarely a dangerous pressure spike may occur and necessitate trabeculectomy.
How Effective Is LPI?
Almost always, a single, patent iridotomy is successful in preventing or relieving pupillary block. The degree of success for treating select patients with pigment dispersion syndrome is not yet known.
What Are the Indications for Argon Laser Gonioplasty?
A gonioplasty may be indicated when angle crowding of the iris persists in a patient with narrow-angle glaucoma who has already had a peripheral iridotomy. Usually, this occurs in patients who have a superimposed degree of phacomorphic or plateau iris crowding. Also, it is often used to facilitate visualization of the angle prior to ALT in these patients. Argon laser gonioplasty is used usually as a temporary measure in patients who are not yet otherwise ready for cataract surgery or combined cataract/glaucoma surgery.
What Is the Mechanism of Action of Gonioplasty?
The procedure uses the argon laser to burn areas of iris stromal tissue in the peripheral iris. This results in contracture of tissues and pulls the peripheral iris from the angle. In cases with some degree of phacomorphic component, it may flatten and stiffen the midperipheral iris to reduce its anterior bulge. Likewise, in plateau iris configuration and nanophthalmos, it may prevent appositional angle closure.
What Are the Principles of Gonioplasty Treatment?
- Avoid iris vessels because sectoral iris atrophy may result.
- Try to treat only a quadrant or perhaps one-half of the iris at a time in order to avoid pressure spikes.
- Keep laser burns in a radial row of two to three burns. Visualize what part of the iris is moving with each application. You should be able to see iris pulling away from the angle as it is flattened. If you see iris stretching the pupil open, then you need to be more peripheral.
How Is Laser Gonioplasty Performed?
- Pretreat with apraclonidine 1%.
- Apply the Abraham lens.
- Set argon laser to green wavelength.
- Spot size is 100 to 200 μm.
- Power setting is 100 to 200 mW. (Use the least amount of power to produce movement of collateral iris tissue. It will also produce a small white blanch.)
- Treat in radial rows of two to three burns. This usually means 10 to 12 shots per quadrant.
- Apply apraclonidine 1% postoperatively.
- Recheck eye pressure 1 hour following procedure.
- Administer a drop of cyclogyl 1% to prevent posterior synechiae.
- Administer prednisolone acetate 1% every 4 hours for 4 days or as needed.
- Recheck 1 to 7 days postoperatively.
What Are the Complications Associated with Laser Gonioplasty?
The most common complication is pressure spike, which can usually be handled medically. All patients should be warned of the chance for iris atrophy in the sector that is being treated. This is especially true if a radial iris vessel is treated. Patients should know that this may change the color of their iris.
When Is Surgical Trabeculectomy Indicated?
Surgical trabeculectomy is indicated when optic nerve function remains threatened by current IOP and medical and laser treatments have been inadequate or poorly tolerated.
Why Not Proceed Straight to Surgery?
Using surgery as the initial treatment for glaucoma has been popular abroad.1 It is postulated that surgery is more successful in some of these communities because of the homogeneous population. Moreover, socialist medical environments may be more cost conscious. In some cases, multiple medical therapy may simply be too expensive as a lifetime treatment. It is also known that medication and preservatives in topical eye drops taken long-term can increase bleb scarring and thereby reduce surgical success.26,27 Even ALT has been linked as a possible cause of encapsulated blebs following filter surgery.28 Another study found male gender to be a risk factor for bleb encapsulation, but the risk from ALT was not statistically significant in that study.29 All of these factors have generated a push by some toward primary trabeculectomy.1
In this country, patients are living longer and our attitudes are changing as to how low pressure must remain in order to reasonably sustain optic nerve function for a given patient’s lifetime. We are being more aggressive with IOP and are proceeding with surgery at earlier stages than in the past. It is important to remember, however, that the incidence and severity of complications with glaucoma surgery is still relatively high compared to other ophthalmic procedures (e.g., cataract surgery, refractive surgery, etc.). Also, success is much less predictable in glaucoma surgery compared to other eye procedures because outcome is so dependent on each patient’s individual scarring response (determines bleb success) and preexisting degree of outflow obstruction (determines how much filtration a given surgery must achieve in order to lower IOP). Furthermore, many of our latest and most potent topical medications (Xalatan, Alphagan, Cosopt, to name a few) were not available when the trend toward primary trabeculectomy began with the “Moorfield studies” of the 1980s.5–8
Even with the most successful glaucoma surgery, it is common to have some increase in the cloudiness of the lens.30 In addition, many patients will be forever symptomatic because of their well-functioning bleb (foreign body sensation). Furthermore, all patients with a functioning bleb are at a lifetime risk for bleb infection and possible endophthalmitis. For all of these reasons, surgical trabeculectomy is generally reserved for patients who remain at high risk despite prior medical and laser therapy.
What Is Guarded Trabeculectomy?
There are an infinite number of variations of glaucoma filtration surgery (Table 19–3). The guarded trabeculectomy is the procedure of choice for most patients. These procedures can utilize either a fornix-based conjunctival incision (conjunctiva is opened at the limbus) or a limbal based conjunctival incision (conjunctiva is opened about 10 mm posterior to the limbus and dissected forward). Each type of conjunctival incision has advantages and disadvantages with corresponding proponents and opponents.
The majority of trabeculectomies are performed under local anesthesia using peribulbar or retrobulbar anesthesia. A peribulbar block is considered safer than a retrobulbar block and therefore is usually recommended. Usually a 1:1 mixture of lidocaine 2% with Marcaine 0.75% is used along with Wydase. More recently, topical anesthesia combined with localized subconjunctival lidocaine 2% and intracameral nonpreserved lidocaine 1% has been occasionally used. This method does not work in all cases because of the lack of adequate akinesia. General anesthesia is sometimes advocated in monocular patients at high risk for retrobulbar or peribulbar anesthesia.
Guarded trabeculectomy First described by Sugar in 1961 and later made popular by Cairnes32 in 1968, this procedure is the most common type of filter surgery performed today. The technique uses a block of sclera to partially occlude or “guard” the egress of fluid from the anterior chamber into the subconjunctival space. This modification greatly reduces the chance of complication due to hypotony in the early postop period. It also reduces the risk of endophthalmitis in the late postop period that was sometimes seen with the thin cystic blebs of full thickness trabeculectomies. Unguarded or full-thickness trabeculectomy This was made popular by MacKenzie in 1830, and early 20th century variations by LaGrange and Holth were used widely until the 1970s.33 It is rarely used today due to the high incidence of the above-mentioned complications. Non-penetrating filtration surgery First described by Zimmerman et al.34,35 in 1984, this is a group of relatively new procedures that leave the innermost fibers of the trabecular meshwork intact. These procedures use a superficial scleral flap just as in traditional guarded trabeculectomy. Under this flap a very deep sclera block is dissected and excised, thereby directly exposing scleral spur. As this dissection is carried to the limbus, Schlemm’s canal and the inner wall of uveal trabecular meshwork (TM) is exposed. Aqueous from the anterior chamber can be seen “percolating through” the thin membrane of uveal TM or peripheral Descemet’s membrane. The superficial sclera block is then sutured back in place. Often collagen implant or viscoelastic is left underneath the superficial scleral flap to maintain an intrascleral reservoir. Being extraocular procedures, the nonpenetrating surgeries may have fewer complication rates of cataract formation, postop hypotony, and uveitis. Because no peripheral iridotomy is performed, bleeding is less of a problem. These relatively new procedures may become increasingly important in the future but they are technically challenging, and long-term success rates are not yet known. A more recent version of this procedure by Stegmann et al.13 called viscocanalostomy is performed in a similar manner, but adds the injection of viscoelastic directly into Schlemm’s canal during the procedure. Shunting or seton devices These were first described by Molteno36 in 1969, and have undergone many variations since. There are a number of valved (Krupin, Ahmed) and nonvalved (Baerveldt, Molteno, Schocket) shunts available. Usually, these devices are reserved for patients with failed prior trabeculectomy or a propensity toward scarring such as neovascular glaucoma. They are also indicated for those patients with extreme scarring of the angle. Most of these devices consist of a tube that remains in the anterior chamber and “shunts” aqueous to an external subconjunctival reservoir. The larger the surface area of the reservoir, the lower the postoperative IOP. These devices require a higher degree of surgical expertise and are fraught with their own individual set of complications. They are invaluable, however, in patients who are at high risk for trabeculectomy failure. |
How Is a Guarded Trabeculectomy Performed?
Guarded trabeculectomies can be done in many ways. The scleral tunnel technique described below is the safest and most reproducible procedure. Because it uses the traditional “cataract” scleral tunnel technique, it is highly adaptive to combined cataract/glaucoma surgery. The scleral tunnel technique allows for the most uniform and reproducible scleral flap.
A cornerstone to the concept of this surgery is that the scleral flap will be made almost watertight with the intention of performing laser suture lysis postoperatively. This greatly reduces the biggest risk for complications in glaucoma surgery, namely postoperative hypotony. This concept has revolutionized glaucoma surgery in that good filtration can be obtained without many of the risks encountered with earlier techniques, such as full-thickness trabeculectomy, Elliot’s trephine, cyclodialysis, etc.
Be sure to prepare the patients beforehand that they will likely have laser suture lysis between 1 and 4 days following surgery. They should be informed that this is a routine part of this type of glaucoma surgery and that although it is an extra step, they are receiving the safest form of surgery.
What Is the Mode of Action of Trabeculectomy?
The goal of glaucoma filtration surgery is to produce a fistula from the anterior chamber through the sclera to allow a controlled amount of aqueous to egress into the subconjunctival space (thus lowering IOP). The aqueous is then reabsorbed into the bloodstream by subconjunctival venules. Transconjunctival evaporation also likely occurs.
What Are the Principles of the Trabeculectomy Procedure?
- Administer inferior and superior peribulbar block; apply intermittent digital pressure until the globe is soft.
- For sterilization, prep with a 50% Betadine solution. Also use it topically to irrigate the cul-de-sac. (Use 25% topically if the case is being done under topical anesthesia.)
- Use talc-free gloves to reduce the chance of Tenon’s cyst formation.37
- Insert a wire lid speculum.
- Pass an 8-0 Vicryl suture through the superior peripheral cornea about 3 mm from the limbus as a corneal traction suture. (Inferior corneal traction sutures also work well if tucked below the lid speculum.)
- For a fornix-based flap, perform a conjunctival peritomy. This is made about 8 to 10 mm in chord length.
- Take special care not to tear the conjunctiva. Use only conjunctival forceps (which has ridges but not teeth) so that conjunctival edges are not torn.
- At the beginning of the peritomy, a relaxing incision is made by initially entering the conjunctiva 4 mm posterior to the limbus to gain access into the sub-Tenon’s space and thereby allow for a sub-Tenon’s dissection, because Tenon’s ends before the conjunctiva at the limbus. This initial entry should be well away (8 mm) from the intended trabeculectomy site.
- After the initial entry, it is important to dissect sub-Tenon’s for the full extent of the conjunctival incision and as close to the limbus as possible. This will expose bare sclera.
- Do not perform aggressive undermining of the peritomy into the quadrants. Just open the conjunctiva enough to allow adequate exposure for surgery. Further posterior dissection is counterproductive, as it only aggravates the inflammatory response.
- Eraser-tip wet-field cautery is used for bleeders and to lightly blanch the area of the sclera to be incised (sclera flap).
- Use a Beaver blade no. 6600 because this single blade can be used for both steps of the formation of the scleral flap.
- Begin the scleral incision 4 mm posterior to the limbus and parallel to it.
- Use the blade to make a three-quarter depth scleral incision. Stop when the deeper blue hue of the inner sclera is seen. Get a feel for the thickness of the sclera and try to achieve the correct depth within the second or third pass. Make the incision about 4 to 5 mm long.
- Turn the blade over so it is parallel to sclera and insert the rounded tip into the deepest part of the incision. Use a wiggling motion to advance the rounded tip within a single plane (parallel to the sclera surface) and into clear cornea. If too much resistance is encountered as the blade advances, then the established plane may be too shallow. This part of the incision is identical to the typical scleral tunnel cataract incision, which is why it is so well adapted to combined surgery, even though the initial incision is not quite as anterior as with typical cataract surgery.
- Advance the blade until it can be visualized about 2 mm beyond the limbus into clear cornea.
- Widen the scleral tunnel so that it is exactly uniform to the edge of its original scleral entrance incision, that is, 4 to 5 mm wide. If the tunnel is made wider than the incision, it will be difficult to get the sclera flap watertight.
- Use Vannas scissors to open both sides of the tunnel to the surgical limbus. Be sure the scissors blades are exactly perpendicular to the sclera that is being cut. Enter the tunnel flat with one blade of the scissors, and then turn the scissors so the blades are perpendicular to the surface of the sclera (one blade within the tunnel, one blade on top of the sclera) and slide the scissors sideways all of the way to the edge of the tunnel to get this incision as perpendicular and uniform as possible. Usually, it takes three or four snips to get to clear cornea on each side. Go up to but not beyond clear cornea or else leakage may occur here.
- Lift the flap and there should be a uniform direct view of the corneal-scleral junction. At least 1 mm of clear cornea should be viewed anterior to this lamellar junction. If this is not seen, then use the Beaver blade again to establish that length.
- If using MMC, first close the scleral flap and apply 0.2 mg/mL for 2 minutes38 on top of the scleral flap. 5-FU in a concentration of 25 to 50 mg/mL for 5 minutes also works well and may be safer.39 Unlike MMC, 5-FU is not a strong alkylator and though toxic to cells of replication (fibroblasts), it has little effect on static cells (sclera). Comparatively speaking, 5-FU is less destructive to scleral and conjunctival tissue and therefore carries less of a chance for late-onset bleb leaks and associated infections. The instrument wipe sponge or corneal light shield40 provides a more uniform uptake of MMC or 5-FU than does the Week cell. Cut a 4- × 4-mm piece of this sponge and place it directly over the scleral flap after it has been soaked in the antimetabolite. Care must be taken to make sure that no edges of the conjunctiva touch the sponge. The sponge does not go underneath the scleral flap, but simply sits on top of it.41 After 2 minutes, use a Weck cell to dry the area completely, and then use copious amounts of balance salt solution (BSS) to dilute any remaining antimetabolite. It is helpful to lift the conjunctival edges up so that they are not in contact with the solution while irrigating.
- Use a microsharp blade to create a paracentesis site at the temporal limbus. If topical subconjuctival anesthesia is being used, then inject the non-preserved intracameral lidocaine 1%.
- If the chamber is at all shallow, then apply a small amount of viscoelastic just at the 12 o’clock site to deepen the chamber just beneath the trabeculectomy. It is not necessary or desired to fill the whole chamber with viscoelastic in most cases.
- To establish the trabeculectomy site, use a microsharp knife (or 2.6-mm keratome if performing phacoemulsification) to enter the anterior chamber beneath the scleral flap. This is done in the same manner as in a paracentesis. The entrance of this incision should be at least 1 mm anterior to the corneal scleral juncture, that is, 1 mm into the cornea and 3 or 4 mm in length. Be sure it is near the center of the overlying scleral flap, and not near its edges.
- If the chamber shallows as this incision is made, then use viscoelastic to focally push the iris back down.
- Insert the Kelly or Holth scleral punch. It must be inserted with the blade open. Be sure it is completely within the eye. (It usually is a tight fit and one feels it “pop through” into the anterior chamber.) Then rotate the instrument so it is directly perpendicular to the scleral plane (rotate the handle upward).
- Once the instrument is perpendicular to the scleral surface, snip out the corneal-scleral junction and proceed snipping bits of tissue into the trabecular meshwork. With each snip inspect the tissue removed, and remove it from the guillotine. If the tissue is carefully inspected, the small pigmented lines of the trabecular meshwork can usually be seen once it is reached. Once the TM is removed, no further punching is needed. Usually, this requires two to three snips posteriorly. Keep the width of the punch excision to a single width. The inner block of corneal-sclera that is removed only needs to be one punch wide to work properly. Two to three punches posteriorly usually penetrate trabecular meshwork, and often into scleral spur.
- As you approach TM with the punch, be sure that the punch does not entrap a peripheral iris roll, iris root, or the anterior portion of the ciliary body. Cutting these will result in profuse bleeding.
- When done properly, heavy bleeding with the above procedure is rare. If it occurs, then Myra cautery or a retinal cautery (pointed tip) will likely be needed for control.
- Use a 0.12 forceps and Vannas scissors to create a small underlying iridotomy. When using the forceps to grasp the iris, it is important to grasp the iris more central than the tissue that presents at the trabeculectomy site to avoid pulling the iris root or cutting the anterior portion of ciliary body or iris arcade. That is, grab a point slightly peripheral to the mid-iris, where the peripheral one-third of the iris meets the central two-thirds.
- Once the iridotomy is made, reapproximate the scleral flap and use BSS on a 27-gauge cannula through the paracentesis site to flush the anterior chamber free of viscoelastic and to establish filtration.
- It is important to prevent the eye from becoming hypotonous (flat chamber) at any point in the case, as this will precipitate anterior displacement of the ciliary body. Use BSS or viscoelastic as needed.
- Next, secure each corner of the scleral flap back down using a 10-0 nylon suture. Cut the sutures on the knot, and try to bury the knot outside of the scleral flap.
- Check filtration by injecting BSS (on a 27-gauge cannula) through the paracentesis and watching the flow rate around the scleral flap. In white patients with nonscarred eyes, there should be almost no leakage at normal pressures. Instead, a white glistening reflex is seen in the scleral groove. If leakage occurs, continue using interrupted 10-0 to make the flap almost watertight. By injecting BSS, an IOP in the mid-teens should be established. In blacks or patients suspected of scarring, slightly more filtration can be allowed. Still the filtration should be a bare trickle, and an IOP of about 10 mm Hg should be maintained after injecting BSS.
- In addition to the corner sutures, often several additional sutures are required to get the scleral flap sufficiently leak-free at normal IOPs. Using BSS through the paracentesis, our goal is usually to establish filtration that allows for an IOP of about 10 to 15 mm Hg. Once this is established, it is a good idea to recheck after 1 or 2 minutes to be assured that the eye is holding that pressure. If so, the end point is reached, and the eye is ready for closure.
- Once the conjunctiva is reapproximated to its original position over the trabeculectomy site (but prior to suturing), it is mandatory to assess the amount of Tenon’s capsule over the trabeculectomy site. Remember that the sutures that close the scleral flap must be easily visible through the conjunctiva to allow for suture lysis postoperatively. It is therefore usually necessary to tease away and remove one or two layers of Tenon’s capsule beneath the conjunctiva to allow for this. Using a conjunctival forceps to pick up the anterior lip of the incision of conjunctiva, the underlying Tenon’s layers can be split away using the Vannas scissors in a blunt dissection method. This must be started at the area of the initial conjunctival relaxing incision where Tenon’s capsule and conjunctiva can be separated. By inserting the scissors with tips closed into this potential space, and then spreading with scissors, a plane can be established. Then the scissors can be used to remove this excess tissue above the scleral flap site. Extreme caution must be exercised to prevent buttonholing of the conjunctiva. Irrigation of BSS on a 27-gauge blunt cannula can be helpful to establish this potential tissue plane. Once Tenon’s capsule is removed and the translucent conjunctiva reapproximated, the 10-0 nylon should be easily visible through it. (Separate dissection of conjuctiva and Tenon’s capsule at the beginning of the case is also an alternative and sometimes is easier.)
- To close the conjunctiva reapproximate it to its original position and hold it in place with a 10-0 nylon (BV needle) at each corner of the original limbal incision. Be sure to include a bit of episcleral tissue so that the conjunctiva does not retract, and it will be held fast to that spot. Additional interrupted or running 10-0 nylon (BV needle) is then used on any relaxation incisions that were created. With all interrupted sutures, it is best to cut on the knot.
- Now use the Beaver blade to rough up the epithelium of the clear cornea at the limbus overlying the trabeculectomy site so that the conjunctiva will better stick down at the site.
- To keep the conjunctiva from retracting at the limbal site of the trabeculectomy, an anterior circumferential suture is quite helpful, and is used in almost all cases. A10-0 nylon suture on a spatula needle is passed into clear cornea just central to the limbus at the point where the conjunctiva should adhere. The needle track runs parallel to the limbus. The entrance of the needle is at one side of the trabeculectomy site in clear cornea, and the exit of the needle is at the other side of the trabeculectomy site in clear cornea. The needle passes three-quarter depth through the cornea. Next, impale the conjunctiva near its lip from the underside so that the needle exits from the surface of the conjunctiva. The nylon then passes over the surface of the conjunctiva, and the needle is then passed from the outside surface of the conjunctiva near its lip (at the other end of the trabeculectomy site) to its undersurface and pulled out from underneath the free edge of the conjunctiva. Then this loop is tied and the knot is rotated slightly so that it is underneath the conjunctival lip. When the knot is properly tied, the conjunctiva will be pulled down over the limbus, and the lip of conjunctiva will cover the knot. Use BSS through the paracentesis site to see if a bleb is created. In patients with scarring who need some filtration, a bleb should be created. In patients who are thought to leak easily, the trabeculectomy is closed watertight and a bleb will probably not be noticed. If there are any potential gaps in the conjunctiva, they should be closed with interrupted 10-0 nylon. This is especially important if MMC is used. If no filtration occurs, then be sure to use the paracentesis site to reduce IOP to the low-teens range. Suture lysis will be required in 24 hours. If IOP is not sustained to at least 10 mm Hg, then additional scleral sutures will likely need to be applied, which will require taking the conjunctiva back down. The rare exception to this is if one expects a high degree of outflow dysfunction in the trabecular meshwork, and a high degree of aqueous production, which will support additional filtration. Sometimes lower pressures will be tolerated if the anterior chamber is very deep and the iris is stiff. In most patients, however, it is best to take the conjunctiva back down and “tighten up” the filtration at the scleral flap if the eye does not hold at least 10 to 15 mm Hg.
- Eraser-tip wet-field cautery is used for bleeders and to lightly blanch the area of the sclera to be incised (sclera flap).
How Are Combined Cataract and Trabeculectomy Procedures Planned?
When combining this procedure with cataract surgery, there are two major differences:
- Make the initial scleral flap incision slightly more anterior than usual to make it easier to perform phacoemulsification. That is, instead of beginning a flap 4 mm posterior to limbus, create the incision 2 to 3 mm posterior to the limbus.
- After the flap is made and it is time to enter the eye, use a keratome (usually 2.6 mm wide) to enter the anterior chamber underneath the flap. Enter in the same way one would normally during a scleral tunnel type cataract surgery. Usually, the entrance for cataract surgery is slightly more anterior (further into clear cornea) than it is with trabeculectomy. This prevents the iris root from coming up through the incision site during phacoemulsification and aspiration.
After the cataract is removed, viscoelastic is used to fill the capsular bag as well as the anterior chamber. The incision is enlarged to about 3.5 mm and a foldable implant (Acrysoft of other nonsilicone material) is inserted.
Before removing viscoelastic from the eye, finish the trabeculectomy. It may be necessary to use a microsharp blade to make another entrance into the anterior chamber beneath the flap, which is more posterior than the existing cataract entrance, to make it easier to use the scleral punch. When more experience is gained, a single entrance into the anterior chamber (i.e., halfway between the normal cataract entrance and the normal trabeculectomy entrance) can usually be used instead. After the iridotomy and before suturing the flap, use the irrigation/aspiration mode to remove the viscoelastic. Because the temporal clear cornea approach is so much easier for cataract surgery, many surgeons are performing each procedure separately.
What Is the Postoperative Care for Patients After Filtration Surgery?
- Apply cycloplegics.
- Apply topical steroid/antibiotic ointment
- Avoid subconjunctival injections, especially when MMC was used. Leaks can develop through needle tracks.
- Apply topical beta-blocker if not contraindicated.
- Give Diamox 500 mg sequel to take with supper if not contraindicated.
- Remember a pressure spike is possible with this procedure, especially if no filtration is present initially.
- See the patient 24 hours later and consider suture lysis. Make note of which suture was required to stop leakage, plan to laser that suture first.
- Use Pred Forte 1% q.i.d. and Ocuflox or Ciloxin q.i.d. as needed. This is continued for at least 1 week, at which time the antibiotic is stopped and Pred Forte is continued q.i.d. another week, then tapered off by decreasing it to three times daily for 1 week, then twice daily for 1 week, then once a day for 1 week. If conjunctival inflammation is still present after tapering Pred Forte, then start fluorometholone (FML) 0.1% q.i.d. for one week and then begin tapering again. Any conjunctival sutures causing irritation should be removed at 1 week.
- If combined cataract surgery is done, Pred Forte 1% may be used more aggressively, that is, every hour for the first day, every 2 hours for 48 hours, and then four times a day for 2 weeks, and then taper as above.
How Is Suture Lysis Performed?
- Use a Hoskins lens to magnify the suture and compress the conjunctiva.
- Use the argon laser with a spot size of 100 μm, power of approximately 200 mW, and time of approximately 0.1 seconds.
- Once a suture is cut, see if the bleb increases and IOP drops to the desired level. If minimal effect is achieved, then continue cutting other sutures one by one.
- Recheck patient again in 24 hours to see if additional sutures will need to be cut.
- Usually suturelysis is ineffective after 2 to 4 days. One of the reasons to use Pred Forte 1% every 2 hours is to extend the time that suture lysis may be effective, that is, usually only up to 48 hours, but with aggressive steroids, possibly up to 4 days or more in some patients.
What Are the Complications of Filtration Surgery?
Some degree of cataract formation is very common.30 Some other possible complications are listed in Table 19–4. The most common complications are related to the IOP being either too low or too high postoperatively.
Hypotony
Optic nerve damage (snuff syndrome)
Infection
Anterior segment and corneal problems
Phthisis bulbi |
What If the IOP is Too Low?
Low IOP following surgery is due to either a wound leak (Seidel positive) or overfiltration (Seidel negative). Most wound leaks need to be repaired with additional sutures at the site of leakage. With thin conjunctiva that leaks through needle tracks, sometimes a patch graft is required. Occasionally some suture leaks can be handled conservatively by lowering IOP with topicals or Diamox to reduce the flow of aqueous through the leak and then patching to allow scar tissue to close the wound. Cyanoacrylate (superglue) can also be used to patch a leak. These methods, however, are not often successful and may jeopardize the success of the filter. Usually, it is best to return to the operating room and repair the leak with additional sutures.
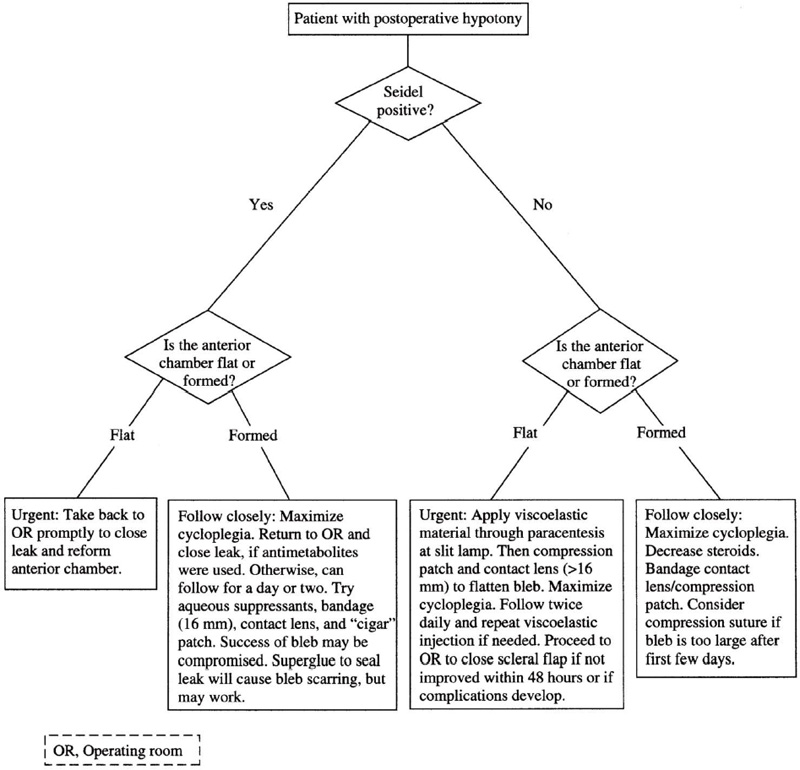
If IOP is low due to overfiltration, then conservative treatment is given as long as the anterior chamber is well formed, no significant choroidal detachment is present, and there is no sign of hypotensive maculopathy or retinal vein occlusions (Fig. 19–2).
Figure 19–2. Management of postoperative hypotony.
What Is the Conservative Treatment for Hypotony after Filtering Procedures?
Cyclogyl 1% is given four times a day to relax the lens-iris diaphragm and help keep the chamber formed. If the problem is overfiltration (large bleb), a large-diameter contact lens (16 to 18 mm) to reduce the bleb size is helpful, as is tight patching or “cigar” patching (i.e., the placement of an extra “roll” of sterile gauze at the superior lid crease overlying the bleb). Steroids are generally temporarily reduced to allow bleb size contraction. If the anterior chamber begins to shallow and especially if there is any iris-TM touch, then more aggressive steps must be taken.
What Is the More Aggressive Therapy for Hypotony After the Filtration Procedure?
Give Cyclogyl 1% four times a day. Reform the anterior chamber. This can usually be done at the slit lamp by injecting viscoelastic (Ocucoat) through the paracentesis site. If the entrance of the paracentesis has already re-epithelialized, it can be easily opened by using a 27-gauge needle (bevel side up) to poke through the epithelium and reestablish the preexisting paracentesis. Then use the blunt viscoelastic cannula for injection.
- The patient should be checked twice daily and viscoelastic injections can be repeated if necessary.
- If the anterior chamber will not stay formed on its own after 48 hours, then the patient will require a trip back to the operating room to tighten down the scleral flap with more sutures.
- Back in the operating room, be sure to recheck for wound leakage by injecting BSS through the paracentesis site, and applying fluorescein or watching the wound carefully under high magnification to see if there is any leakage. If there is no leakage, but the bleb is very large, this can be handled in two ways. The easiest way is to apply a compression suture. This involves passing an 8-0 nylon suture (spatula needle) through conjunctiva, Tenon’s, and episcleral tissue at a point posterior to the bleb, then running the suture across the bleb and passing the needle again through clear cornea at three-quarter depth just central to the limbus and then tying the suture tight to itself to compress the bleb. Extremely large blebs may require two compression sutures running parallel in a similar manner. Horizontal sutures to block posterior flow can also be added. The second way to treat overfiltration is to reopen the conjunctiva and apply more 10-0 nylon sutures to the scleral flap until watertight. This should be checked repeatedly using BSS through the paracentesis to document that the eye can hold the high pressure (greater than 20 mm Hg) before closing the conjunctiva back down. Be sure to close the conjunctiva watertight as well. Do not forget to allow aqueous out through the paracentesis site to titrate pressure back into the low teens at the end of the case. Also, be prepared for the probability of needing suture lysis postoperatively.
If, however, the patient is found to be Seidel positive in the operating room, then a more difficult decision has to be made—whether or not to simply apply more conjunctival sutures until the patient is Seidel negative, or whether to reopen the conjunctiva, make the scleral flap watertight, and then close the conjunctiva again. Although it is tempting to just apply conjunctival sutures, if the eye has been hypotonous, and especially if choroidals are present, it may be best to go ahead and close down the scleral flap so that one can be certain that postoperative hypotony will be cured. Then the scleral flap sutures can be lasered as needed.
Occasionally, patients with a very thin scleral flap, or poor approximation of the scleral flap, will continue to leak in spite of abundant 10-0 nylon sutures. Sometimes they will even leak through needle tracks (especially with thin scleral flaps). These patients often require either a Tenon’s patch graft or a tudoplast graft (preserved pericardium) to close off the leaking scleral fistula. In either case, the tissue is simply sutured to bare sclera to cover the area of leakage. Conjunctiva is then reapproximated and closed. If there is insufficient conjunctival tissue for closure, a conjunctival graft will be needed.
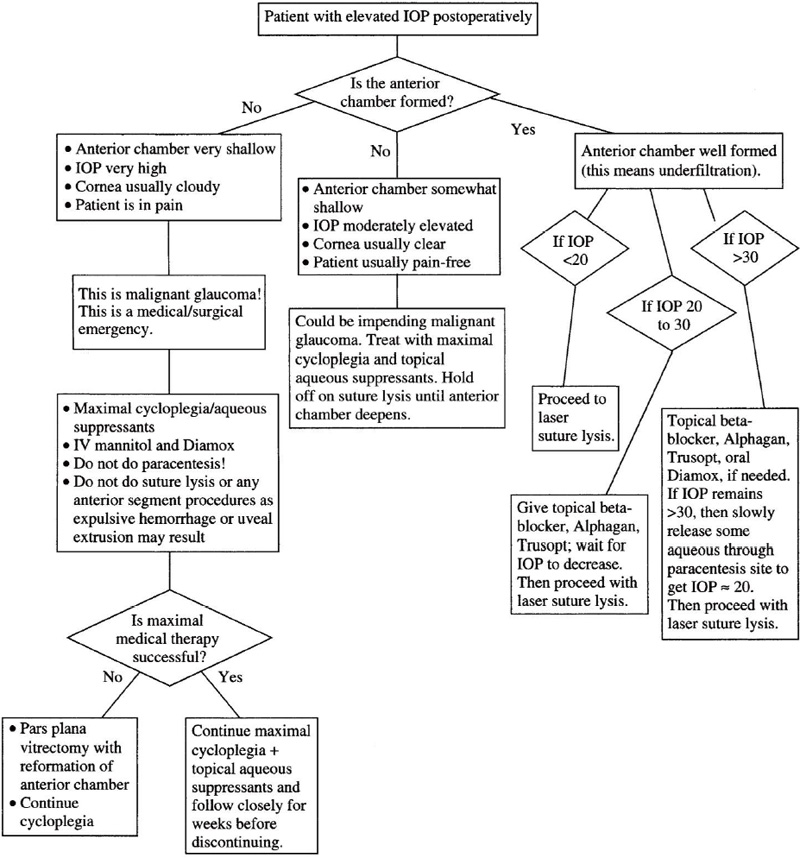
Figure 19–3. Management of a patient with elevated IOP postoperatively.
What If the IOP Is Too High During the First Week?
If the anterior chamber is collapsed and the IOP is very high, then the patient may have malignant glaucoma (Fig. 19–3). These patients are treated with maximal dilation and cycloplegia, maximal medical therapy including mannitol, and often still require pars plana vitrectomy. If the anterior chamber is shallow but not collapsed, the patient may have extensive PAS from prolonged hypotony and will require an attempt at angle reconstruction with viscoelastic, as well as surgical reevaluation of the trabeculectomy site.
If the anterior chamber is deep (i.e., no malignant glaucoma) then the patient is underfiltering. Laser suture lysis should be attempted until the desired effect is achieved. If the pressure is very high, then it might be safer to reduce pressure prior to suture lysis. This is attempted medically first, but a 27-gauge needle can be used (bevel up) through the paracentesis site to slowly “burp” aqueous from the anterior chamber if medical therapy is insufficient or too slow.
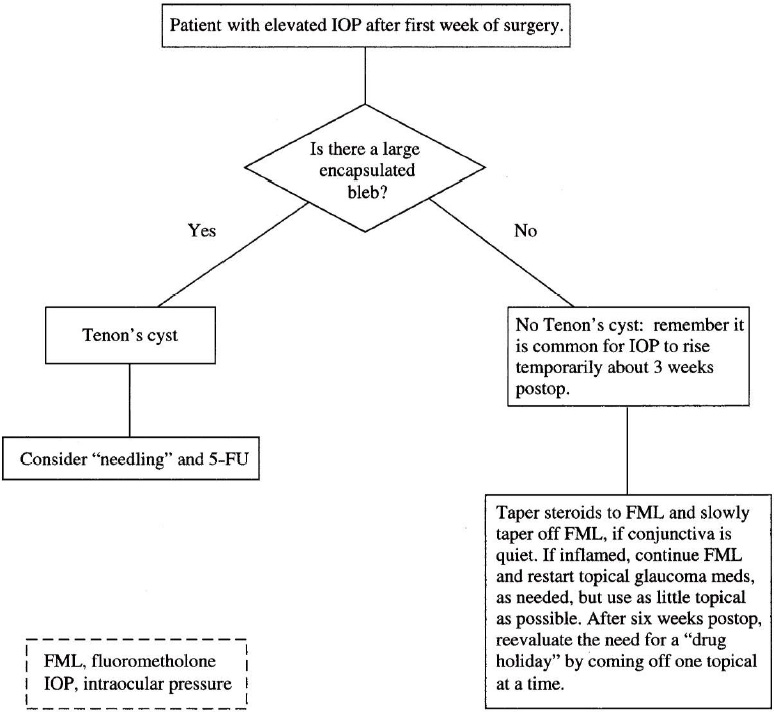
Figure 19–4. Management of a patient with elevated IOP after first week of filtration surgery.
|
How Is Elevated IOP Managed After the First Week?
Consider that the patient may be a steroid responder, and begin tapering steroids (Fig. 19–4). Because most patients only need conjunctival treatment rather than intraocular treatment, it is reasonable to change from Pred Fort 1% to FML 0.1% rather early postoperatively. If a Tenon’s cyst is developing, and pressure is inadequately controlled with medication, then proceed with needling of the bleb and subconjunctival 5-FU injection near, but not into, the bleb (Table 19–5).
What About Cycloablative Procedures?
These procedures (Table 19–2) are only indicated if all other avenues fail. They reduce IOP by destroying the ciliary body and consequently decreasing the production of aqueous humor. Various types of laser therapies and a cryo procedure are available (Table 19–2). The former more commonly are associated with fewer complications than the latter (see Chapter 22).
In transpupillary (direct) laser cyclophotocoagulation, more controlled destruction of the ciliary epithelium is possible as compared to transscleral laser procedure.42 Most patients require retro- or peribulbar anesthesia for comfort during this surgery. The 3 and 9 o’clock meridians are avoided to prevent damage to the long posterior ciliary arteries. Laser energy parameters are variable and depend on the nature of the laser material. Complications may also be minimized by treating 270 degrees or less of the ciliary epithelium. The effect on IOP may be dramatic, though many patients require repeat treatments. Most (60 to 70%) end up with pressures of 22 mm Hg or lower.42–44 Complications include pain, hemorrhage, reduced visual acuity, uveitis, and phthisis bulbi.
Uram45 introduced endoscopic cyclophotocoagulation in the treatment of glaucoma. He reported a 57% decrease in IOP in patients undergoing combined cataract and glaucoma surgeries
Future Considerations
As previously mentioned, nonpenetrating trabeculectomies and adaptations of shunt devices will be important future considerations. The nonpenetrating trabeculectomies especially sound promising and may become a more common form of glaucoma surgery in the future.
Endoscopic laser cyclodestructive procedures may gain popularity, especially in combined cataract cases as technology advances. Even still the “traditional” guarded trabeculectomy should increase in frequency as the population ages. Planned postoperative suture lysis should also increase in frequency as the benefits of this modification become better known.
Acknowledgments
In that this chapter is mostly a compilation of what I have learned from others, I would like to thank all of those who came before. In particular, I thank my mentors: Dr. Thom Zimmerman, Dr. George Nardin, Dr. Bernard Schwartz, and Dr. M. Bruce Shields.
References
10. Ainsworth JR, Jay JL: Cost analysis of early trabeculectomy versus conventional management in primary open angle glaucoma. Eye 1991;5:332–338.
31. Sugar HS: Experimental trabeculectomy in glaucoma. Am J Ophthalmol 1961;51:623–627.
32. Cairnes JE: Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968;5:673–679.
33. Shields MB: Textbook of Glaucoma. Baltimore: Williams & Wilkins, 1987;466–471.
40. Khoury JM, Joos KM, Shen JH, et al.: Half corneal light shield as a delivery system for standardized application of mitomycin C. J Glaucoma 1998;7:8–11.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree