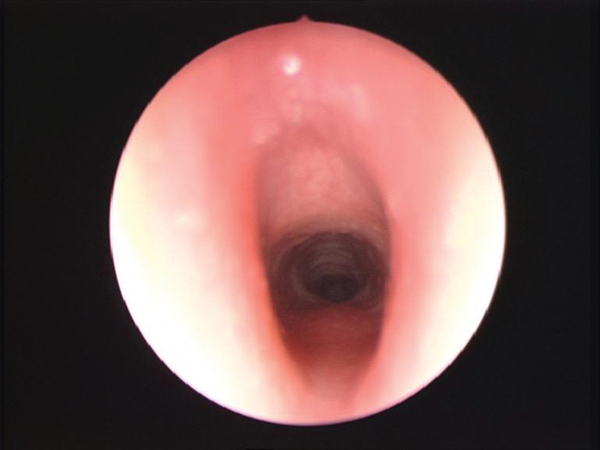
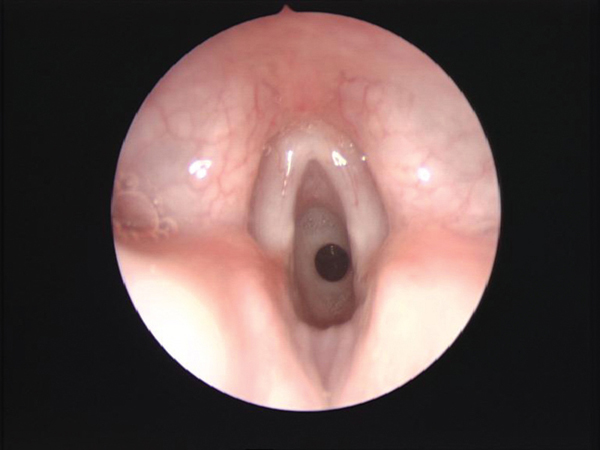
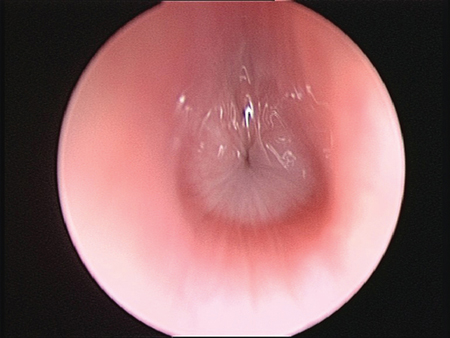
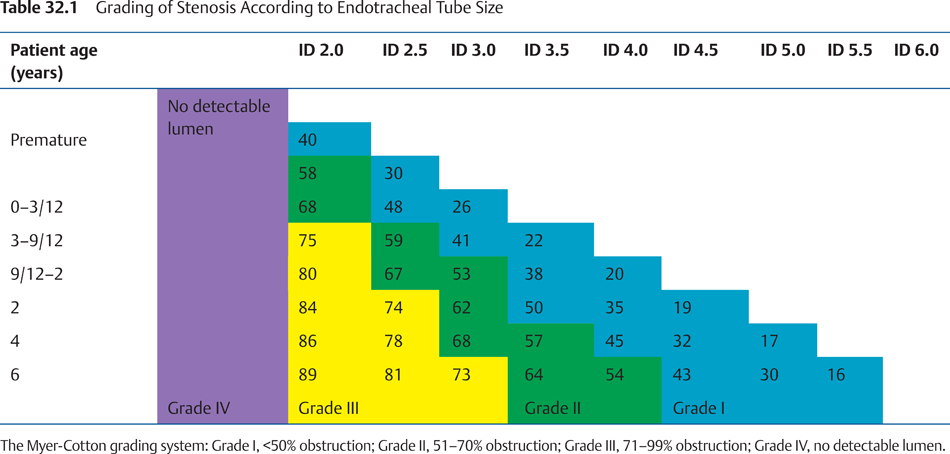
32 Pediatric Laryngology: Diagnosis and Treatment of Acquired Disorders of the Larynx Subglottic stenosis is one of the common causes of airway obstruction in children. Subglottis extends from the inferior surface of the true vocal cords up to inferior margin of the cricoid cartilage.1 The diameter of the normal subglottic lumen is 4.5 to 5.5 mm in a full-term infant and 3.5 mm in a premature infant. The diameter of subglottis less than 4 mm in a full-term infant is considered narrow. Subglottic stenosis can be classified on the basis of etiology into congenital or acquired. Other classifications are based on the characteristics, for example, soft or hard stenosis and degree of stenosis. Congenital subglottic stenosis is by definition when there is no apparent cause for the stenosis, for example, trauma or prolonged intubation. This has been discussed in detail in the congenital anomalies of larynx (Chapter 31). Acquired subglottic stenosis patients have a history of prolonged intubation or laryngeal trauma. Vast majority (90%) of acquired stenosis are secondary to prolonged endotracheal intubation.2 The incidence of subglottic stenosis after intubation in children ranges from 0.9 to 8.3%. The incidence of acquired subglottic stenosis following neonatal intubation is reported as less than 1%3 and is usually a result of prolonged endotracheal intubation. Prolonged endotracheal intubation is well tolerated in neonatal age group as the cricoid cartilage is relatively immature.4 As the child grows, the cricoid cartilage becomes more fibrous and rigid, and as a result, the larynx becomes less tolerant of the intubation in older children. Ischemic injury occurs if the pressure exerted by the endotracheal tube is greater than the capillary pressure. Ischemia leads to edema, pressure necrosis, and finally ulceration of the mucosa. These ulcerations eventually heal up by forming granulation tissues and eventually scarring causing subglottic stenosis. The factors that predispose to the development of subglottic stenosis include gastroesophageal reflux; shape and size of larynx (congenital subglottic stenosis); duration of intubation; size of endotracheal tube; repeated intubations; traumatic intubation; sepsis; systemic factors (malnutrition, hypoxemia); chronic inflammatory disorders; external laryngeal injury; chemical and thermal injury; and benign or malignant neoplasms (papillomas, hemangiomas). The use of a large-diameter endotracheal tube even for a short period can lead to ischemic ulceration and scarring. Poor fixation of the tube allowing movement also causes injury. Measures taken to prevent subglottic stenosis include use of an uncuffed tube placed via a nasal route that reduces potential tube movement to a minimum. Injury to the airway is less likely with a small tube that allows a small leak on positive pressure ventilation. Good nursing care and hygiene are paramount.5 Symptoms of acquired subglottic stenosis include biphasic stridor, with a normal cry/voice. In an intubated child, the presentation is usually failure to extubate or accepting smaller than age-appropriate tube. Signs include increased work of breathing and use of accessory muscles of respiration. Subglottic stenosis is evaluated by a direct laryngotracheobronchoscopy examination under a general anesthetic (Figs. 32.1 to 32.3). A complete assessment of the airway is required to confirm the suspected diagnosis and to rule out any coexisting tracheobronchial pathology. The exact diameter of the stenosis is measured by passing various sizes of endotracheal tubes and graded using the Myer-Cotton grading system for the stenosis.6 In addition, an assessment is made of the length of the stenosis and if it is a soft or firm stenosis. The assessment of the degree of stenosis is performed objectively by checking the size of endotracheal tube the stenosis accepts with a leak on positive pressure. This is measured against the age-appropriate endotracheal tube for that child, and the stenosis is graded accordingly6 as shown in Table 32.1. The management of subglottic stenosis depends on the severity, location, and type (soft/firm) of stenosis. Surgery is the primary treatment modality via either an open or an endoscopic approach. Grade I stenosis can be managed simply under the watchful eye of a qualified surgeon. Grade II stenosis can be treated by endoscopic procedures, that is, incision ± balloon dilatation. Endoscopic procedures may need to be repeated on a regular basis. If endoscopic management is not successful, then open procedure may be required. Grade III and IV stenosis will require open procedures. The two most common open procedures are laryngotracheal reconstruction (LTR) and partial cricotracheal resection (CTR). LTR involves splitting the cricoid cartilage and expanding the framework with a cartilage graft. Partial CTR involves segmental excision of the stenotic segment, preserving the posterior cricoid plate, and an end-to-end anastomosis.7 The management of pediatric airway reconstruction has changed considerably since its introduction in the 1970s. Surgical correction of subglottic stenosis was first attempted by Negus,8 using laryngofissure and dermal grafting in adults. Rethi9 reported splitting the cricoid ring anteriorly and posteriorly in adults. Aboulker7 (1966) introduced a stent that could be wired into the tracheostomy tube. Grahne10 first described the application of the Rethi procedure to children. Doig et al11 reported using a cartilage graft positioned in an anterior cricoid split to expand the cricoid ring, and then Evans and Todd12 described laryngotracheoplasty, which involved splitting the trachea and cricoid using a castellated incision and re-suturing it in an open manner over a stent. Cotton, unaware of Doig’s publication in the German literature, separately introduced the LTR with cartilage grafting (1978) after earlier animal work with Fearon13 and developed it into the preferred technique for framework expansion. In the 1970s and 80s, laryngotracheoplasty and LTR were the main surgical procedures, and Cotton & Evans2 reported a 5-year follow-up of LTR in children. The next development was single-stage LTR, using an endotracheal tube as an airway and stent.14,15 Monnier et al16 published the first series of successful CTRs in children. LTR with autologous cartilage grafts has been demonstrated to be an effective and reliable technique for the surgical management of subglottic stenosis. Good results have been reported from many different institutions around the world.17–20 Generally, the two-stage LTR is advocated in children with complex multilevel stenosis, significant neurological deficits, significant lung disease, or cases where reintubation is anatomically difficult (e.g., craniofacial anomalies).21 Some authors perform two-stage LTR in cases with severe stenosis,19,22 although many others advocate partial CTR in selected cases with grade III/IV subglottic stenosis where the disease is separated from the glottis by an adequate margin.7,23 Pediatric airway stenosis presents with varying degrees of severity and significant comorbidities. The choice of operation for reconstructing the airway must be considered carefully by the surgeon depending upon which modality is considered likely to achieve safe and expeditious surgical reconstruction in each individual patient. The final results of LTR are generally expressed in terms of decannulation rates. Most of the patients who have a tracheostomy undergo surgery primarily to get rid of the tracheostomy, and thus decannulation does become an important outcome measure. For those patients who did not have a tracheostomy before the LTR, the outcomes were based on the improvement in their symptoms and the airway endoscopy findings before and after the procedure. Clinical Pearls •The incidence of acquired subglottic stenosis is increasing as more preterm children are surviving with history of prolonged intubation at some stage. •The treatment needs to be tailored to the individual patients’ symptoms and severity of the stenosis.
Subglottic Stenosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree