Pediatric Ophthalmology
Edited by P. F. Gallin
Thieme Medical Publishers, Inc.
New York ©2000

24

Plastic Surgery
This chapter details congenital ptosis and nasolacrimal duct obstructions, which together constitute the majority of nontumorous pediatric ophthalmology/plastic surgery cases. More detailed and global information can be obtained in the many superb and detailed ophthalmic plastic surgery texts referenced herein.
 Congenital Ptosis
Congenital Ptosis
In addition to a host of associated clinical issues including amblyopia, anisometropia, strabismus, and blepharophimosis, the cosmetic appearance of the child with ptosis is objectionable to parents and may affect social interaction with other children. Severe bilateral ptosis that produces the head-back and chin-up posture may interfere with the child’s ability to walk and delay general motor development. Included in this discussion of congenital ptosis are those cases secondary to developmental dystrophy without any innervational abnormality.
After a comprehensive physical examination is performed to exclude other congenital anomalies, meticulous history taking and ophthalmic examination are imperative to arrive at the proper diagnosis and the best management plan. All phases of examination and management must be carefully balanced with the needs of the child and parents, including the child’s general development.
Evaluation
One initiates the evaluation of a child with congenital ptosis with a careful history. Although generally rare, a family history of congenital ptosis may be elicited. Blepharophimosis syndrome (including telecanthus, epicanthus inversus, and often lateral ectropion of the lower eyelids) constitutes 3 to 6% of cases of bilateral congenital ptosis and is transmitted as a dominant hereditary trait. Because of the intimate embryologic association of the levator and superior rectus muscles, some cases of congenital ptosis may be seen with ipsilateral weakness of the superior rectus muscle.1,2
The parents’ observations are always important in determining the child’s level of impairment and variability. The ophthalmologist must conduct thorough discussions with parents to rule out the possibility of birth trauma, myasthenia gravis, or synkinetic causes.
Physical Examination
After a complete general physical examination is performed by a pediatrician, the ophthalmologist should first perform a general inspection including head and chin position, brow, and frontalis muscle elevation. The examiner should take care to note the chin-up head position, furrows on the forehead, and markedly arched eyebrows. These features underscore the functional impairment the ptosis has upon the child. Variation of the degree of ptosis with jaw or extraocular muscle movement suggests synkinetic ptosis. From 4 to 6% of all congenital ptosis cases are associated with the jaw-winking phenomenon of Marcus-Gunn. This syndrome is characterized by ptosis that is either reduced or overcompensated with chewing movements. Infants sucking on a bottle or pacifier will often elicit these synkinetic movements. Old photographs may also assist the ophthalmologist in assessing the history and possible variability.
Visual acuity and cycloplegic refraction must be performed to evaluate for the presence of amblyopia either secondary to lid occlusion or anisometropia from unilaterally oblique astigmatism. A careful neuroophthalmic exam will identify superior rectus or congenital oculomotor palsy or Horner’s syndrome.
A meticulous data sheet must be devised for each patient with congenital ptosis. While the patient fixates at a distant target, the following signs should be noted. Palpebral fissure height, marginal reflex distance, upper lid crease position, levator function, and tarsal width should be measured; the presence of Bell’s phenomenon, jaw winking, or Cogan’s lid twitch sign (as seen in myasthenia gravis) should be noted. In the appropriate setting, pharmacologic testing (including phenylephrine hydrochloride 2.5%, cocaine, and hydroxyamphetamine) should be performed.
The degree of levator function should be carefully measured. The frontalis muscle’s contribution to eyelid elevation is eliminated by exerting mild pressure with the examiner’s open hand upon the forehead and brow. A millimeter ruler is held in front of the patient’s eye, and the patient is then instructed to look downward. In this position, the millimeter ruler is lined up with the lid margin, and then the patient is instructed to look in extreme upgaze. The amount of excursion between these two positions is noted as the levator function.
At times a pharmacologic agent is instilled in the fornices and the levator function is remeasured. This determines if the sympathetic lid receptors correlating with Muller’s muscle are functioning.
Drawings, photographs, and basic tear production tests are also of paramount importance before arriving at a diagnosis and developing a treatment plan.
Treatment
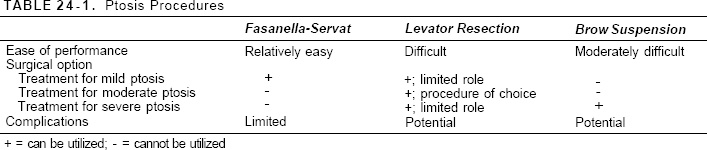
Once diagnosis of congenital ptosis is made, a management plan must be devised based primarily on the magnitude of the ptosis and visual disability and secondarily on cosmetic consequences (Table 24-1).
Indications
Mild Unilateral or Bilateral Ptosis
Mild ptosis that does not encroach upon the visual axis is a cosmetic issue and can be approached surgically after a child reaches 4 to 5 years of age, when measurement can be more readily obtained and social interaction at school becomes an issue. The parents, in conjunction with the physician, determine the optimal time.
This type of ptosis is associated with good levator function (10 to 11 mm or more) and is easily treatable with a Fasanella-Servat tarsectomy or relieved by a small (10 to 13 mm) levator resection performed either via the skin or conjunctival route.1
Moderate Ptosis
Moderate ptosis is both functionally and cosmetically important because it often causes the child to adopt a head-back, chin-up position to compensate. If the child has fair levator function (5 to 7 mm), a large levator resection of 18 to 22 mm should be considered. If the levator function is good (8 mm or more), a moderate amount of levator resection (14 to 17 mm) is performed.1
Severe Ptosis
This type of ptosis is most functionally disabling and usually requires intervention between 1 and 1½years of age. This form is usually associated with poor levator function (4 mm or less). It is probably best to first attempt a maximal levator resection (23 to 24 mm or more) by the skin approach. If this procedure fails, the most definitive procedure is a fascia lata brow suspension.1
Surgical Options
Fasanella-Servat Tarsectomy
This rather simple operation has been modified by many and is an invaluable procedure in the management of mild ptosis associated with good levator function (10 to 11 mm or more). Although some of the levator aponeurosis is included, this procedure is largely a tarsectomy with shortening of Muller’s muscle.
The details of this operation can be briefly described (Fig. 24-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


