Essentials of Diagnosis
General Considerations
Otosclerosis is a disease process unique to the temporal bone and unlike other generalized bone dyscrasias such as Paget disease and osteogenesis imperfecta; it nearly exclusively involves the otic capsule. Disease progression is characterized by abnormal removal of mature dense otic capsule bone by osteoclasts, and replacement with the woven bone of greater thickness, cellularity, and vascularity. While otosclerosis may potentially involve any part of the bony labyrinth, it carries a distinct predilection for the region near the anterior border of the oval window (fissula ante fenestram). When disease involves the annular ligament of the oval window and stapes footplate, a conductive hearing loss (CHL) invariably occurs. Involvement of other parts of the otic capsule may result in sensorineural hearing loss (SNHL) and vestibular symptoms.
The true prevalence of histological otosclerosis is unknown. Estimates reported for clinical disease (ie, clinical otosclerosis) range from 0.5% to 1.0%. However, the incidence of subclinical disease (ie, histologic otosclerosis) in unselected autopsy series has been reported as high as 13%. About 15 million people in the United States have been diagnosed with otosclerosis, and it is considered among the most common causes of acquired hearing loss. Compared to caucasians, otosclerosis is half as prevalent among Asians (0.5%) and one-tenth as common in African-American patients (0.1%). In practice, otosclerosis is seen more often in women than in men by the ratio of approximately 2:1. However, it has been proposed that the incidence may be the same in both sexes and that hormonal influences during pregnancy might cause a more rapid progression in women, bringing them to clinical attention. Symptoms rarely become apparent before late teens, with most patients presenting between the age of 20 and 45.
Pathogenesis
The otic capsule and stapes form from a cartilaginous anlage, which begins endochondral ossification by the 19th week of embryogenesis and is complete by the end of the first year of life. The vestibular surface of the footplate remains cartilaginous throughout life. Bone turnover, which is normally seen in other parts of the body, does not occur in the “healthy” otic capsule after initial development. However, with otosclerosis there is increased osteoblastic and osteoclastic activity and vascular proliferation. The otosclerotic focus is defined by an area of increased bony turnover and metabolic activity and the term “otospongiosis” is most descriptive of the histologic appearance at this stage of the disease. As the disease stabilizes or “burns out,” the normal bone of the otic capsule is replaced with a focus of metabolically quiescent, dense mineralized bone. The most common location of the otosclerotic focus is the region of the otic capsule anterior to the stapes footplate (the region of the fissula ante fenestram). Fixation of the stapes begins as the lesion spreads to involve the annular ligament. Extension over the footplate is uncommon but may lead to total obliteration of the footplate. Less frequently, lesions may extend into the inner ear resulting in hyalinization of the spiral ligament and SNHL. Rare cases of pure SNHL from isolated cochlear otosclerosis without ossicular involvement have been reported.
The inciting stimulus for the abnormal bone remodeling in otosclerosis is unknown and has been attributed to both genetic and environmental factors. In most cases, the disease is inherited as a simple autosomal dominant trait with incomplete penetrance and variable expressivity. Recent findings suggest an association between the measles virus and otosclerosis; whether the measles virus is a factor that can initiate the otospongiotic process remains to be determined.
Clinical Findings
The typical patient with otosclerosis presents with a history of slowly progressive hearing loss that is usually bilateral and asymmetric, although unilateral disease may occur in up to 30% of patients. Patients with CHL including those with otosclerosis may also report improved hearing with background noise, a paradoxical phenomenon known as paracusis of Willis. Hearing deficits typically become apparent when they reach a 25–30 dB loss whereat the patient has difficulty understanding speech. Tinnitus is a common complaint and may be an indication of sensorineural degeneration. Fluctuations in hearing are uncharacteristic but may occur during times of hormonal instability (eg, during pregnancy) and patients rarely have complaints of vertigo.
Otoscopic examination is essential and best performed with an operating microscope. The goal of the exam is to exclude other causes of a CHL, such as cholesteatoma, tympanosclerosis, and middle ear effusion or masses. Even with advanced otosclerosis, the tympanic membrane is normal, the middle ear space is pneumatized, and the malleus should move with pneumatic otoscopy. In active disease, the astute clinician may appreciate a reddish blush (Schwartze sign) over both the promontory and the oval window niche owing to the prominent vascularity associated with an otospongiotic focus.
Tuning fork tests (Rinne and Weber) should be carefully performed at 256, 512, and 1024 Hz to confirm the findings of the audiogram. Weber testing should lateralize to the ear with the greatest conductive deficit and a negative Rinne test (bone conduction greater than air conduction) at 512 Hz usually indicates an air-bone gap of at least 25 dB (Table 51–1).
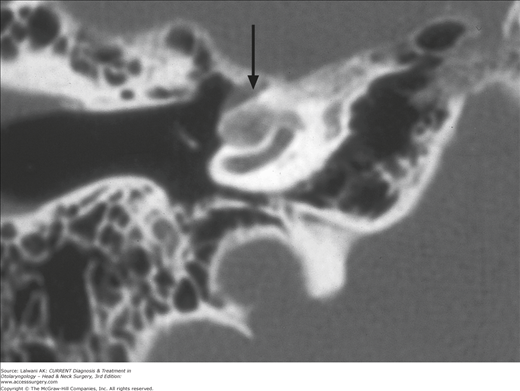
High-resolution CT scanning (less than 1 mm slices) provides excellent visualization of the anatomy of the middle ear and otic capsule and for this reason is the initial imaging modality of choice when the diagnosis is in question. It is valuable in assessing the pathology of the oval window and footplate, and the extent of otic capsule involvement and may also be helpful in identifying contralateral subclinical disease. CT scanning may show subtle areas of demineralization, which are typically located just anterior to the oval window (Figure 51–1), as well as thickening of the footplate. In a recent study examining 209 cases of otosclerosis, 95.8% of patients having confirmed otosclerosis had identifiable preoperative findings on CT. With cochlear involvement, there is a demineralization of the otic capsule (Figure 51–2), which yields the so-called halo sign or double ring sign seen on CT as a low-density zone outlining the basal turn of the cochlea.
In the sclerotic phase of disease or after fluoride therapy, remineralization may occur and CT findings may be indistinguishable from the normal otic capsule. A CT scan is not necessary in most cases but should be considered when the patient has vertigo, SNHL, poor word recognition or if there is a concern for superior semicircular canal dehiscence syndrome. A CT scan is routinely obtained in pediatric patients given the extremely low prevalence in this age group and because of the higher risk of otic capsule and temporal bone malformations.
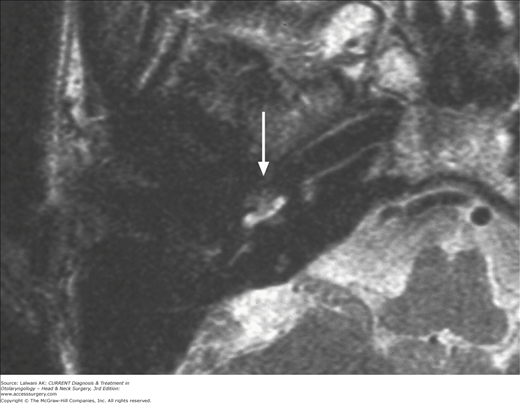
MRI provides very limited information regarding otic capsule pathology and is not obtained for routine cases of otosclerosis. In patients with an atypical presentation (pediatric onset, vertigo, SNHL) MRI may detect congenital anomalies of the labyrinth, fibrosis within the cochlea and can exclude retrocochlear pathology, such as an acoustic neuroma. During active disease, T1-weighted images show a loss of normal signal void from the otic capsule. Soft tissue or intermediate signal density may be noted in or around the otic capsule, and contrast-enhanced T1-weighted images can show enhancement of the pericochlear otic capsule. T2-weighted images may be beneficial for preoperative cochlear implant evaluation; a reduction or loss of the normal fluid signal from the membranous labyrinth depicts intracochlear fibrosis or bone deposition, which may hinder full electrode insertion (Figure 51–3).
Figure 51–3.
Axial T2-weighted scan demonstrating the lack of normal fluid signal from the cochlea due to inflammation or obliteration (or both) of the lumen (arrow). This scan correlates fairly, closely, and anatomically to the axial CT scan of the same patient presented in Figure 51–2.
Given the relatively normal exam findings, audiometric testing is one of the most important tools in evaluating a patient suspected of having otosclerosis. Testing patients who have a mixed hearing loss or far-advanced otosclerosis can be problematic because of masking dilemmas and audiometer limits. An experienced audiologist is invaluable in providing accurate and complete information on this type of testing.
On pure-tone audiometry, patients with early otosclerosis present with progressive low-frequency CHL. As otosclerosis spreads to involve the entire stapes, an increase in mass compounds the progressive increase in stiffness, resulting in (1) progression of loss in the high frequencies, (2) a gradual widening of the air-bone gap, and (3) a flat audiogram configuration. In the absence of SNHL, pure conductive loss seen with a completely fixed stapes are limited to a 60 to 65 dB hearing level with a maximum air-bone gap across the frequency range. As the disease spreads to involve the cochlea, bone conduction thresholds increase, resulting in a mixed hearing loss in which most of the conductive components are confined to the low frequencies. Decreased bone conduction levels in high frequencies usually represent a true SNHL.
The hallmark of bone conduction thresholds in otosclerosis is the Carhart notch (Figure 51–4). This is characterized by the elevation of bone conduction thresholds of approximately 5, 10, and 15 dB at 500, 1000, and 2000 Hz, respectively. The Carhart notch is thought to result from the disruption of normal ossicular resonance, which is approximately 2000 Hz. It is therefore a mechanical phenomenon and not a true reflection of cochlear reserve since it reverses after successful surgery (see Table 51–1).
Figure 51–4.
Audiogram demonstrating a CHL with a characteristic elevated bone threshold near 2000 Hz (Carhart notch). A type As tympanogram is caused by decreased tympanic membrane compliance. This pattern is often seen in otosclerosis but other conditions such as tympanosclerosis can mimic this finding.
The gradual stiffening of the ossicular chain produced by progressive stapes fixation leads to specific patterns of change on tympanometry. Because middle ear aeration is not affected by otosclerosis, patients with early- and mid-stage disease characteristically have a normal Type A tympanogram. Progressive stapes fixation results in a Type AS (A-shallow) tympanogram (Figure 51–4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree