Orbital Surgery
Robert C. Kersten
Jeffrey A. Nerad
H. Jane Kim
Neoplasms involving the orbit are uncommon. Their proper treatment requires a detailed knowledge of orbital anatomy and the clinical manifestations of orbital diseases and appropriate diagnostic assessment of these manifestations. A thorough understanding of the natural history of the various orbital disorders is essential to determine the need for appropriate surgical intervention and the optimal surgical approach.
PREOPERATIVE EVALUATIONS
History and Physical Examination
A wide range of signs and symptoms may alert the ophthalmologist to involvement of the orbit by a pathologic process. These include proptosis or globe displacement; compressive optic neuropathy with visual field or visual acuity loss; refractive changes such as progressive hyperopia, restricted eye movements, and diplopia; optic disc changes, including pallor or edema; and fundus changes such as choroidal folds. These manifestations may be the consequences of a primary intraorbital disease or may occur secondary to involvement of the orbit by a process extending from the overlying soft tissues, periorbital sinuses, or intracranial cavity.
All patients with suspected orbital pathology should have a thorough ophthalmic history and physical examination. Detailed questioning about the nature, onset, and progression of the chief complaint is necessary to formulate a differential diagnosis. Previous ocular and general medical history related to diseases, operations, medications, and family history should be obtained. A general review of systems will identify risk factors for related systemic diseases, such as hyperthyroidism, metastatic cancer, or lymphoma. A complete examination of the eye and periocular tissues is essential. Abnormal protrusion or displacement of the globe, extraocular motility disturbances, soft-tissue changes, and decreased corneal or periorbital cutaneous sensation should be specifically sought. Special attention always should be directed to evaluation of optic nerve function. Visual acuity testing alone is not sufficient because visual acuity is often preserved initially in patients with compressive optic neuropathy. All patients should be examined closely for detection of an afferent pupillary defect, abnormal color vision, or loss of contrast sensitivity. Formal perimetry should be performed to rule out peripheral field loss. If the presentation has been gradual, evaluation of old photographs may help establish the time course of the pathologic process. In selected cases, appropriate blood work to help identify orbital inflammatory or neoplastic processes should also be obtained.
Orbital Imaging
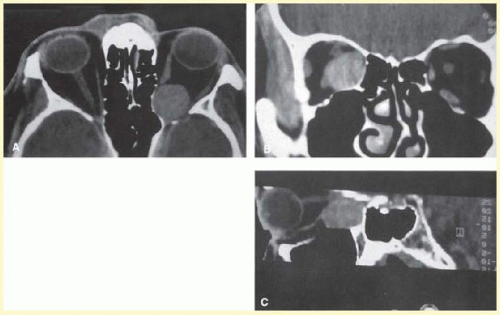
Valuable information about the nature and extent of an orbital pathologic process is provided by imaging studies such as CT scan, MRI, and orbital echography. Orbital fat provides a natural contrast between most adjacent orbital structures on CT scanning, and orbital bones are visualized well. CT is essential for evaluation of the orbital bones because they cannot be imaged with MRI. Direct coronal or sagittal images are important to identify the relationship of a lesion to the optic nerve so that the surgical approach can be planned to avoid traversing the optic nerve (Fig. 86.1). CT has the disadvantages of radiation exposure and limited soft-tissue differentiation.
Order CT of orbits and sinuses, including cavernous sinus with 1.5-mm cuts, especially if suspecting foreign body or direct traumatic optic neuropathy. Order intravenous contrast if suspecting inflammatory, infectious, or vascular lesions. Newer multislice helical CT scanners allow continuous acquisition of data, so that a single rapid pass allows formatting in axial, coronal, and sagittal planes. Multislice CT provides shorter examination times with reduced motion artifact and radiation exposure when compared with conventional CT.
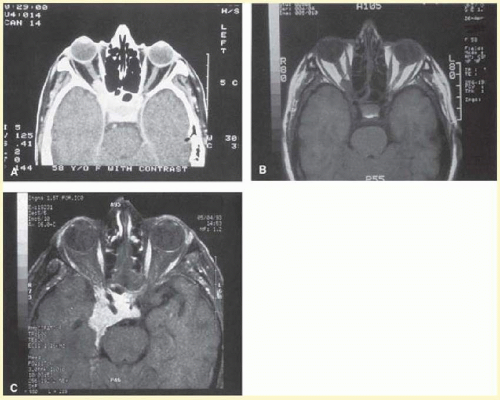
MRI is useful in selected cases, especially when evaluating the orbital cranial junction.1,2,3 Significant bony artifact and a lack of orbital fat in the orbital apex make CT scan resolution of the orbital apex structures poor. Because cortical bone has low signal on MRI, there is no bone artifact when viewing the orbital apex on MRI. The lack of intervening fat in the apex to provide contrast is overcome on MRI because contrast is provided by the individual nuclear characteristics of each tissue so that the orbital apex structures are visualized well. Consequently, conditions that affect the optic nerve and chiasm, such as optic nerve meningioma and glioma, generally are evaluated with MRI rather than CT scan (Fig. 86.2).
Order MRI of orbits and sinuses, including cavernous sinus with fat suppression with thin cuts through the orbits and gadolinium contrast, especially for suspected optic nerve lesions. Renal function test must be carried out before gadolinium-based contrast is ordered because gadolinium is generally contraindicated in individuals with renal dysfunction to avoid rare but serious complication known as nephrogenic systemic fibrosis/nephrogenic fibrosing dermopathy.4 Use of a contrast agent can further enhance the T1 signal intensity of lesions and is particularly helpful in imaging areas where there has been a breakdown in the blood-brain barrier. Because orbital fat produces a bright signal on T1-weighted images, orbital MR usually is performed with “fat suppression” to prevent masking of lesions. However, incomplete fat suppression can produce artifacts that may be misinterpreted as abnormal enhancement.
A few other orbital conditions are better visualized with MRI than CT scanning.1,2,3 Often, organic foreign bodies, such as wood, are not imaged well with CT scan. These foreign bodies are often visible with MRI. However, care must be taken when imaging any metallic intraocular or intraorbital foreign body because the strong magnetic field of the MR scanner may cause the foreign body to shift position or cause thermal damage to surrounding structures. In some tumors and vascular anomalies, high blood flow is appreciated on MRI. This is caused by a lack of signal, known as a flow void, created by blood flowing rapidly through larger vessels. Tumors that originate in the brain and extend into the orbit secondarily, such as sphenoid wing meningioma, are also visualized well with MRI. However, bony detail and calcification within the meningioma are not imaged well. In unusual circumstances such as this, CT scan and MRI may prove to be complementary, and both techniques may be required to fully evaluate the orbital disease process.
Orbital echography can provide useful information in the evaluation of orbital disorders. Because each tissue has its own acoustic characteristics, echography can provide a high degree of tissue contrast. Spatial resolution is also quite good. In some situations, echography can provide information not available on CT scan or MRI. These instances include detection and measurement of blood flow5 and intraoperative localization of small foreign bodies.6 Orbital echography requires specialized equipment and a large amount of expertise to obtain the detailed information that is readily available with CT scan or MRI; consequently, its use has decreased. Recent advances in orbital imaging have been summarized by Lee and colleagues.7
PREOPERATIVE CONSIDERATIONS
As in any surgical procedure, appropriate preoperative communication with all members of the surgical team is necessary. This communication starts with an informed consent to the patient. An explanation of the procedure as well as the specific goals and risks of the orbitotomy is given. Hemostasis in orbital surgery is paramount as orbital hemorrhage can result in orbital compartment syndrome and ischemic optic neuropathy. Antithrombotic therapy should be discussed, and pros and cons of stopping the agents must be weighed for the individual patient and the planned procedure.8 Withholding medications and dietary supplements with anticoagulant effects is preferred for extensive orbital surgeries and is done under the guidance of patient’s primary physician and cardiologist if applicable. American College of Chest Physicians clinical guideline states that 10% to 14% of platelet function is restored for each day after interruption of antiplatelet agent (e.g., aspirin, clopidogrel, ticlopidine) and recommends resuming 12 to 24 hours postoperatively.9 Therefore, 5 days of cessation of antiplatelet confers effective reversal of anticoagulation. In case of warfarin, the anticoagulant effect is halved approximately every 36 to 42 hours; therefore, after 5 days of interruption, most anticoagulant property should be eliminated.9 If the patient is at high risk of thromboembolic complications, it may be necessary to replace warfarin with subcutaneous low molecular weight heparin to be discontinued 24 hours prior, or intravenous heparin, to be discontinued 4 to 6 hours prior to surgery. Preoperative control of hypertension must be optimized. This is probably more important in minimizing surgical bleeding than anticoagulation status in our experience. Appropriate general preoperative laboratory tests are undertaken, depending on the patient’s age and type of anesthetic used. Communication with the operating room staff about additions to the routine instrumentation helps to avoid delays once the operation has started. Preoperative discussion with the anesthesiologist may be required to review the patient’s specific medical condition or operative concerns regarding intraoperative blood pressure or possible blood loss. In some cases, collaboration with other surgical specialists, such as a neurosurgeon, otolaryngologist, or pathologist, is necessary. The surgical plan should be discussed before the team enters the operating room.
INTRAOPERATIVE CONSIDERATIONS
Each surgical approach to the orbit offers its own specific challenges; however, there are several general considerations that make any orbitotomy more successful. These include adequate exposure, proper instrumentation, and good hemostasis. It is also important to have intraoperative flexibility to alter the surgical plan when necessary. Finally, surgical specimens must be handled carefully and submitted properly to obtain the maximum amount of information from the orbitotomy.
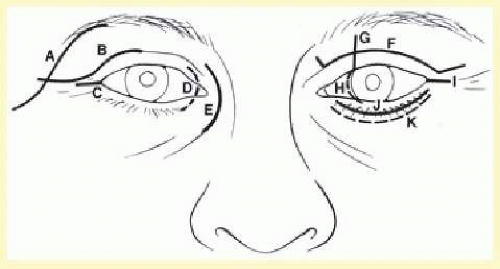
Incisions around the orbit are planned with two key considerations in mind. The first is to allow the most direct access to the lesion, and the second is to allow optimal scar camouflage. Incisions may be hidden by placing them within the hairline or brow, in the bulbar conjunctiva, or in the palpebral conjunctiva of the lower lid. Alternatively, external incisions may be disguised by placing them in preexisting upper or lower eyelid creases or in lateral canthal rhytides (Fig. 86.3).
Adequate exposure begins with marking the appropriate conjunctival or skin incision. The majority of conjunctival incisions heal without visible scar tissue. However, every skin incision leaves a somewhat visible scar. Thus, there is a tendency to mark as small a skin incision as possible. In some cases, the incision is too small to adequately expose the orbital mass. Hesitation in making a long enough skin incision can be minimized by camouflaging skin incisions as described. Once the skin incision is marked, local anesthetic containing 1:200,000 epinephrine is injected into the adjacent skin. This is done before the surgeon scrubs so that there is sufficient time for vasoconstriction to occur before the skin incision is made.
While the surgeon scrubs, the operating room personnel prepare and drape the patient. The operating room staff should be instructed to prepare and drape a generous surgical field. It is usually helpful to prepare and drape both orbits within the field, so that the contralateral side may be used as a reference to judge symmetry. Skin incisions usually are made with a No. 15 scalpel blade or a Colorado microdissector needle. Although an adequatelength incision should be made, it is often surprising how extensively the deeper structures can be exposed through a small skin incision when there is wide elevation and retraction of deeper soft tissues overlying the periosteum. If the choice of incision or length of incision is inadequate, the surgical plan should be modified to allow appropriate exposure. Often it is possible to start with a shorter incision, lengthening it if it restricts access.
Visualization of deeper orbital tissues involves appropriate retraction of overlying soft tissues. Individual 4-0 silk sutures placed in the subcutaneous tissues offer a large degree of flexibility in retracting the skin and subcutaneous tissues. A variety of orbital retractors should be available for each case. The value of an experienced assistant to provide adequate retraction and exposure cannot be overemphasized.
INSTRUMENTATION
Orbital surgery requires special instrumentation. Familiarity with and use of these instruments are essential for efficient orbital surgery. Proper instrumentation begins with illumination. Overhead operating room lights provide useful illumination for superficial parts of the orbitotomy. Except for somewhat superficial anterior orbitotomies, these overhead lights provide inadequate illumination to complete the orbitotomy. A fiberoptic headlight is extremely helpful for working more deeply within the orbit.
