Airway problems in children are managed with a variety of techniques, depending on their cause, severity, chronicity, and anticipated outcome. The decision of whether a child would benefit from a tracheotomy is often made by the managing airway surgeon or otolaryngologist in the acute or emergent setting. More elective decisions regarding tracheotomy in children with chronic airway obstruction, respiratory failure, prolonged intubation, or the need for pulmonary toilet are often best made by a multidisciplinary team, including otolaryngologists, pulmonologists, critical care physicians, and general pediatricians.
Although pediatric tracheotomy is a relatively infrequently performed procedure, children undergoing tracheotomy still utilize a great deal of health care resources. One study estimated that 4,861 tracheotomies were performed in children in the year 1997 (
1). The estimated aggregate inpatient hospital charges for children with tracheotomies in 1997 was about $952 million per year or about $200,000 per child, which would be about $1.34 billion per year or $282,000 per child in 2011 dollars (
1). Hospital admissions for tracheotomy rank among the longest hospitalizations for all children with all problems (
2). Pediatric patients with tracheostomy tubes have high hospital readmission rates, even 5 years after the tracheotomy was performed (
2). Furthermore, parents caring for children with tracheostomy tubes experience considerable caregiver burden. Indeed, having a child with a tracheostomy tube can affect caregivers’ emotional wellbeing, as well as have a significant economic impact on the family (
3,
4). In one study, caregivers of children with tracheostomy tubes reported adverse effects on many aspects of their quality of life, including sleep, relationships, social life, and ability to work (
4).
Although the terms “tracheotomy” and “tracheostomy” have been used interchangeably in the past, they have distinct meanings. The term “tracheotomy,” from the Greek word tome (to cut), refers to the surgical procedure and the act of making an opening in the trachea. On the other hand, “tracheostomy,” from the Greek word stomoun (to provide a mouth or opening), refers to the actual opening or hole in the trachea. A tracheostomy tube is the tube that is placed into that opening in the trachea.
HISTORY
The history of tracheotomy is fascinating and a knowledge of that history helps better understand the procedure today. References to making an opening in the windpipe are found in at least two of the three oldest known medical books, including the Rig Veda, a sacred Hindu book written between 2000 and 1000 bc (
5). In the eighth century bc, Homer described the operation of cutting open the trachea to relieve a choking person (
5). In the fourth century bc, Alexander the Great is reported to have punctured the trachea with the point of his sword to help a soldier choking on a bone lodged in his throat. Asclepiades, who practiced in Rome in the second century bc, was the first surgeon known to perform elective tracheotomies. Galen and Aretaeus both described and discussed tracheotomy in the second century ad (
5,
6). The procedure was further defined in the second century ad by Antyllus, who recommended that the
arteria aspera (trachea) be divided with a transverse incision at the third or fourth ring (
6). In the seventh century ad, Paul of Aegina repeatedly performed tracheotomy and recorded that one could know when the airway had been entered by the rush of air and the loss of the patient’s voice (
6). From that time until the 16th century, there is little in written medical history about tracheotomy.
There are frequent references to tracheotomy from the 16th century until around 1830, but most were negative, considering the procedure useless and dangerous (
5). During this time period, only 28 successful tracheotomies were described in the literature (
6). In 1590, Sanatorius used a trocar to perform a tracheotomy and left a cannula in place for the first time (
5). In 1620, Nicholas Habicot
described what was possibly the first successful pediatric tracheotomy in a 14-year-old boy, who swallowed a cloth wrapped around 9 coins. The package of coins lodged in the esophagus and compressed the trachea, causing airway obstruction. The tracheotomy relieved the airway obstruction and the coins were pushed into the stomach, later to pass in the stool (
6). Habicot also performed a tracheotomy in another young man as a means to evacuate blood from the airway, which had resulted from a penetrating wound of the larynx (
5). In 1650, Theophilus Bonetus recommended the use of tracheotomy for a 7-year-old boy who had airway obstruction from aspirating a piece of bone; unfortunately, he was overruled by the boy’s primary physician and the child died (
5).
Heister was the first to use the term “tracheotomy”. In 1839, he described the operation using a straight tube and a trocar, and suggested that it had been neglected by modern surgeons (
5,
6). In the early and mid-19th century, tracheotomy became commonly used as a life-saving treatment for diphtheria patients (
5). Trousseau (
7) reported having performed the operation on more than 200 patients with diphtheria, and saving the lives of about one quarter of them. As a result of the successful use of tracheotomy for airway obstruction in diphtheria patients, the operation became popular for other causes of airway obstruction, including croup, foreign bodies, and trauma (
5). Indeed, the medical literature in the second half of the 19th century is full of articles on tracheotomy, including technique, postoperative complications, and indications (
5).
Chevalier Jackson (
8,
9) demonstrated that when tracheotomy is performed with proper technique and postoperative care, the mortality from the procedure is quite low. He recommended using a slow and deliberate technique and avoiding a hasty operation, avoiding general anesthesia when airway obstruction is present, avoiding a “high” tracheotomy or division of the cricothyroid membrane, and dividing the thyroid isthmus (
8,
9). He also emphasized the importance of proper postoperative care, stating “the ‘pipes,’ natural and instrumental, must at all times be kept clear” (
8).
Tracheotomy was also used in the early administration of general anesthesia in the late 19th century (
5). However, by the early 1900s, when endotracheal intubation was popularized, the use of tracheotomy for this indication markedly decreased. In addition, in the early 20th century, immunization for diphtheria and the introduction of sulfonamides significantly decreased airway problems from upper respiratory infections (
5).
In the 1930s, tracheotomy again was popularized as a useful procedure for the respiratory care of patients with poliomyelitis (
5,
10). The introduction of the polio vaccine (Salk vaccine) in the 1950s markedly decreased the incidence of poliomyelitis and the need for tracheotomy for this indication. As late as the 1970s, laryngotracheobronchitis and epiglottitis were common indications for tracheotomy in children, before endotracheal intubation became a popular treatment for acute airway obstruction from inflammation (
11). However, vaccination against
Haemophilus influenzae type B has contributed to significantly decreasing the rates of epiglottitis in children.
Since the 1960s and 1970s, the indications for tracheotomy in the pediatric population have shifted from its predominant use for the treatment of acute airway obstruction from infection and inflammation to the modern indications of the need for prolonged ventilation in patients with respiratory failure (e.g., from prematurity and bronchopulmonary dysplasia), the management of chronic airway obstruction, and the need for pulmonary toilet to manage excessive secretions (
12,
13,
14).
INDICATIONS FOR TRACHEOTOMY
There are three main indications for tracheotomy in the pediatric population: (a) respiratory failure and anticipated need for prolonged ventilation; (b) upper airway obstruction; (c) providing access for pulmonary toilet. Some children who benefit from tracheotomy have more than one of these indications.
Table 92.1 lists many of the indications for tracheotomy in children, divided into these three main categories, although there is some overlap between these categories.
A survey of 85 pediatric otolaryngologists who performed a combined total of more than 2,000 tracheotomies per year demonstrated that about 40% were performed for ventilator dependency, 30% for extrathoracic airway obstruction, 20% for neurologic dysfunction, and 10% for intrathoracic airway obstruction (
15). In two separate series of patients separated by a decade, Wetmore et al. (
11,
13) found that prolonged intubation was the primary indication for tracheotomy in 53% of patients and airway obstruction in 38% or 39% or patients, with the remaining patients having other indications such as pulmonary toilet. In a recent series from Lyon, France, prolonged ventilator dependence was the indication for tracheotomy in 57% of children and upper airway obstruction in 43% (
16). Another recent study demonstrated that 46 of 70 children (66%) who underwent tracheotomy had the procedure for prolonged mechanical ventilation (
17). This study also found that children who have a tracheotomy for prolonged mechanical ventilation are likely to require a significantly longer hospital stay than children who have a tracheotomy for other reasons (
17).
Many studies have demonstrated a significant change in indications for tracheotomy in the past 30 years (
12,
13,
18,
19). There has been an increase in tracheotomies for prematurity and chronic lung disease, congenital anomalies, acquired subglottic stenosis, and neuromuscular disease, and a concomitant decrease in tracheotomies for infectious diseases such as laryngotracheobronchitis (croup) and epiglottitis, as well as for short-term airway management (
13,
18). In one study, infants and young children were most likely to undergo tracheotomy for congenital anomalies, prematurity, lung disease, or some combination of these indications, whereas in adolescents, injury was the most common reason for tracheotomy (
1).
In children, respiratory failure and prolonged ventilator dependence are often caused by prematurity and bronchopulmonary dysplasia. In a study of 450 children who underwent tracheotomy, Wetmore et al. (
13) found that bronchopulmonary dysplasia was the most common diagnosis.
Upper airway obstruction in children may be caused by craniofacial or structural abnormalities of the upper airway or by dynamic obstruction from hypotonia secondary to neurologic or neuromuscular disorders (
12). Such hypotonia also can result in excess secretions or difficulty managing secretions; in these cases, tracheotomy also provides the benefit of easier access for suctioning and pulmonary toilet.
In the pediatric population, more tracheotomies are performed during the first year of life than during any other age group (
12). In a series of preterm infants undergoing tracheotomy, Pereira et al. (
20) found that 73% were performed for ventilator dependence, 18% for airway obstruction, and 9% for pulmonary toilet (
20). Another study of tracheotomy in the preschool population found that tracheotomies are not very commonly performed in preschool-age children and the most common indication in this age group is the need for pulmonary toilet, often due to progressive neurologic disease; trauma was the second most common indication in this age group (
21).
TRACHEOTOMY VERSUS ENDOTRACHEAL INTUBATION
Since the late 1970s, endotracheal intubation has replaced tracheotomy as the primary management technique for airway obstruction secondary to infectious etiologies such as laryngotracheobronchitis and epiglottitis (
12,
18). Anesthesiologists and pediatric intensivists have become more skilled at performing difficult intubations. For example, fiberoptic intubation has permitted some patients with
craniofacial disorders to have endotracheal intubation rather than a tracheotomy.
In the neonatal and pediatric intensive care units, improved management of endotracheal tubes has both decreased the complication rate from prolonged intubation and improved long-term intubation as an alternative to tracheotomy (
18). In one recent 12-year series, the overall rate of tracheostomy tube placement for patients admitted to the neonatal intensive care unit was 0.7% (
22). Indeed, the incidence of neonatal-acquired subglottic stenosis has significantly decreased over the past several decades (
23).
Endotracheal intubation has the potential to cause injury to the glottis, subglottic region, and trachea relatively quickly, particularly if there is an improperly sized endotracheal tube, over-inflated endotracheal tube cuff, infection, or active gastroesophageal reflux. Perichondritis, infection, and active reflux can lead to delayed healing and scar formation. In adults, tracheotomy is typically recommended when there is an anticipated need for endotracheal intubation for more than 1 or 2 weeks. In infants and children, this time period can be prolonged with proper selection of endotracheal tube size, avoiding cuffed tubes or minimizing the pressure in the cuffs, and restricting movement on the tube. Newborns can tolerate longer periods of intubation (greater than 50 days) with a low risk of subglottic stenosis (
24). One study suggested that children between the ages of 1 month and 18 years can also tolerate prolonged intubation well, and that with a properly managed endotracheal tube, 30 to 60 days is a reasonable time period (
24). The average intubation period before tracheotomy in children was 32 days in one recent study and 43 days in another (
19,
25). However, there is no standard timing for tracheotomy after prolonged ventilation in children (
17,
24). The need for repeated intubation for a variety of reasons or multiple failed self-extubations also may be a reason for an earlier tracheotomy.
Table 92.2 provides a list of the relative advantages and disadvantages of tracheotomy versus prolonged endotracheal intubation. For children who have a relatively short need for intubation and who are not moving around, endotracheal intubation may be a better choice than tracheotomy. One advantage of endotracheal intubation is that it can be performed by many health care providers, whereas tracheotomy requires an experienced surgeon. Endotracheal intubation does not require a surgical procedure with the associated complications. However, disadvantages of endotracheal tubes include that they can become easily plugged, especially in younger children with smaller tubes, they can cause damage to the glottis and subglottis, and they are less comfortable for awake patients.
With tracheotomy, shorter, larger tubes can be placed, leading to decreased airway dead space and easier access for pulmonary toilet. There is less propensity to cause damage to the larynx, including the supraglottic, glottic, and subglottic regions. Tracheostomy tubes tend to be more comfortable for awake patients than endotracheal tubes. Children with a tracheostomy can be discharged from the hospital, even while still requiring a mechanical ventilator. In addition, care for children with a tracheostomy can be provided by trained caregivers/family members and does not necessarily require the constant presence of a health care professional.
There are a variety of techniques available to try to avoid tracheotomy in certain cases of upper airway obstruction (
16). For example, some patients with isolated acute subglottic injury from endotracheal intubation can respond to balloon dilation of the airway. In selected cases of patients with recurrent croup and fixed subglottic stenosis, when this is the only airway lesion and the patient has no pulmonary compromise, a single stage laryngotracheal reconstruction
can be an alternative to tracheotomy. Some patients with Pierre Robin sequence and airway obstruction from retrognathia and glossoptosis can avoid a tracheotomy by undergoing mandibular distraction osteogenesis as a newborn. The details of these techniques to avoid tracheotomy and their appropriate indications are beyond the scope of this chapter.
TRACHEOTOMY TECHNIQUE
With the exception of a few life-threatening emergencies, tracheotomy in children should be performed in the controlled setting of the operating room under general anesthesia. When possible, the procedure should be performed with the patient intubated with an endotracheal tube to control the airway. If there is significant upper airway obstruction and endotracheal intubation is not possible but a rigid ventilating bronchoscope can be inserted, the procedure can also be performed over the bronchoscope. A laryngeal mask airway (LMA) can also be used when it is not possible to perform endotracheal intubation and a rigid bronchoscope cannot be passed or is not available. In children, awake tracheotomies without a controlled airway should be reserved for the few life-threatening situations in which endotracheal intubation or insertion of a rigid bronchoscope or LMA is not possible. Percutaneous tracheotomy is generally not recommended in children.
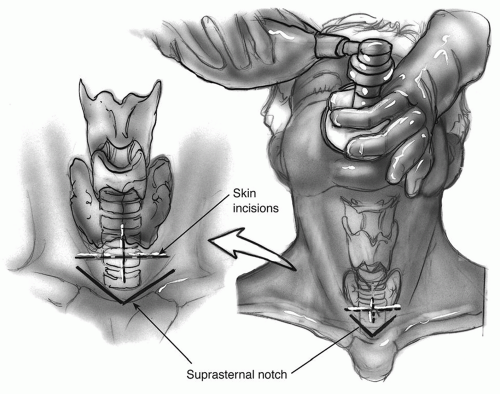
The patient is placed supine on the operating table with a shoulder roll to extend the neck (
Fig. 92.1). In children with short necks or significant submental fat, tape can be used to help keep the submental pannus out of the way and to hold the head in position. The neck is carefully palpated and the level of the cricoid cartilage, thyroid notch, and sternal notch are marked (
Fig. 92.2). The infant larynx is located higher in the neck than in older children and adults, the thyroid cartilage is broader, and the cricoid cartilage is often the most prominent palpable structure. The skin incision is marked between the level of the sternal notch and cricoid cartilage (
Fig. 92.3). The skin can be infiltrated with local anesthesia with epinephrine. The neck is then prepared and draped, although the face is often left uncovered in order to provide access to the endotracheal tube by the anesthesiologist.
Either a horizontal or vertical skin incision can be made. Excessive subcutaneous fat deep in the incision can be removed using electrocautery (
Fig. 92.4). The platysma fascia is divided. The strap muscles are then divided vertically and retracted (
Figs. 92.5 and
92.6). The thyroid isthmus can be retracted superiorly or inferiorly, or divided (
Fig. 92.7). If the thyroid isthmus is sitting over the area where the incision in the trachea should be made, the isthmus should be divided with electrocautery and ligated. The trachea is palpated often during the procedure to ensure
that the approach to the trachea remains in the midline (
Fig. 92.8). The trachea in children is more pliable and has more lateral mobility than in adults; so it is important to be sure that dissection remains in the midline with the trachea centered in the surgical field. Excessive lateral dissection should be avoided to help minimize subcutaneous air and decrease chance of injury to the dome of the pleura or recurrent laryngeal nerves. When using electrocautery during tracheotomy, the fraction of inspired oxygen (FiO2) should be kept below 30% to help prevent a surgical fire.