Parinaud’s Oculoglandular Syndrome
Elmer Y. Tu
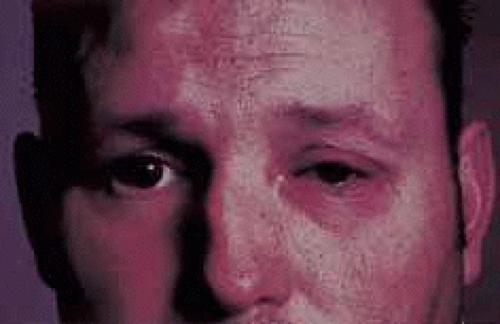
Parinaud’s oculoglandular conjunctivitis is a form of follicular, granulomatous conjunctivitis (with or without ulceration), often associated with a visible swollen preauricular and/or submandibular lymph node on the same side1 (Fig. 1). The conjunctival granuloma may occur in bulbar or palpebral conjunctiva, upper or lower. Fever and other systemic signs may or may not be present. The conjunctival granulomas and the regional lymph node swelling usually diminish in 4 to 5 weeks, although in some cases the enlarged lymph nodes may progress to suppuration.
Parinaud’s oculoglandular syndrome (POS) consists of the characteristic granulomatous conjunctival inflammation, usually unilateral, with extension to or involvement of local, ipsilateral lymph nodes. Although cat-scratch disease (CSD) is by far the most common etiology, as a syndrome it does not constitute a disease with a specific origin or pathology but is a common endpoint for multiple infectious and noninfectious processes. The clinical findings in CSD are most representative of the originally described Parinaud’s conjunctivitis. Other known causative agents are listed in Table 1. Although cat-scratch disease is usually a benign, self-limiting disease, laboratory examinations should be obtained to determine the exact causal agent and to rule out other more serious infections. Diagnostic considerations for Parinaud’s oculoglandular conjunctivitis are listed in Table 2.
Table 1. Causes and Treatment of Parinaud’s Oculoglandular Conjunctivitis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 2. Laboratory Diagnosis of Parinaud’s Oculoglandular Conjunctivitis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
CAT-SCRATCH DISEASE
Cat-scratch disease is caused by Bartonella henselae (formerly Rochalimaea) and rarely by Afipia felis.2,3 Eye involvement (benign inoculation lymphoreticulosis)4,5 develops in those persons who have close contact with cats, especially children younger than 10 years of age. Over 90% of patients report a history of being scratched by a healthy cat (see Fig. 2), often a kitten.6 Kittens are the most susceptible to infection with B. henselae and may manifest an asymptomatic bacteremia for several weeks, whereas some adult cats have been shown to be chronic carriers. Transmission from cat to cat is mediated by the cat flea, whereas cat-to-human transmission may occur from trauma (scratch), inhaling materials infected by cats, being licked by infected animals, or rubbing one’s eye after contact. Human-to-human transmission has not been reported, and patient isolation is, therefore, not required. It is also not considered necessary to remove the cat from the home because of the low overall rate of human transmission.7 However, multiple infections within the same family have been reported.8 A primary inoculation lesion in the conjunctiva, skin, or mucous membrane occurs in about 76% of patients.5
 Fig. 2 Cat scratch marks with nonsuppurative preauricular lymphadenopathy. (Courtesy of Dr. Andrew M. Margileth. Margileth, A: A new look at old cat scratch. Contemp Pediatr 7:27, 1990) |
The annual incidence of CSD is approximately 24,000, with children or adolescents making up 80% of cases.6,9 Parinaud’s is classified as an atypical manifestation of CSD and occurs in approximately 3% to 7% of all infections.4,10 Seven to 14 days after exposure, redness, irritation, watery conjunctival discharge, and the sensation of a foreign body develop in the eye. The typical lesion consists of a unilateral granulomatous nodule located in the upper or the lower palpebral conjunctiva, surrounded by follicles (Fig. 3), intense chemosis, and injection. The fornices and bulbar conjunctiva may be involved (Fig. 4). The granuloma may be single, large, and flat, or there may be multiple elevated vegetations (Fig. 5). Corneal involvement usually consists of superficial punctate keratitis, but rarely may cause significant keratitis.11
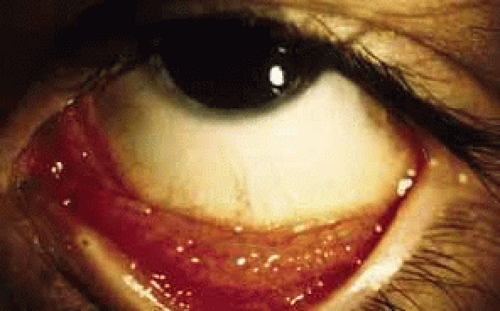 Fig. 3 Bartonella henselae (cat-scratch disease) conjunctivitis. Multiple tarsal (conjunctive) follicles are present. (Courtesy of Daniel A. Johnson, MD; San Antonio, TX) |
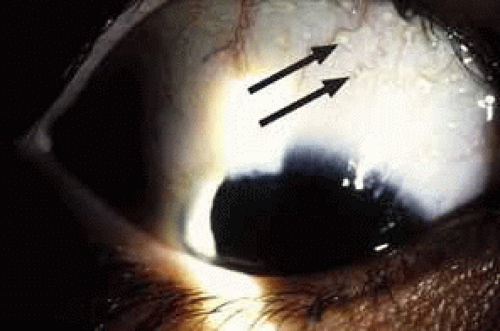 Fig. 4 Bartonella henselae conjunctivitis demonstrating multiple bulbar (arrows) conjunctival follicles. (Courtesy of Daniel A. Johnson, MD; San Antonio, TX) |
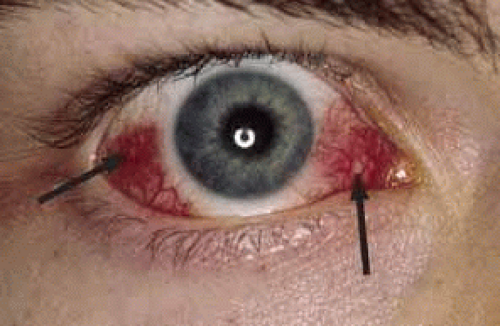 Fig. 5 B. henselae conjunctivitis multiple nonulcerative granulomas (arrows) are seen in the bulbar conjunctiva. (Courtesy of Daniel A. Johnson, MD; San Antonio, TX) |
Finding the inoculation site is often helpful in the diagnosis of cat-scratch disease. If the skin is involved first, a primary, nonpruritic papule or pustule appears 3 to 7 days after the animal scratch or bite. The skin papules persist for 7 to 21 days and disappear without a scar. A variety of other skin lesions including erythema nodosum, erythema multiforme, and nonspecific morbilliform rashes may occur.
Regional granulomatous lymphadenopathy is present in all patients with cat-scratch disease and may involve the head, neck, and axilla (Fig. 6). One to 3 weeks after inoculation, preauricular, cervical, and submaxillary nodes are visible on the affected side. The nodes are firm, are usually nontender, and may be enlarged to the size of a golf ball. Approximately 10% of these lymph nodes progress to suppuration. Systemic symptoms and signs are common but are usually mild. Low-grade fever, chills, headaches, anorexia, and general malaise may also be present. Without treatment, the course is benign, and complete recovery within 2 to 3 months is the rule.
 Fig. 6 Cat-scratch disease with golf-ball-sized axillary lymph node. (Courtesy of J. Brian Reed, MD; Wilford Hall, TX) |
Immunocompromised hosts are more likely to develop the disseminated form of the disease as bacillary angiomatosis, a reactive vascular skin tumor mimicking Kaposi’s sarcoma, or bacterial peliosis, an infiltration of systemic organs.12,13 B. henselae is an emerging human pathogen and was noted in 10% of a group of HIV patients in South Africa screened by PCR.14,15 Although immunocompetent individuals are not advised to avoid infected cats, studies in immunocompromised patients have produced conflicting recommendations.16
PATHOLOGY
Cat-scratch disease has been recognized as a clinical entity for more than 50 years. B. henselae is a small, pleomorphic, gram-negative bacillus that has been identified in conjunctival granuloma, skin, and lymph node specimens. The organism is best demonstrated using the Warthin-Starry silver impregnation stain. With a modified Brown-Hopp tissue Gram stain, the organism can be detected as a pleomorphic, gram-negative, nonacid-fast bacterium measuring 0.3 to 1 μm by 0.6 to 3 μm. The bacteria are found in the vessel walls of capillaries and in macrophages in the germinal centers, appearing as a single organism or in chains. Focal areas of necrosis are noted with activated histiocytes and polymorphonuclear in the surrounding cells, forming a granuloma.
B. henselae is very difficult to isolate using standard laboratory techniques. First described in 1990 by Relman et al., polymerase chain reaction (PCR) amplifying the 16S rRNA of B. henselae is both a highly sensitive and specific method for identifying the organism.17 Its successful use has been described on conjunctival specimens as well as lymph node biopsies and aspirates.18,19,20,21 There is no cross reactivity with other Bartonella species.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree