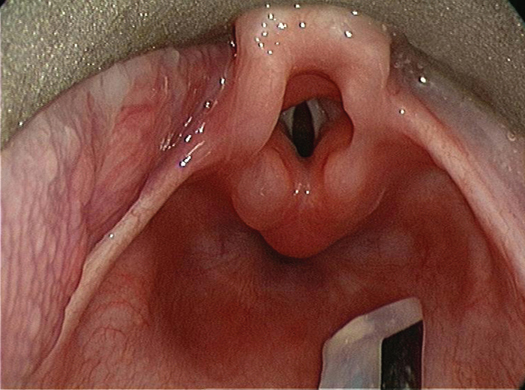
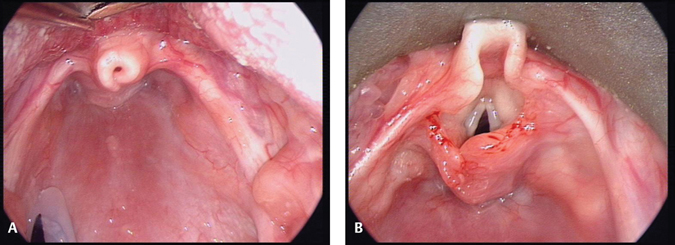
31 Pediatric Laryngology: Diagnosis and Treatment of Congenital Anomalies The pediatric larynx is different from the adult larynx in size, shape, and position. The main functions of the larynx are providing breathing passage, prevention of aspiration, and voice production. As a result, the laryngeal anomalies present with symptoms related to these functions. Laryngomalacia or “floppy larynx” is the most common congenital anomaly of the pediatric larynx. It is the most common cause of stridor in young children. Nearly 50 to 75% of stridor in children in the general population can be attributed to laryngomalacia.1 It is characterized by collapse of the supraglottic structures on inspiration. The spectrum of presentation of disease, progression, and outcomes varies. Some children have a mild stridor with no consequences, while others can have feeding difficulties or severe airway compromise.2 There are three theories of etiology. 1.Immature cartilage has been proposed but histopathology has demonstrated normal cartilage, and the absence of laryngomalacia in premature infants makes this unlikely. 2.A neuromuscular imbalance has been suggested. This may explain laryngomalacia in children with neurological disease but is unlikely to be the explanation in normal children. 3.A variant in normal anatomy that leads to progressive collapse over the early weeks of life before growth and increased rigidity lead to a reduction in symptoms. This seems most likely. Most of the published literature suggests that the affected infants are likely to be male and term pregnancies in Caucasians. African-American infants of all gestational ages may be at risk and low birth weight may be a stronger predictor of laryngomalacia regardless of patients’ gender and ethnicity.3 Gastroesophageal reflux disease contributes to feeding difficulties. Medical comorbidities, especially neurological abnormalities, heart disease, and associated anomalies contribute to disease severity and affect surgical outcomes. Various classification systems have been proposed but offer little contribution to the clinical management. They are essentially descriptive. Three abnormalities are present to a greater or lesser degree: tightly curled epiglottis, short aryepiglottic folds, and prolapsing arytenoids (Fig. 31.1). The history is highly suggestive of the diagnosis of laryngomalacia in most of the cases. These children usually present with an inspiratory stridor within the first 2 weeks of life. The stridor varies with position of the child and level of activity. The stridor is worse with crying and feeding and in supine position. On examination, subcostal retraction indicates severe obstruction and pectus excavatum indicates chronic obstruction. Severe cases may be associated with feeding difficulty, failure to thrive, intermittent complete obstruction, or cardiac failure.4 The stridor usually increases in severity over the initial few months, being at its worst at 6 months of age. This improves and resolves gradually. The possibility of synchronous lesions should not be overlooked as 27% of the children presenting to a tertiary referral center with laryngomalacia can have synchronous airway anomalies.5 Most of the children with laryngomalacia have mild symptoms and do not require surgical intervention. The symptoms usually begin at 2 weeks of age and are at its worst by 6 months of age and then plateau and gradually start resolving. The majority of these will resolve spontaneously by 18 to 24 months. Children with reflux disease have improvement in their symptoms with antireflux medications. Nearly 20% of children with laryngomalacia have airway or feeding symptoms severe enough to need surgical management. Children with severe disease and no other comorbidities should be offered aryepiglottoplasty and have good outcomes. Others with multiple medical comorbidities could be offered aryepiglottoplasty, but do not have good outcomes. Supraglottoplasty (Fig. 31.2A, B) encompasses any surgical procedure to modify flaccid obstructing supraglottic structures. The position and extent of the surgical excision is adapted to fit the individual patient’s anomaly. Complications of the procedure include supraglottic stenosis, aspiration, dysphagia, and lower respiratory infections. Very rarely tracheostomy is required for severe cases of collapse of the supraglottis. Clinical Pearls •Laryngomalacia is the most common cause of stridor, but every stridor in a child is not laryngomalacia. •Airway endoscopy should be performed early if there are any odd features in the history. •Aryepiglottoplasty is a good surgical treatment, but the excision needs to be conservative to minimize complications. The saccule is a pouch arising from the anterior end of the laryngeal ventricle. Saccular cyst or a laryngocele is an abnormal dilatation of the saccule. It is usually filled up with air and mucus. A saccular cyst can be congenital or acquired. Its lumen is isolated from the interior of the larynx and it does not contain air. These features differentiate it from a laryngocele. A saccular cyst is also submucosal and is covered with normal mucous membrane. These cysts usually are secondary to developmental failure of patency of opening of the saccule or occlusion of the opening secondary to inflammation, trauma, or any other lesions. Two types of saccular cysts are lateral and anterior. The lateral saccular cyst extends posterosuperiorly into the false cord and aryepiglottic fold. The anterior cyst extends medially and posteriorly and protrudes into the laryngeal lumen. A laryngocele can be internal or external. Internal laryngocele is confined to the interior of the larynx and extends into the false cord and aryepiglottic fold. An external laryngocele extends laterally into the neck through the thyrohyoid membrane. Laryngoceles can also be congenital or acquired. The presenting symptoms in these conditions are usually intermittent hoarseness and worsening dyspnea with crying. Other symptoms include weak cry or aphonia or inspiratory stridor. Diagnosis is confirmed by airway endoscopy or magnetic resonance imaging (MRI) scan if indicated. Treatment includes aspiration or excision or deroofing of the cyst. External approach for excision is considered if endoscopic approach is unsuccessful. Vocal cord paralysis in infants is the third most common cause of congenital stridor after laryngomalacia and congenital subglottic stenosis. It can be unilateral or bilateral. Bilateral cord palsy can be secondary to other congenital anomalies, that is, myelomeningocele, Arnold-Chari malformation, and hydrocephalus. This is the result of raised intracranial pressure. Acquired vocal fold paralysis of one or both cords can follow a surgical procedure for tracheoesophageal fistula, neck surgery, or cardiothoracic surgery. The paralysis can also follow an external injury (strangulation and road traffic accident) or internal injury (endotracheal intubation or esophageal stethoscope. Children with bilateral vocal cord palsy present with inspiratory stridor, which is usually high pitched. This is because of the paradoxical movement of vocal cords being further adducted during inspiration as a result of negative intrathoracic pressure, rather than expected abduction. During expiration, the paralyzed vocal cords abduct passively. Unilateral vocal cord palsy has more subtle symptoms such as coughing, choking, aspiration, breathy voice, and weak cry. These children only rarely will have stridor. Diagnosis of vocal cord palsy can be made by awake flexible laryngoscopy or laryngoscopy under general anesthesia. It is essential to differentiate paralysis from immobility due to anterior webbing, posterior glottic scarring, or cricoarytenoid joint fixation or an infiltrative lesion. Some centers perform ultrasound to diagnose/confirm cord palsy. Flow volume loops give an objective assessment of the degree of airway obstruction in bilateral cord palsy. Up to 45% of the patients may have other coexisting airway pathologies, so a formal airway endoscopy is essential. Vocal cord paralysis in children usually resolves spontaneously within 6 to 24 months. If the recovery does not happen within 2 to 3 years, the chances of improvement are remote. The majority of children with unilateral and at least 50% with bilateral cord palsy can be managed conservatively. Surgical options for younger children include tracheostomy to bypass the obstruction caused by the paralyzed cords. Any operations on the vocal folds for bilateral paralysis are deferred until the child is at least 3 to 4 years of age to allow time for natural recovery. Any procedure to improve the airway is likely to have an adverse effect on the quality and volume of the voice. Surgical procedures are chosen on individual patient basis. Tracheostomy on its own gives the child a safe airway and does not affect the vocal cords and the potential of a good voice; however, it has the morbidities associated with it. Other surgical techniques focus on enlarging the glottic airway. The techniques include arytenoidectomy,6 lateralization suture, cordectomy, and laser cordotomy.7 In severe cases, laryngotracheal reconstruction with a posterior graft is an option. For unilateral paralysis, to reduce the aspiration and strengthen the voice, the options are of vocal cord injection or rarely thyroplasty. Clinical Pearls •Children with vocal cord palsy should have a full airway assessment to rule out any additional pathology. •Surgical treatments to improve the airway do carry a small risk of worsening the voice.
Laryngomalacia
Saccular Cyst/Laryngocele
Vocal Cord Paralysis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree