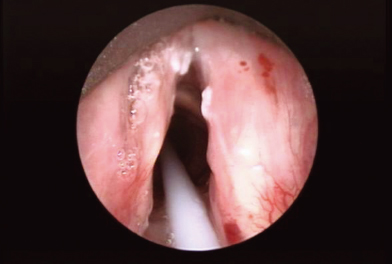
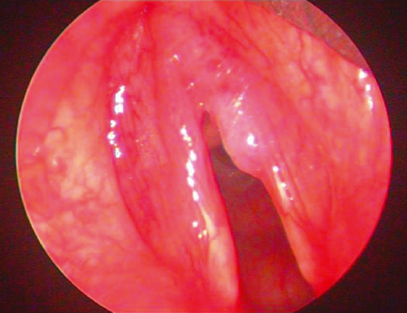
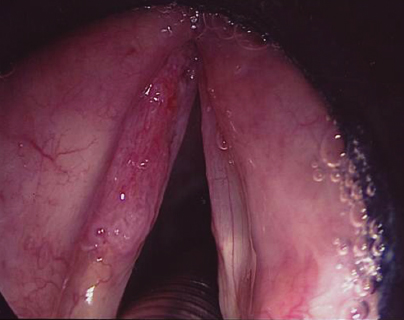
26 Premalignant Lesions of the Larynx Exactly 43 years after Durant described the first documented case of laryngeal leukoplakia as “white cicatrices” adjacent to a malignant laryngeal lesion,1 Jackson in 1923 conceptualized premalignancy of the larynx as akin to “a large number of citizens leaving their regular daily routine and mobilizing preparatory to invasion.”2 In 2008, cancer of the larynx accounted for 1.2% of all new malignancies diagnosed worldwide and was responsible for 82,000 deaths.3 The best chance of curing any cancer is via its early detection and eradication as morbidity and mortality are proportionately related to stage.4 The former is pertinent to the larynx, as laryngectomy is a devastating consequence for many patients in the curative treatment of advanced laryngeal cancer. Thus, appropriate management of precancerous laryngeal lesions in those patients fortunate enough to present at this stage is obviously vital. A cancerous lesion is a culmination of multiple genetic changes leading to the selection of a clonal population of cells that have broken free from local host-specific growth control mechanisms.5 Classifying the morphological correlates of this sequence of events has generated much debate among pathologists and the wider scientific community. Classification schemes are only useful if they provide prognostic information and can thus impact on subsequent management. In 1952, Kleinsasser devised a systematic classification for precancerous lesions of the laryngeal squamous epithelium. There were three tiers that sequentially progressed as follows: simple squamous cell hyperplasia, hyperplasia with atypia, and finally carcinoma in situ (CIS).6 Numerous classification schemes have evolved from this fundamental premise, but to date none have found universal acceptance. Currently, two are prominently used throughout the world (discussed later). Much focus in recent years has been placed on the molecular events characterizing laryngeal precancerous lesions, aiming to enhance the predictability of the fairly subjective morphological criteria that govern these existing schemes.7 The larynx serves to protect the airway and to commence vocalization and provides the ability to generate raised intrathoracic pressure as in a Valsalva maneuver. These vital functions may all be compromised by overaggressive treatment of preneoplastic lesions, some of which may ultimately even regress.8 This chapter discusses the presentation, aspects of diagnosis including the aforementioned histological difficulties, and principles for managing preneoplastic laryngeal lesions. While the detailed functional anatomy and physiology of the larynx are discussed elsewhere, an appreciation of macro and microanatomy is necessary for understanding surgical management. The larynx may be grossly divided into the supraglottis, the glottis, and the subglottis, separated respectively and arbitrarily by two horizontal lines: one passing through the level of the apices of the laryngeal ventricles and another at 1 cm below the free edge of the vocal folds. Within the glottis lie the true vocal folds that extend anteriorly from the vocal processes of the arytenoid cartilages to form a confluent attachment at the inner surface of the junction between the laminae of the thyroid cartilages (the anterior commissure). The posterior commissure lies between the arytenoid cartilages and is limited posteriorly by the mucous membrane bridging them. The rima glottidis is the triangular airspace between the vocal folds anteriorly and the vocal processes and the base of the arytenoid cartilages posteriorly. Being the narrowest section of the upper airway, it affords most resistance to airflow and thus airborne carcinogens. This is perhaps one of the reasons why the glottis and in particular the vocal folds are the commonest sites of laryngeal carcinoma and indeed preneoplastic lesions. Although the vocal folds constitute two-thirds of the length of the rima glottidis, the wider posteriorly located interarytenoid space has a much larger area through which most of the volume of air passes during respiration. The vocal folds and their intervening space are responsible for creating the necessary vibratory cycles for phonation. The anterior commissure is an important surgical landmark. It may be difficult to access and incomplete visualization often leads to uncertainty in the complete surgical clearance of any disease sited here. It is also a source of significant postoperative morbidity if inappropriately managed. The anterior commissure comprises the convergence of the vocal ligaments with the thyroepiglottic ligaments from either side. These ligaments ultimately unify to form the anterior commissure tendon (Broyles ligament), which is a thick gland-free region that resists tumor spread. However, superior and inferior to the Broyles ligament, the glottic mucosa reflects onto bare thyroid cartilage which at this point is devoid of inner perichondrium. It is here that the tumor may easily invade the thyroid cartilage to significantly upstage disease. The mucosa covering the larynx consists of two types. Stratified nonkeratinizing squamous epithelium lines the vocal folds and much of the epiglottic surface, signifying their position in areas that are subjected to repetitive abrasive forces, that is, contact of the vocal folds upon closure of the rima glottidis in the former case. The remainder of the laryngeal surface is covered by ciliated columnar respiratory epithelium. Squamous carcinoma of the larynx commonly occurs at the transition between the squamous and respiratory epithelium on the ventricular surface of the true vocal folds (the inferior arcuate line). Mucinous glands are found in the saccule of the ventricles (which are guarded by the false vocal folds), the laryngeal surface of the epiglottis, and the infraglottic surface of the vocal folds. The free edge is void of glands needing to remain smooth to optimize its ability to oscillate during the phonatory cycle. The vocal folds are also largely devoid of lymphatics and thus cervical lymphadenopathy for early-stage glottic carcinoma is relatively rare. The level of the rima glottidis is a watershed that marks the junction of the different embryological origins of the superior and inferior larynx. The vast majority of surgical procedures on preneoplastic laryngeal lesions will involve the vocal folds. It is thus important to understand their layered histological structure to minimize functional damage. Nonkeratinizing squamous epithelium lines the surface. The lamina propria lies deep to this and is divided into the superficial (Reinke space, which consists of fluid amorphous material), intermediate (elastic fibers), and deep (firm collagenous fibers) layers. The intermediate and deep layers form the vocal ligament. Deeper still lies the vocalis muscle. Functionally, the vocal fold acts as three layers: the cover (squamous epithelium and superficial layer of the lamina propria) slides and vibrates on the transition zone (intermediate and deep layers of the lamina propria) and the body (the vocalis muscle). A variety of malignant neoplasms may arise in the larynx (Table 26.1), reflecting the different tissues from which they originate. The vast majority, however, are squamous carcinomas (up to 95%) and predominantly arise on the true vocal folds. All other histological subtypes will necessarily develop via a premalignant phase, but due to the paucity of such cases in the literature they have not been studied and characterized to the same extent as premalignant squamous carcinomatous lesions. The remainder of this chapter will therefore focus on the latter. Histologically, neoplasms that do not fulfill the criteria for frank malignancy are referred to as dysplastic. Lesions are dysplastic when there is evident cytological and tissue architectural atypia without invasion. CIS lies at the extreme end of the dysplastic spectrum, where morphological features of malignancy are displayed by an epithelial lesion that has not yet breached the underlying basement membrane.9 Laryngeal dysplastic epithelium manifests clinically in three main forms: leukoplakia (white patches), erythroplakia (red), and mixed leukoerythroplakia (speckled).9 Leukoplakia (Fig. 26.1) represents keratin production (which is not normally produced by laryngeal squamous epithelium), whereas erythroplakia (Fig. 26.2) indicates enhanced vascularity. Although keratinization is the histological counterpart of leukoplakia, its extent does not correlate with the underlying degree of dysplasia. Indeed the rare purely erythroplakic area, although clinically less impressive than a thickened, raised patch of leukoplakia, has a much higher chance of representing severe dysplasia/CIS.10 Some clinical features are indicative of high-risk epithelium: erythroplakia, surface granularity, large surface area; but in general clinical correlation (Figs. 26.1 to 26.3) with the underlying state of the epithelium is relatively poor.7,11 For this reason a biopsy is mandatory in all suspected cases. Most dysplastic squamous epithelial lesions arise on the true vocal folds, but they may occasionally be found in other laryngeal subsites normally covered with squamous epithelium (e.g., the epiglottis) or in areas of squamous metaplasia that usually occur as a consequence of repeated physical insult. Table 26.1 Histological Subtypes of Laryngeal Malignancies
Anatomy
Definitions and Histology
• Squamous carcinoma ○Histological variants: verrucous, spindle, and basaloid • Mucoepidermoid • Adenoid cystic • Sarcomas ○Rhabdomyosarcoma ○Chondrosarcoma • Lymphoma • Neuroendocrine ○Carcinoid ○Small cell |
Dysplastic epithelium represents an increased risk of malignant transformation compared with nondysplastic epithelium.8 However, the term dysplasia covers a broad range of morphological atypia that do not always lie neatly on a spectrum from normal epithelium to CIS. There have been numerous attempts at grading such changes ever since Kleinsasser’s landmark work.12 The ideal grading system should have prognostic value regarding the risk of malignant transformation and demonstrate good interobserver and intraobserver reproducibility. Unfortunately, nearly 60 years and over 24 attempts later, such a morphological grading system does not exist. Thus, laryngeal dysplasia remains one of the most hotly debated subjects within head and neck pathology. The two major grading systems for laryngeal dysplasia in use in the United Kingdom are the World Health Organization and the Ljubljana classifications.13
The WHO classification has three dysplastic categories: mild, moderate, and severe, straddled on either side by hyperplasia and CIS. Squamous hyperplasia here simply represents an increased number of cells that may occur in the spinous layer (acanthosis) or in the parabasal/basal layers (basal cell hyperplasia). There is no cellular atypia or architectural disturbance, although there is often a degree of superficial keratin formation. Histological features found in dysplasia, which suggest malignant potential, include abnormal mitotic figures, in terms of both morphology and numbers, nuclear pleomorphism, and stromal inflammation.
Mild, moderate, and severe dysplasia represent a spatial increase in dysplastic epithelium, with cytological and architectural disturbance limited to the lower one-third (basal/parabasal), the lower two-thirds, and extending throughout the epithelium, respectively. The degree of cytological atypia also increases with increasing grade. By these definitions, the distinction between severe dysplasia and CIS is somewhat blurred and indeed many pathologists and clinicians manage these entities similarly.14 The WHO classification evolved from the classification for lesions of the cervix, that is, cervical intraepithelial neoplasia (CIN), with the laryngeal adaptation for CIN 1, 2, 3 replaced by squamous intraepithelial neoplasia (SIN) 1, 2, 3.15 Kambic and Lenart in 197116 felt that this categorization did not divide patients with laryngeal dysplasia into distinct prognostic groups, and their own adaptation was further modified by a working group on head and neck pathology from the European Society of Pathology in 199717 to form the Ljubljana classification, which in essence is a two-tier classification of laryngeal dysplasia. Abnormal laryngeal epithelium is subcategorized as follows: (1) basal/parabasal hyperplasia (minimal risk of malignant transformation) or (2) atypical hyperplasia or “risky” epithelium, featuring cellular atypia which does not span the entire width. Simple squamous hyperplasia in the Ljubljana classification is confined to the spinous layer, whereas CIS is defined as “full-thickness” atypia without invasion, thus overlapping with the WHO’s “severe dysplasia” and is prognostically significantly different from the other categories. Table 26.2 summarizes the two classification schemes.
There is no easy overlap between these and other classification systems, but dichotomous systems such as the Ljubljana classification or indeed dichotomizing the WHO classification system (e.g., severe/CIS versus mild/moderate) appears to be far better in reliability studies.18 This indicates the relative uncertainty of categorizing middle-grade or “moderate” dysplasia. As expected, agreement reliability for any particular grading system improves following group training sessions.17 The importance of accurate histological grading cannot be stressed enough, as it is the single most important determinant of subsequent patient management.
Table 26.2 Comparison of Two Popular Classification Systems Used for Premalignant Laryngeal Epithelium
The WHO Classification (2005) | The Ljubljana Classification |
• Squamous cell hyperplasia | • Squamous cell (simple) hyperplasia |
• Dysplasia ○Mild dysplasia ○Moderate dysplasia ○Severe dysplasia | • Abnormal epithelium ○Basal/parabasal cell hyperplasia ○Atypical hyperplasia (“risky” epithelium) |
• Carcinoma in situ | • Carcinoma in situ |
Clinical Insight
The senior author (K.G.) maintains a close collaboration with dedicated head and neck pathologists to ensure consistency of pathology reporting. These patients can be challenging and multidisciplinary meetings allow concerns regarding the nature of laryngeal dysplasias to be voiced in the context of a patient’s clinical condition, comorbidities, and risk factors, all of which influence future management.
Epidemiology
There is a paucity of epidemiological data on preneoplastic laryngeal lesions. However, the incidence of frank laryngeal malignancy varies throughout the world, presumably as a consequence of exposure to differential quantities and types of carcinogenic agents. The nature of the carcinogenic insult will also determine the site of the lesion within the larynx. Thus inhaled smoke, to which most resistance occurs at the glottis, is most likely to cause vocal cord lesions, whereas supraglottic lesions are more likely to result from ingested carcinogens such as alcohol.19 In the United Kingdom, the age-standardized incidence of laryngeal carcinoma for men was 5.3/100,000 and for women 1/100,000 in 2005.19 The male to female ratio is likely to decline, however, due to the relative increase in female smokers of late. As with most other carcinomas, the incidence increases with age. In one of the largest single-center series of leukoplakic lesions of the larynx, comprising a total of 1268 patients, the male to female ratio was 4.6, but women developed pathology at an earlier age (mean 44.8 VS 51.5 years). Here, the overall incidence, based on the catchment area of the host institute, was 2.61/100,000 for simple hyperplasias and 0.86/100,000 for atypical hyperplasias.7
Etiology
The risk factors for laryngeal dysplasia will necessarily be the same as that of laryngeal carcinoma. Laryngeal neoplasia is a preventable disease in the vast majority of cases, implicating environmental factors in causation. The strongest association is with tobacco smoking. Burning cigarettes releases tar that contains carcinogenic polycyclic aromatic hydrocarbon compounds. These are degraded into intracellular chemicals that bind to and damage DNA and RNA molecules. Several observational studies report a dose-dependent increase in the risk of laryngeal cancer with tobacco smoking.20 Alcohol and smoking appear to act synergistically to enhance the risk of laryngeal cancer,21,22 although as mentioned above, patients whose predominant risk factor is alcohol are more likely to develop supraglottic carcinoma.23 Although alcohol, like cigarette smoke, directly instigates carcinogenic pathways, concurrent malnutrition, including defective vitamin status, is also likely to play a significant role.24
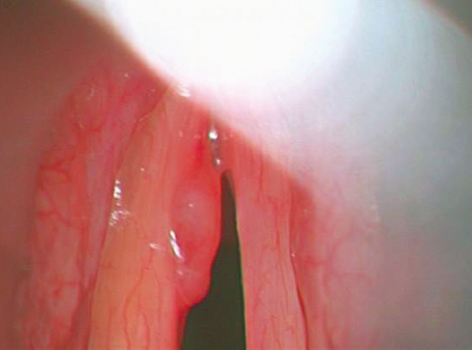
There is a growing and convincing body of evidence implicating human papillomavirus (HPV) in oropharyngeal carcinomas.25 HPV-positive and HPV-negative cancers in this site appear to be different clinical entities, with distinct prognoses.26 As with squamous carcinoma of the cervix, serotypes 16 and 18 appear to be the most carcinogenic. This HPV-positive versus HPV-negative carcinoma dichotomy is not as clear-cut in the larynx. The prevalence of HPV in laryngeal carcinoma specimens varies from 0 to 58%, depending on the population and method of detection utilized, with an overall reported prevalence of around 25%.7 A recent systematic review revealed only a weak correlation between HPV and laryngeal carcinoma.25 Serotype 16 is the most commonly isolated subtype. In contrast, the serotypes most prevalent in recurrent respiratory papillomatosis are 6 and 11. Recurrent respiratory papillomatosis (Fig. 26.4) may rarely transform into squamous carcinoma, particularly if patients have been irradiated, but these two disease entities are thought to have different mechanistic origins.27 It should be noted that HPV has been detected in up to 25% of individuals with clinically and histologically normal laryngeal epithelium.28
That chronic laryngopharyngeal reflux may play a role in laryngeal carcinoma was first highlighted by Olson in 1983.29 Several uncontrolled case series report high prevalences of gastroesophageal reflux disease (GERD) in patients with laryngeal carcinoma.30 However, given the relatively high prevalence of GERD in the general population, it is difficult to attribute a direct etiological role. Larger sample sizes, with well-matched controls, are necessary for further clarity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree