Prevention of Ocular Infections
Kirk R. Wilhelmus
Infections and postinfectious complications account for part of the world’s avoidable blindness.1,2 The prevention of ocular infection emerged during the nineteenth century, beginning with the use of handwashing and silver nitrate eyedrops to prevent ophthalmic neonatorum (Table 63.1) and of aseptic technique and antiseptic agents to prevent postoperative endophthalmitis.3 Improved knowledge of infectious disease pathogenesis allows many other preventive strategies to reduce microbial transmission and to save sight.2
TABLE 63.1. Effect of prophylaxis for acute neonatal conjunctivitis. (Leipzig, 1874–1882)* | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Levels of Prevention
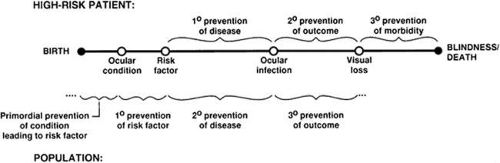
The prevention of ocular infections can occur at multiple levels (Table 63.2). Primary prevention averts exposure to an infectious agent or reduces the acquisition of infection through immunization or by antimicrobial prophylaxis given before (e.g., preoperatively) or after (e.g., postnatally) exposure to microorganisms. Secondary prevention aims to intervene during early infection. Tertiary prevention corrects visual impairment caused by infectious eye disease.
TABLE 63.2. Levels of prevention in ophthalmic epidemiology. | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Prevention strategies can be classified from the perspective of the individual or the community (Fig. 63.1). Policy decision makers in public health ophthalmology must judge the relative advantages and shortcomings of available options (Table 63.3). Preventive strategies that reduce the burden of ocular infections often call for multiple levels of prevention.4,5,6,7,8
TABLE 63.3. Strategies in preventive ophthalmology. | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Primary Prevention
Universal Precautions
Universal precautions involve hand cleansing, disinfection, avoidance of injury, and barrier protection.9,10 Contact instruments must be disinfected between patients. Contact lenses used for fitting patients should be disinfected by heat or hydrogen peroxide. Tonometer tips should be wiped clean and disinfected with isopropanol, diluted bleach, or hydrogen peroxide. Eyedropper tips should not touch the patient’s ocular surface or tear film. Multiuse ophthalmic solutions can be discarded periodically or replaced with unit doses.
Sanitation
Hygiene is a basic element of preventive ophthalmology. Hand washing using liquid soap dispensers, antiseptic solutions, or alcohol hand rubs reduces skin flora and should be a routine practice in the eye clinic.11,12 The use of disposable gloves or fingerlings or a no-touch technique with disposable applicator sticks is recommended to manipulate the eyelids when examining infected eyes.13 Special precautions are needed during office outbreaks of communicable ocular infections.14,15 Door handles, telephones, and other shared devices in waiting areas offer opportunities for improved design.
On a global scale, most eye infections occur in less developed regions where haphazard urbanization without a sanitary infrastructure breeds infectious outbreaks. Improving crowded, dirty living conditions among the economically disadvantaged can reduce the incidence of infectious eye diseases.16,17 Better hygiene and cleaner water supplies reduce the occurrence of eye diseases such as trachoma.16,18 Using insecticides and taking other precautions to repel flies and to avoid insect bites help to prevent trachoma and vector-transmitted diseases in endemic areas. International agencies that accelerate economic development make a large impact on a society’s ocular health.19
Segregation
The identification of infected patients permits reducing their direct and indirect contact with susceptible persons. Formerly, quarantine, deportation, and restricted immigration were used to exclude people with suspected contagious diseases (Fig. 63.2). Precautions must also, however, protect the privacy and rights of individuals. In the eye care setting, segregating patients with symptomatic conjunctivitis to a designated area and deferring nonessential procedures such as tonometry can avoid an office outbreak.20 Counseling those with a communicable ocular infection aims to minimize risky behavior and the number of contacts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree