Fig. 5.1
Lymphocytic thyroiditis, histology H&E. In an alternance of macro- and microfollicles bordered by cubic thyrocytes not showing oncocytic changes, one can see large lymphoid follicles with prominent germinal centers, as well as a diffuse interstitial lymphocytic infiltrate
Fig. 5.2
Riedel’s thyroiditis, histology H&E. Thyroid parenchyma has almost completely been replaced by dense collagen bands and a mixed, predominantly mononucleated inflammatory infiltrate. An intact and two atrophic thyroid follicles can be seen on the left of the image
5.1.4 Goiter
The term goiter is referring to an abnormal diffuse enlargement of the thyroid gland. Nodular hyperplasia of the thyroid, either uninodular or multinodular, can be the origin of a goiter. It can be endemic (related to iodine deficiency, the most common form) or less commonly sporadic and in this case of unknown etiology. In its early form, hyperplasia is diffuse and limited to the follicles that tend to adopt a macrofollicular architecture. In more advanced forms, the normal thyroid parenchyma is replaced by variously sized nodules that can present a variety of different morphological aspects. It is thus not unusual to observe nodules completely or partially encapsulated as well as areas with solid, colloid, hemorrhagic or cystic, calcified, fibrotic, and degenerated aspects. Microscopically, the thyroid epithelium can present a wide range of variations, from atrophic with flat cells to hyperplastic with cuboidal thyrocytes. Nuclei are usually centrally located, round, with inconspicuous nucleoli, and with coarse granular chromatin [1].
5.1.5 Well-Differentiated Thyroid Carcinomas
Well-differentiated thyroid carcinomas are represented by papillary thyroid carcinoma (PTC), the most common entity, and follicular thyroid carcinoma (FTC). Both forms present excellent prognosis. No precursor lesion is officially identified for both types of carcinoma. However, lesions that have not fully developed the major criteria for malignancy, i.e., typical nuclear characteristics for PTC and unequivocal capsular and/or capsular vascular invasion for FTC are usually identified as lesions of uncertain malignant potential. The most important histological feature of PTC is represented by nuclear atypia (Fig. 5.3): nuclei are raisinoid with clear chromatin, nuclear indentations (grooves), and most characteristically intranuclear cytoplasmic invaginations (nuclear pseudo-inclusions or orphan Annie eyes). Papillary structures (hence the name) are present in the classic variant, but not seen in the follicular variant, where nuclear features are also less pronounced than in the classic variant. The most important histological feature of FTC is represented by infiltration of the tumor capsule (capsular invasion) and/or infiltration of capsular vessels (vascular invasion) (Fig. 5.4). Cytologically, the morphology of the nuclei of follicular cells constituting the tumor is not different from that of normal thyrocytes. These cells are mostly arranged in microfollicular structures.
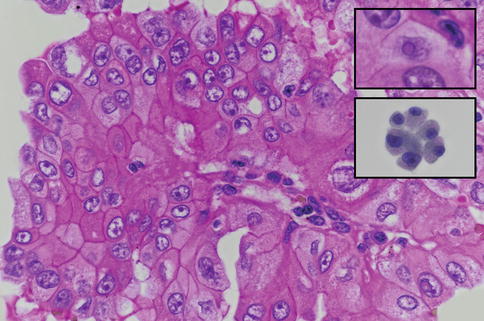
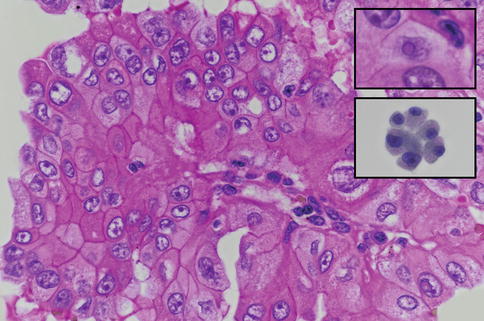
Fig. 5.3
Papillary thyroid carcinoma (PTC), histology H&E and cytology PAP (lower inset). In this oncocytic variant of PTC, cells are larger than in the classic variant of PTC, because of an increased content of eosinophilic and granular cytoplasm. Nuclei show the typical atypia of PTC: an irregular nuclear membrane outline, a ground-glass nucleus sometimes containing a pseudo-inclusion (upper inset). These cells rest on a true papilla with a vascular core. The lower inset shows the typical cytological aspect of thyrocytes with oncocytic cytoplasm and a nucleus of varying size and irregular nuclear membrane suggestive but not specific of PTC
Fig. 5.4
Follicular thyroid carcinoma, histology H&E and cytology PAP (lower inset). At low power, one can see a proliferation of small to medium thyroid follicles, bordered on the left by a thick fibrous capsule. An unequivocal capsular vascular invasion is seen in this area and at higher magnification in the upper inset. The lower inset shows a microfollicle containing a droplet of colloid, as seen cytologically. This cytological image alone could not allow a distinction between a follicular adenoma and a follicular carcinoma, capsular and/or vascular capsular invasion being necessary for the diagnosis
More and more interest is rising in the field of thyroid carcinogenesis, with several molecular markers identified as initiators: RET/PTC and PAX8/PPAR-gamma rearrangements as well as RAS point mutation. Unknown additional events are required for progression to poorly differentiated or anaplastic forms. The only molecular alteration that has been found so far to be specific for carcinoma (PTC) is the BRAF point mutation. The identification of this anomaly is particularly useful in thyroid fine-needle aspiration (FNA) cytology in case of suspicious features, as its positive predictive value for carcinoma is 100 % [2].
5.1.6 Poorly Differentiated and Undifferentiated Thyroid Carcinomas
The prognosis in these forms of carcinomas drops dramatically in comparison to the well-differentiated forms, both forms being almost always lethal. Fortunately their incidence is low, as compared to well-differentiated carcinomas. Poorly differentiated carcinomas are also named “insular carcinomas,” while “anaplastic carcinomas” describe undifferentiated carcinomas. It is not clear if these forms arise “de novo” or if they originate from well-differentiated carcinomas, both theories being probably valid. Additional genetic and epigenetic alterations are required for the progression to less differentiated forms. Histologically, insular carcinomas are characterized by a solid, trabecular, or insular (hence the name) architecture. Essential to pose the correct diagnosis are the presence of necrosis and a high mitotic activity. Anaplastic carcinomas (Fig. 5.5) show no reliable histological features to recognize them as primary cancers of the thyroid gland and thus open a differential diagnosis with locoregional or metastatic cancer: tumor is largely necrotic and cells are highly atypical with monstrous features, sometimes evoking high-grade sarcomas. Expression of basic epithelial cell differentiation markers such as cytokeratins as well as thyroid-specific markers is often lost in anaplastic carcinomas [3, 4].
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


