Chapter 39 Orbital tumors can affect both the afferent and the efferent visual system including the optic nerve, ocular motor cranial nerves, extraocular muscles, and the position of the eye in the orbit. Some tumors are benign, relatively harmless, and require no treatment, whereas some are malignant and are a threat to visual and systemic morbidity and mortality. Thus, early diagnosis is important so that proper and timely therapy is initiated. It is important to refer patients with orbital tumors to the ophthalmologist trained in managing these diseases. Imaging studies and better instrumentation have greatly improved our ability to diagnose and manage orbital tumors.1 Sudden loss of vision associated with an orbit tumor, acute proptosis, or signs of an orbital tumor in a child require urgent evaluation by an ophthalmologist, neuro-ophthalmologist, or orbital surgeon. The presenting complaint and temporal sequence of events are important. Orbital tumors in adults and children are quite distinct (Table 39–1). Loss of vision followed by proptosis is most likely the feature of an optic nerve glioma, whereas the reverse is true of other intraconal masses. A history of previous surgical procedure, sinus disease, breast or lung masses, postural and diurnal variation in proptosis (varix), pulsations, trauma, and skin lesions is helpful in narrowing the differential diagnosis of an orbital mass. This is discussed in detail in Chapters 13 and 14, as well as later in this chapter.
ORBITAL TUMORS
URGENCY OF EVALUATION
DIAGNOSIS
SYMPTOMS
Primary | Direct Extension (Secondary) |
Adults | Eyelid |
Cavernous hemangioma Fibrous histiocytoma Benign lymphoid hyperplasia | Sebaceous, squamous, and basal cell carcinomas |
Lymphoma | Eye |
Meningioma | Malignant melanoma |
Neurilemmoma | Retinoblastoma |
Lacrimal gland tumor Pleomorphic adenoma Adenoid cystic carcinoma | Sinus Squamous cell carcinoma Cranium |
Arteriovenous fistula and varix | Meningioma |
Children | Metastatic |
Dermoid cyst | Adults |
Capillary hemangioma Optic nerve glioma | Lung, breast, prostate, gastrointestinal tract |
Lymphangioma | Children |
Rhabdomyosarcoma | Neuroblastoma, Wilms’ tumor |
SIGNS
Proptosis (see Chapter 14)
Protrusion of the globe is the most frequent manifestation of an orbital tumor. However, the commonest cause of both unilateral and bilateral proptosis in adults is Graves’ disease (Chapter 38), whereas in children it is orbital cellulitis (Chapter 40). Proptosis can be axial (forward displacement), superior (inferior lesion), or inferior (superiorly placed mass). Some implications of proptosis directions include:
• Axial: Optic nerve glioma, cavernous hemangioma
• Superior: Tumor of floor of orbit
• “Down and Out”: mucocele of frontal sinus
• “Down and In”: lacrimal gland tumor
Note: True proptosis should be distinguished from pseudoproptosis. The differential diagnosis of the latter includes unilateral high-axial myopia, shallow orbit (as in Crouzon disease), orbital asymmetry, asymmetric palpebral fissures (e.g., retraction of the upper eyelid in Graves’ disease), contralateral enophthalmos, and Horner’s syndrome of the opposite eye.
Other Signs
Palpation around the globe may reveal a mass in the anterior orbit. The regional preauricular and submandibular lymph nodes should be palpated. Fundus examination may reveal retinal folds, dilated retinal veins, or shunt vessels on the optic disc. Specific periorbital changes can provide clues to the diagnosis in some cases of orbital tumors.2 Examples include:
• Salmon-colored mass (suggests lymphoproliferative disorders)
• Vascular discoloration (blue suggests lymphangioma, or varix, red suggests capillary hemangioma)
• Ecchymoses (suggests neuroblastoma or leukemia)
• S-shaped lid (suggests plexiform neurofibroma)
• Corkscrew (arterialized) conjunctival vessels (suggests arteriovenous fistula)
• Frozen globe (suggests metastasis or adenocarcinoma of the lacrimal gland)
• Enophthalmos (suggests metastatic scirrhous carcinoma of breast, resulting from fibrosis and shrinkage)
• Increased resistance to retropulsion (suggests a posterior orbital mass)
• Orbital bruit on auscultation with a stethoscope over closed eyelids (suggests arteriovenous fistula or an orbital bony defect, as in neurofibromatosis)
ANCILLARY TESTS
The Hertel exophthalmometer is usually used to measure the amount of protrusion from the lateral orbital rim to the anterior corneal surface. A difference greater than 2 mm between the two eyes is significant and suggestive of proptosis.3 Although orbital ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) have dramatically improved diagnostic accuracy, these should not be used to replace a thorough clinical examination. For most orbital lesions, CT scanning is the preferred imaging technique as it provides excellent spatial resolution and bony detail. MRI is better for soft tissue detail. Laboratory workup is necessary to rule out other inflammatory, infectious, systemic (lymphoma), and metastatic orbital disorders.
TREATMENT
All orbital tumors do not need surgical removal. Small, asymptomatic tumors are best left alone and observed, and removed only if there is progression or symptoms. Most benign and malignant tumors of the orbit can be treated by surgical excision alone. Some malignant lesions may require additional radiation and chemotherapy with or without exenteration (removal of globe, eyelids, and retrobulbar orbital tissues). A team approach involving an orbital surgeon, neurosurgeon, oncologist, radiation oncologist, and neuroradiologist is essential in managing malignant orbital tumors.
Tissue diagnosis can be obtained using one of three approaches: fine-needle aspiration biopsy, excisional biopsy (complete removal of the tumor along with its capsule), or an incisional (small representative tissue sample) biopsy. Results of imaging are very helpful in making this decision. The differential diagnosis of a very well circumscribed lesion seen on a CT scan of the orbit include a cavernous hemangioma, schwannoma, fibrous histiocytoma, and hemangiopericytoma. The management of these lesions involves an orbitotomy with an excisional biopsy of the tumor. In contrast, an incisional biopsy is more appropriate for a diffuse mass (inflammatory pseudotumor, lymphoma, some metastatic tumors), as a complete removal would be technically difficult. A frozen section tissue examination may be necessary to plan the surgical approach in these cases. If a patient with a known history of cancer with metastases presents with an anterior orbital mass, a fine-needle aspiration biopsy can confirm the diagnosis and avoid an unnecessary orbitotomy.
SURGICAL APPROACHES
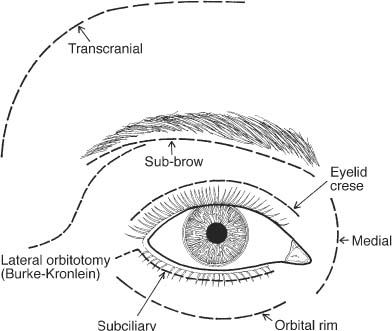
The various surgical approaches to the orbit are outlined in Fig. 39–1. In general, a sub-brow, lid-crease, conjunctival, subciliary, orbital rim or a medial incision best approaches the tumors of the anterior orbit. The best approach for a mid-orbital, intraconal lesion is a lateral orbitotomy performed by a lazy-S or a modified Burke-Kronlein incision. The incision starts lateral to the supraorbital notch just beneath the lateral half of the brow, extending inferolaterally along the orbital rim, past the lateral canthal angle, and ending over the zygomatic arch just medial to the hairline.4 A combined craniotomy-orbitotomy is the best approach for a tumor located at the orbital apex. Although the previous should serve as a broad general approach, careful planning and individual surgeon experience is very important to achieve the best result.
FIGURE 39–1 Surgical approaches to the orbit for anterior, midorbital, and apical tumors of the orbit.
Complications of Orbital Surgery
Sound knowledge of orbital anatomy is vital to avoid damage to important neurovascular structures in the orbit that may result in ischemia, diplopia, or hemorrhage. The most serious complication is visual loss from optic nerve injury (mechanical, cautery, vascular compromise).
COMMON ORBITAL TUMORS CLASSIFICATION (TABLE 39–1)
Orbital tumors are best classified as (1) primary tumors; (2) involving the orbit secondarily from neighboring structures; and (3) from metastases. Orbital lesions are also quite distinct in children and adults. The common tumors in childhood include dermoid cyst (most common), lymphangioma, capillary hemangioma and optic nerve glioma. In adults, cavernous hemangioma, schwannoma, fibrous histiocytoma, lymphoma, pleomorphic adenoma of the lacrimal gland, and meta-static lesions are common.5
INFLAMMATORY LESIONS MASQUERADING AS A TUMOR (SEE CHAPTERS 38 AND 40)
• Acute and chronic orbital cellulitis
• Graves’ ophthalmopathy
• Pseudotumor
• Mucormycosis
These conditions are described at length in Chapters 38 and 40.
DERMOID CYST
Symptoms and Signs
Dermoid cysts are the most common orbital tumor of childhood6 and represent 80% of all cystic orbital lesions and 24% of all orbital and eyelid lesions. They may lie superficially or deep in the orbit. Superficial lesions present early, typically along the bony suture lines in the superolateral or superonasal quadrants. They present as a slowly enlarging, smooth, painless, solitary, oval, firm mass, free from the overlying skin. In contrast, the deep lesions are seen in both adults and children and present as a painless, slow-growing proptosis. Spontaneous rupture can result in a marked orbital inflammation.
Ancillary Tests
Ultrasonography of superficial lesions demonstrates a medium to high internal reflectivity, whereas deep lesions demonstrate a low-to-absent internal reflectivity. CT scan demonstrates a well-defined lesion with an enhancing rim and some calcification that may be associated with a bony defect.
Pathology
Dermoid cysts are developmental choristomas, lined with stratified squamous epithelium and filled with keratin debris, oily material, and hair shafts.
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree