Fig. 8.1
Corneal vascularisation with graft failure secondary to graft rejection. Vascularisation of the recipient corneal bed is the most significant single risk factor for graft failure on multivariate analysis in all published reports (Reproduced from Niederkorn and Larkin [1], with permission of Informa Healthcare)
Inflammation is also an independent variable associated with corneal graft failure due to rejection. Using immunohistochemical staining analysis in 107 recipient corneas, Williams et al. found an inverse relationship between leucocyte counts in the graft bed and 3-year actuarial graft survival [20]. Hence, corneal transplantation is best avoided in an actively inflamed eye where possible, although it is important to note that even a history of inflammation alone without activity at time of transplantation results in a less favourable 5-year graft survival of 64 % compared to 91 % in an eye without any history of inflammation and 56 % in an eye without a history of inflammation but active inflammation at time of transplantation [16].
A previously rejected corneal graft implies allosensitisation with relative loss of immune privilege and has been demonstrated to increase risk of rejection in a subsequent allograft, even if the recipient cornea is avascular [22]. The number of preceding transplants in the recipient eye is also a prognostic factor for graft survival, with decreasing graft survival rates for subsequent allografts.
Other factors that have been shown to increase the risk of rejection include grafts in children, large-diameter grafts [25, 26] and the presence of atopy [27, 28]. The presence of non-ocular atopic disorders, even in the absence of clinically evident conjunctival allergy, appears to confer a higher risk of graft rejection. The mechanisms underlying this are not fully understood. However, patients with atopic dermatitis have been shown to have a poorer graft prognosis [27, 29, 30], and murine asthma models have also demonstrated that airway allergen exposure alone increases corneal allograft rejection risk [31]. Studies of corneal transplantation in the setting of allergic conjunctivitis have demonstrated an increased incidence and swifter tempo of graft rejection and the presence of an eosinophilic component in the alloreactive effector population of rejected grafts that is only found in atopic graft recipients [28, 32].
Post-transplant events can also lead to subversion of immune privilege and hence increase the risk of rejection. Loosened sutures, suture-related infections and herpetic infection recurrence are local episodes of alloantigen-independent inflammation that lead to recruitment of alloreactive cells, angiogenesis, lymphangiogenesis and upregulation of MHC molecules on graft cells [1, 33]. This combination of events can lead to an acute-onset rejection response, which must be recognised early and promptly treated.
Clinical Features of Graft Rejection
In 1948, Paufique and colleagues used the term maladie du greffon (disease of the graft) to describe clouding of the graft after an initial period of clarity [34]. In 1969, Khodadoust and Silverstein demonstrated that each layer of the cornea – epithelium, stroma and endothelium – could manifest a rejection reaction [35]. The incidence of corneal allografts experiencing a rejection episode at some stage following transplantation has been reported as ranging from 18 to 21 % in large cohorts of graft recipients [36, 37].
Epithelial rejection is characterised by the presence of an elevated linear opacity that stains with fluorescein and often progresses from the periphery to the centre of the graft over the course of several days to a few weeks. The average onset of an epithelial rejection line was 3 months’ post-transplantation with a frequency of 10 % in one series [38]. Stromal rejection is characterised by nummular subepithelial infiltrates, similar to those found in adenoviral keratitis (Fig. 8.1a). They can be seen concurrently with an epithelial or endothelial rejection line. Its average onset was reported to be 10 months’ post-transplantation with a frequency of 15 % [38, 39]. Patients with epithelial and stromal rejection may be asymptomatic or have only mild ocular discomfort.
In contrast, patients with endothelial rejection tend to be more symptomatic and may present with visual disturbance and/or symptoms consistent with anterior chamber inflammation. If examined early, there may only be cells in the anterior chamber without any flare or graft abnormality. This will then be followed by aggregated alloreactive cells adherent to graft endothelium as keratic precipitates, the presence of an endothelial rejection line and an area of localised graft oedema (Fig. 8.1b) [35, 40, 41]. The average onset of endothelial rejection has been reported to be 8 months’ post-transplantation with a range of 2 weeks to 29 months, although unequivocal endothelial rejection has been observed as late as 9 years’ post-transplantation [38, 41]. A rejection episode results in loss of donor endothelial cells, which are critical for maintenance of corneal transparency. As human endothelial cells do not repair by mitosis, endothelial decompensation may ensue if the cell density is reduced at rejection below the threshold necessary to prevent stromal swelling. This may happen at the time of an irreversible acute graft rejection or manifest at an interval following one or more rejection episodes that were reversed with treatment. Risk factors for significant endothelial cell loss include a delay in presentation of more than 1 day between onset of symptoms and initiation of treatment and recipient age of greater than 60 years [42].
Pachymetry is useful in detecting an increase in oedema and deturgescence following the initiation of steroid treatment. Naacke et al. reported that apart from preoperative diagnosis, the only other factor found to be significantly associated with reversibility of graft rejection was graft thickness at time of rejection diagnosis [43]. The Collaborative Corneal Transplantation Study Group also reported that 49 % of eyes had an increase in corneal thickness of at least 10 % in association with the development of a rejection episode, and the likelihood of graft failure was predicted by a larger increase in thickness at 1, 3 and 6 months [44].
Management of Corneal Transplant Rejection
Treatment of Rejection
The leading cause of graft failure is immunological graft rejection. It is important to promptly recognise the clinical features and initiate treatment, as a delay in diagnosis and treatment adversely affects graft prognosis.
Treatment with intensive topical corticosteroid, such as dexamethasone 0.1 %, is successful at reversing most endothelial rejection episodes. In cases where topical steroids fail to reverse rejection, this has been attributed to the failure of the topical steroid to reverse effector components of the allogeneic response or a delay in recognition and initiation of treatment with resultant significant endothelial cells loss, ultimately leading to graft failure [42].
Regarding additional systemic steroid, Hill et al. found that a single intravenous pulse of methylprednisolone was more effective than oral prednisolone in reversing rejection in patients who presented with endothelial graft rejection within 8 days of symptom onset. Patients were also significantly less likely to undergo a further rejection episode if the graft survived, with 67 % of the oral cohort and 26 % of the intravenous cohort experiencing further episodes of rejection [45]. A second pulse of intravenous methylprednisolone given 24 h or 48 h later did not demonstrate any advantage in addition to that of a single dose at diagnosis [46].
However, a subsequent prospective randomised trial by Hudde et al. did not demonstrate a statistically significant benefit in receiving a single intravenous methylprednisolone pulse in addition to intensive local corticosteroid in terms of reversal of the rejection episodes, later recurrence of graft rejection or graft failure with a follow-up duration of 2 years. The intensive local corticosteroid regime used in that study consisted of one dose of subconjunctival betamethasone (2 mg) and hourly dexamethasone 0.1 % for 24 h [47]. Another study reported a higher rate of rejection reversal in patients receiving subconjunctival triamcinolone (20 mg) versus a single dose of intravenous methylprednisolone in addition to topical prednisolone acetate 1 % [48]. Successful reversal of an endothelial rejection episode ranges from 51 to 92 % [43, 47].
Other studies have examined the use of topical [49, 50] and systemic [51] cyclosporine in the treatment of endothelial rejection: Poon et al. in a prospective randomised trial did not find a significant benefit in using a commercially available preparation of topical cyclosporine (0.05 %) in addition to intensive topical steroids [49].
Prevention of Corneal Transplant Rejection
Patients with Low Rejection Risk
In patients without risk factors for graft rejection identified prior to transplantation, typical post-operative immunosuppression consists of dexamethasone 0.1 % or prednisolone acetate 1 % four times daily for the first 2–3 months, reducing gradually to zero by 6–12 months following transplantation. There are no definitive randomised controlled trials into the optimal immunosuppression regime for low-risk grafts, although there is remarkable consensus worldwide regarding the need for prophylaxis post-operatively with topical corticosteroid as demonstrated by surveys of practice patterns [52–54].
Koay and colleagues in their survey of corneal surgeons in the Bowman Club in the United Kingdom reported that all surgeons used topical steroids post-operatively, with 50 % favouring prednisolone acetate 1 % and 36 % favouring dexamethasone 0.1 %. Average duration of topical treatment was 8.7 months, although 5.5 % of respondents continued treatment indefinitely in low-risk grafts [52]. This is in stark contrast to that reported by Price and colleagues, who surveyed 250 corneal surgeons attending an endothelial keratoplasty course at a tertiary referral centre between 2006 and 2008; the majority (87 %) of whom were from the United States. They reported that 46 and 22 % of respondents continued topical steroids indefinitely for pseudophakic/aphakic and phakic patients, respectively, in low-risk grafts [55].
Price and colleagues also found that the majority (76 %) of respondents used intraoperative corticosteroids, of which 72 % were delivered as sub-tenon or subconjunctival injections, 8 % were intravenous, 7 % were oral and 2 % were intraocular. Again, all surgeons used topical steroids post-operatively, with 95 % using prednisolone acetate 1 %. Most surgeons (57 %) used the same regimen regardless of lens status. However, 14 % of respondents who initially prescribed prednisolone acetate 1 % for phakic patients had switched to a lower-strength corticosteroid such as fluorometholone or loteprednol at 6 months, and 20 % had withdrawn their patients’ topical steroid. In contrast, 10 % of respondents had switched their pseudophakic/aphakic patients to a lower-strength steroid, and 10 % had withdrawn topical steroids [55].
Nguyen and colleagues in a recent prospective randomised trial of 406 eyes following normal-risk keratoplasty reported significantly higher rejection rates in grafts where topical steroids were stopped at 6 months (9.1 %) compared to 12 months (4.9 %) [56]. The use of topical cyclosporine 0.05 % four times daily for 1 year has also been undertaken and found to be significantly less effective than historical controls using topical corticosteroid for a median of 7 months as rejection prophylaxis in low-risk grafts [57].
Patients with High Rejection Risk
There is much less consensus on the post-operative management of grafts with high rejection risk (Fig. 8.2). Due to the shortage of large comparative prospective studies into immunosuppression regimes, different centres use varying protocols based on individual clinical experience and informed by experimental evidence, small uncontrolled or retrospective clinical studies and extrapolation from what has proven effective in solid organ transplantation. This is compounded by the lack of a consensus definition of what constitutes a “high-risk” graft, which also makes direct comparison between studies difficult. Some reports include risk factors for graft failure independent of rejection as part of their “high-risk” definition, and others include a subset of patients who received HLA-matched donor corneas, a factor that may independently affect transplant outcomes with respect to rejection.
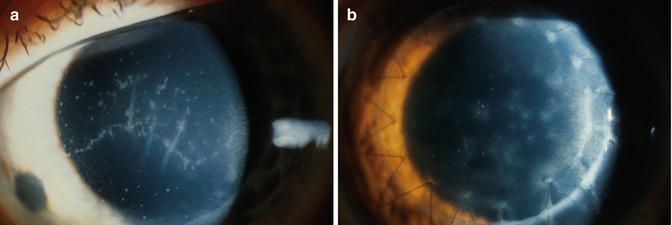
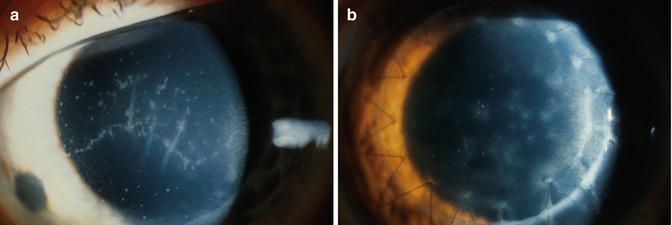
Fig. 8.2
(a) Endothelial rejection. A horizontal endothelial line, scattered keratic precipitates and Descemet membrane folds are shown. (b) Stromal rejection. Scattered anterior stromal infiltrates shown are restricted to donor cornea (Reproduced from Larkin [41] with permission of BMJ Publishing group)
Furthermore, as corneal transplantation is not a life-saving procedure, ophthalmologists are hesitant to commit patients to long-term systemic immunosuppression due to the potential side effects and risk of developing malignancies. However, in cases where there is a high rejection risk and patients are reliant on graft survival in order to undertake activities of daily living, the risks of systemic immunosuppression may be more justifiable.
Both topical and systemic immunosuppressive agents have been evaluated for prophylaxis against graft rejection in high-risk grafts. However, systemic rather than local administration is justified by evidence in experimental models that alloantigen immunisation does not occur in the eye, but that transported corneal alloantigens lead to clonal expansion of alloreactive T lymphocytes in regional lymph nodes and possibly spleen [58–60].
The majority of reports on systemic immunosuppression as prophylaxis against corneal allograft rejection utilise one of the calcineurin inhibitors, cyclosporine and tacrolimus, as monotherapy. This is in contrast to renal transplant recipients, who commence dual- or triple-agent prophylaxis that typically includes prednisolone, mycophenolate mofetil and calcineurin inhibitors or sirolimus. Hence, the poorer prophylaxis outcomes in corneal patients compared to renal transplant recipients may be due to (i) low drug doses, (ii) short duration rather lifelong prophylaxis and (iii) the narrow spectrum of activity within the alloreactive cell phenotypes of monotherapy [61]. Monotherapy with calcineurin inhibitors, which block T lymphocyte clonal expansion by interfering with interleukin-2 gene transcription, may also be less effective as most graft-reactive cells in the anterior chamber after rejection onset in humans are CD14+ cells of monocyte-derived macrophage lineage rather than lymphocytes [62].
Cyclosporin A
Cyclosporin A (CsA) is a calcineurin inhibitor that disrupts the signalling pathways necessary for the proliferation of activated T lymphocytes via interleukin-2 gene transcription. Various studies have evaluated the use of systemic CsA in addition to topical steroids in high-risk grafts. Direct comparison is limited by varying methodology such as their prospective versus retrospective nature, the inconsistent inclusion of HLA-matched grafts, varying intended CsA serum trough levels and the use of additional systemic corticosteroids in some studies. Survival of these high-risk grafts at 2 years has been reported to range from 67 to 74 % [63–67].
Hill and colleagues in their prospective series reported a significant reduction in rejection episodes in their CsA (49 %) group compared to controls (73 %) and noted that there was a significant higher rate of rejection reversal in patients on CsA 63]. Duration of CsA prophylaxis was also important; the group receiving CsA for 12 months had better rejection-free survival compared to those receiving CsA for 4 months or controls [68]. However, this contrasts with other studies that did not find a significant difference in graft rejection incidence or graft survival between CsA and control groups [65, 66].
Topical CsA has also been evaluated as rejection prophylaxis in high-risk grafts without convincing evidence of its efficacy. A prospective randomised trial did not demonstrate a significant difference in graft rejection incidence using CsA 2 % in addition to topical steroids, but did find a significantly higher proportion of reversibility in rejection episodes in the CsA group [69]. Other retrospective case series have reported significantly higher rejection-free graft survival rate in CsA 2 % versus control groups, but no difference in overall graft survival [70, 71]. Interestingly, one case series demonstrated blood levels of CsA after topical treatment [72].
Tacrolimus
Tacrolimus is a macrolide antibiotic isolated from the soil fungus Streptomyces tsukubaensis. Like cyclosporine, it is also a calcineurin inhibitor and has been successfully used in liver and renal transplantation [73]. Both topical [74, 75] and systemic [76–78] tacrolimus has been evaluated in high-risk grafts as monotherapy.
Joseph and colleagues reported the use of oral tacrolimus (aiming for a trough level of 1–12 μg/l) for 18–24 months in 43 patients. Five patients experienced rejection-related graft failure (12 %), whilst a further three patients experienced rejection episodes that were reversed [77]. Yamazoe and colleagues used a lower dosage of tacrolimus in their recent prospective study of 10 patients with a history of graft failure whilst on systemic CsA prophylaxis, aiming for a target trough level that was half of that used in renal transplantation (8–10 μg/l for 2 months then weaned to a maintenance level of 5–6 μg/l) for 18 months. Graft rejection occurred in 2 patients (20 %), both of which led to graft failure [78]. However, they reported significantly fewer graft rejection episodes on tacrolimus compared to cyclosporine in the same cohort of patients. Side effects were reported in 20–60 % of patients.
Mycophenolate Mofetil and Sirolimus
Mycophenolate mofetil (MMF) is a purine synthesis inhibitor that selectively inhibits proliferation of T and B lymphocyte proliferation. MMF has been shown to be effective and safe as prophylaxis against rejection following kidney, heart and liver transplantation [79–83].
Birnbaum and colleagues evaluated the efficacy of MMF for 6 months versus controls in a prospective, multicentre randomised trial involving 98 patients. Kaplan-Meier analysis demonstrated significantly higher rejection-free graft survival in the MMF group (83 %) compared to controls (65 %) with an average follow-up duration of 35 months. Rejection-related graft failure was 29 and 78 % in the MMF and control groups, respectively. Sixty-three percent of patients in the MMF group experienced side effects; 3.5 % of patients needed to be withdrawn from the MMF group due to severe side effects [84].
Studies comparing MMF with CsA have been conflicting. A prospective study of 56 patients did not demonstrate a significant difference in rejection rates [64], whilst a later retrospective study of 417 patients with 3-year follow-up reported a statistically significant, stronger effect of MMF in terms of rejection-free survival [85].
MMF has also been compared with oral sirolimus (rapamycin) administered for 6 months as monotherapy without a significant difference in the incidence of rejection [86]. Sirolimus is a microbial macrolide that prevents G1 to S phase progression in the T lymphocyte cell division cycle and is active against T lymphocytes, B lymphocytes, dendritic cells, monocytes and macrophages.
Chatel and Larkin evaluated the efficacy of combination therapy with MMF and sirolimus in a prospective case series where patients were at high rejection risk but did not have any other risk factor for graft failure. Six patients received both sirolimus and MMF for 12 months, followed by sirolimus for another 2 years at trough serum levels used in prophylaxis following cadaveric kidney transplantation (sirolimus aiming for a blood trough level of 12–20 μg/l; MMF 2 g daily). Rejection episodes occurred in 3 patients (50 %), one of which led to transplant failure. Graft survival was 83 % with a minimum follow-up of 13 months, and only one patient required cessation of MMF due to significant adverse effects [61].
Endothelial Keratoplasty Following Failed Penetrating Keratoplasty
In cases where endothelial failure ensues subsequent to graft rejection, endothelial keratoplasty has become the preferred option for many surgeons to restore graft clarity where possible, particularly in cases where the failed penetrating keratoplasty has healed with a satisfactory refractive shape profile. Its advantages over a repeat penetrating keratoplasty include preservation of tectonic integrity and faster visual rehabilitation (Fig. 8.3).
Fig. 8.3
Descemet stripping automated endothelial keratoplasty (DSAEK) following failed penetrating keratoplasty (PK) due to allograft rejection. The edge of the DSAEK graft can be seen beneath the PK (black arrow)
Mitry and colleagues in a recent review of 246 eyes that underwent Descemet stripping automated endothelial keratoplasty (DSAEK) following failed penetrating keratoplasty (PK) across six sites in Europe, United States and Asia reported an estimated DSAEK survival rate of 89, 74 and 47 at 1, 3 and 5 years, respectively [87]. Other single-centre case series have also reported similar rates of graft survival [88–90]. This is comparable to the 1- and 5-year graft survival rates for repeat penetrating keratoplasty of 80 and 58 %, respectively, for a second graft, and 71 and 47 %, respectively, for a third graft [16]. The Collaborative Corneal Transplantation Studies Research Group has also reported the increasing risk of graft failure with repeat grafts, from 17 % without a previous graft to 53 % with 2 or more previous grafts [18]. A promising finding was that a number of factors that increase the risk of graft failure following repeat PK, such as corneal vascularisation and number of previous PK, were not significant risk factors following endothelial keratoplasty [91].
Based on multivariate analysis, Mitry and colleagues reported significant pre-operative risk factors for DSAEK failure following failed PK as young recipient age, previous tube filtration surgery and rejection episodes before PK failure. It is important to note that any rejection episode prior to PK failure was found to be a significant predictor of post-DSAEK rejection, which in turn was a significant predictor of DSAEK failure [87]. This is in contrast to Anshu and colleagues, who did not find a DSAEK rejection episode to be a significant risk factor for subsequent graft failure, but concurred that previous tube filtration surgery is an independent risk factor [91]. Visual rehabilitation following DSAEK has also been reported to be comparable to that of a repeat PK [87, 91–93].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