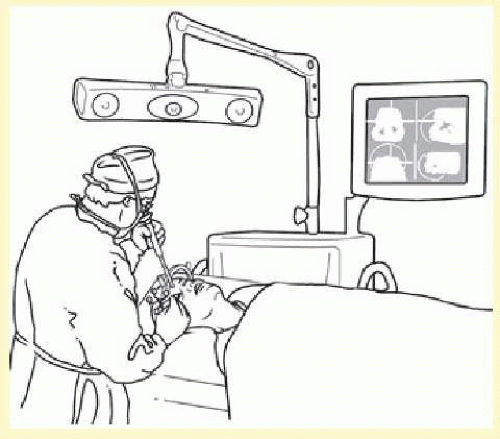
To detect the subtle differences in color and texture of the many orbital tissues, magnification is helpful. Surgical operating loupes are used routinely by most surgeons. Many varieties of surgical loupes are available. Custom-fit operating loupes with the surgeon’s individual near and distant prescription provide the best fit and comfort. Magnification of 2.5× with a working distance of 14 to 16 in is standard for most orbital procedures. Higher-powered operating loupes are available, but they are somewhat awkward to work with and limit the field of view. An operating microscope is recommended for higher levels of magnification. Maximum benefit is obtained with a microscope on a counter-weighted stand, similar to those used by most neurosurgeons. These stands allow upright positioning of the microscope on the X-, Y-, and Z-axes. The use of a 300-mm objective lens attached to the microscope permits the longer instruments used in orbital surgery to be placed into the operative field without contamination by inadvertent contact with the microscope. One of the most significant benefits of an intraoperative microscope is that it allows both the surgeon and the assistant to simultaneously visualize the depths of the orbital incision. The operating microscope can also be attached to a video monitor so that the operating room staff can be more involved in the procedure, and the operation may also be videotaped.
A variety of specialized orbital instruments, including retractors, dissectors, and bone-cutting tools, are available. Standard orbital retractors include several sizes of Sewall and malleable ribbon retractors. Retractors are useful in dissecting through the orbital fat; in addition, they offer exposure once the mass is identified. Placement of neurosurgical cottonoids beneath the retractor helps to keep orbital fat from prolapsing into the wound. Several types of periosteal elevators are useful; the most common is a Freer periosteal elevator. Numerous air-driven bone saws and drills are available. Bone rongeurs of several sizes should be on the surgical instrument tray. One of the various orbital miniplating or microplating systems may be useful for reattaching bone flaps and reconstructing bony defects. A retinal or glaucoma cryoprobe is helpful for applying traction to encapsulated solid or cystic orbital masses to facilitate their dissection from surrounding orbital tissues. For combined sinus and orbital surgery, the use of a nasal endoscope sometimes is helpful. Techniques involving many of these instruments frequently are not emphasized in ophthalmic residency training. Familiarity in these instruments must be obtained before beginning orbital surgery.
COMPUTERIZED IMAGE-GUIDED INTRAOPERATIVE NAVIGATION
In recent years, computerized image-guided systems have been devised to display the location of anatomic structures intraoperatively, often referred to as surgical navigation technology. The position of a probe in the surgical field is visualized in real time on a computer screen adjacent to the operating table that displays the patient’s preoperative imaging. The most common applications are where the anatomy is complex with many vital structures are situated in close proximity. The technique is fascinating and worthy of explanation.
There are three steps in the image guidance process: (1) preoperative imaging, (2) intraoperative registration of anatomic landmarks with the scans, and (3)intraoperative navigation. Before preoperative imaging, markers (known as fiducials) are placed on the patient’s skin, usually behind and above the ear. The position of the fiducials can be seen on the scans. In the operating room, the patient, the probe, and the computer are linked in the registration process. A “camera” linked to the computer “sees” the probe as the surgeon touches a fiducials on the patient with a probe. The exact three-dimensional position of the probe is recorded in the computer. The registration process continues in a similar manner, linking each fiducial on the patient with its position on the computer image. Additional registration points are linked using anatomic landmarks such as the tragus. The more points that are registered, the higher the accuracy of the subsequent navigation. The operation proceeds in normal fashion. When confirmation of the location of any anatomic structure is desired, the probe is placed into at that position, the camera “sees” the probe, and the computer shows the position of the probe on the monitor (Fig. 86.4). Different probe configurations allow simultaneous positioning of more than one probe. It is possible to use a drill or suction catheter as a probe so that the intraoperative position of these devices can be visualized while being used. The accuracy of intraoperative navigation can be in the submillimeter range if high-resolution scans and accurate registration are used.
Functional endoscopic sinus surgery and skull base operations are examples of procedures in which complex anatomy exists, often with variation from patient to patient or even side to side. Disease processes such as tumors or polyps can distort the anatomy as well. In these cases, the time spent in setting up the equipment and registering the system can be worthwhile. Surgical navigation has been used in orbital surgery, especially intraorbital foreign body removal or those orbital cases involving combined sinus and intracranial approaches. No doubt new innovations in imaging and computer technology will expand the uses of image guidance systems.
HEMOSTASIS
Control of bleeding is one of the most important skills an orbital surgeon must learn. Obtaining hemostasis begins in the office with specific questioning of the patient about the use of aspirin, nonsteroidal anti-inflammatory drugs, and vitamins and dietary supplements. Frequently, the patient will not regard these over-thecounter medications as important. Discontinuation of anticoagulants and antiplatelet medications may have serious adverse outcomes and should be undertaken in conjunction with the patient’s medical doctor. Although the need to routinely discontinue anticoagulant medications before performing all ophthalmic plastic procedures has been questioned,8 orbital hemorrhage carries a considerable risk of visual loss, and all attempts to optimize the patient’s coagulation parameters should be made before elective orbital surgery. Warfarin generally is stopped 5 days before surgery, and the patient’s international normalization ratio (INR) should be checked immediately preoperatively to ensure adequate hemostasis. At times it may be necessary to replace warfarin with heparin, which can be reversed 24 hours (low molecular weight heparin) or 4 to 6 hours (intravenous heparin) preoperatively if the patient is at high risk of thromboembolic complications. Patients being considered for elective orbital surgery should discontinue aspirin and other nonreversible platelet inhibitors for 5 days before surgery. Nonsteroidal medications are reversible platelet inhibitors whose effect diminishes as they are cleared from the circulation. The duration of the platelet often depends on the half-life of the drug, but it is usually recommended that the medication be discontinued 2 days preoperatively. Systemic hypertension should be brought under optimal medical control in the preoperative period. Significant intraoperative bleeding correlates more with intraoperative hypertension than any other variable.
Once in the operating room, the patient should be placed in the reverse Trendelenburg position to decrease venous pressure. The patient’s blood pressure should be strictly controlled in most cases, with the goal of maintaining the blood pressure at or slightly below the patient’s normal range. In patients with particularly vascular tumors, consideration should be given to hypotensive anesthesia with placement of an intra-arterial blood pressure monitor.
The vasoconstriction provided by the dilute epinephrine (1:100,000 to 1:200,000) mixed with local anesthetic helps to prevent bleeding when 1 or 2 mL is injected 10 minutes before incision. Small vessels are coagulated with bipolar cautery. When the surgeon is working away from the eyelids or orbit, unipolar cautery may be used to cut or coagulate the bleeding vessels. In general, unipolar cautery should not be used within the confines of the orbit because it may preferentially conduct along myelinated nerve fibers. When large arteries are encountered, aneurysm clips may be applied. Longhandled bayonet microsurgical bipolar cautery instruments are available for intraorbital and intracranial coagulation. Visualization is improved with Q-tips or “peanut”-type gauze dissectors to absorb small amounts of blood on the field. When bleeding is more vigorous, suction may be required to visualize bleeding vessels. Suction is facilitated by placing the suction tip against a cottonoid rather than on the orbital fat. Specialized suction tips are useful in the sinus. These suction devices may include irrigation or unipolar cautery. Bone wax, Gelfoam (absorbable gelatin sponge), Surgicel (oxidized regenerated cellulose), Avitene (microfibrillar collagen), Floseal (thrombin and collagen matrix), and Thrombogen (thrombin) are also available to facilitate coagulation.
In most orbitotomy cases, blood products are not required. In some cases where tumor resection involves other parts of the cranium or face, blood replacement may be required. In cases where resection of particularly vascular tumors is necessary, preoperative angiography with arterial embolization may be helpful. If there is concern about postoperative bleeding, a flexible vacuum drain may be used. Atraumatic extubation of the patient at the completion of the procedure is important to prevent increased venous pressure, which increases the risk of orbital hemorrhage.
INTRAOPERATIVE FLEXIBILITY
The ability to modify the surgical plan intraoperatively is necessary in orbital surgery. Inadequate exposure may be improved by extending the surgical incision or by more aggressive soft-tissue and periosteal elevation. Unexpected difficulties in exposing or making a safe biopsy of an orbital mass may require the use of combined surgical approaches, such as the addition of lateral orbitotomy, to a planned medial orbitotomy. Larger orbital procedures involving tumors that extend outside the orbit require a team approach in cooperation with surgeons from other disciplines. In these cases, as well as all orbital procedures, preoperative contingency plans for intraoperative modifications will make the orbitotomy more successful. In all types of surgery, the ability to modify the initial plan becomes easier with experience.
CARE OF THE SURGICAL SPECIMEN
Orbital tumors are rare. Frequently, the amount of tissue that is available is small. Consequently, great care must be taken in obtaining and handling the orbital biopsy specimen to ensure the most accurate diagnosis. Preoperative consultation with the ocular pathologist is advisable when an unusual diagnosis is suspected. Intraoperative frozen-section analysis of the biopsy tissue may be helpful in confirming that appropriate tissue has been sampled. Frozen-section diagnosis should be confirmed with permanent section analysis before decisions are made about disfiguring procedures such as orbital exenteration. Fresh tissue for flow cytometry and immunopathologic analysis should be obtained for all lymphoid lesions and is often of benefit in the diagnosis of many unusual orbital tumors. Occasionally, electron microscopy may be helpful. When the orbitotomy is performed for diagnostic reasons, the tissue must be treated delicately to avoid crush and drying artifact. Attention to these details will increase the diagnostic accuracy of the procedure.
CHOICE OF ORBITOTOMY APPROACH
To select the best surgical approach to an orbital lesion, the surgeon must know the location of the lesion and the structures to be traversed in reaching it and have a properly formulated working diagnosis. The diagnosis anticipates whether the lesion is expected to be encapsulated or diffuse, benign or malignant, and whether complete excision of the lesion is preferred or a biopsy followed by nonsurgical treatment is more appropriate. The orbital examination and review of orbital imaging studies usually suggest that the lesion is either benign or malignant; in many cases, a specific diagnosis is suggested. In general, well-outlined masses with smooth contours are likely to be benign. Tumors with diffuse borders and evidence of invasion into the surrounding tissues, including orbital fat or bone, are likely to be malignant. Exceptions to these rules exist (e.g., the smooth, well-outlined mass frequently seen in malignant lymphoma, or the diffuse borders apparently infiltrating into orbital fat found in idiopathic inflammatory disease of the posterior orbit).
INCISIONAL VERSUS EXCISIONAL BIOPSY
A thorough knowledge of orbital disorders guides the decision to treat medically or perform an incisional or an excisional biopsy. In some cases, such as suspected Graves’ ophthalmopathy or idiopathic inflammatory “pseudotumor,” medical treatment may be prescribed without the need for surgery. In other cases, orbitotomy may be required before treatment can be initiated. The differential diagnosis suggests whether the lesion is thought to be amenable to surgical excision or is a process in which surgery to establish a diagnosis is better followed by medical management or radiation therapy.
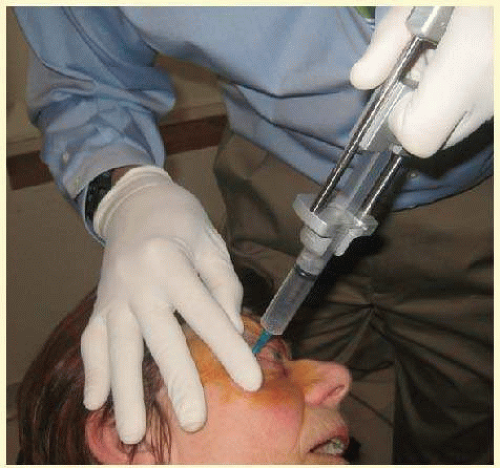
An incisional biopsy is performed when a representative piece of tissue is removed but some of the lesion is left behind. This type of biopsy is used to confirm a clinical diagnosis before proceeding with medical therapy or radiation therapy (e.g., lymphoma, orbital pseudotumor, rhabdomyosarcoma). It may also be used to obtain a tissue diagnosis before planning a definitive surgical treatment such as exenteration or extensive orbitocranial resection. In some cases, incisional biopsy provides a tissue diagnosis and is also used to debulk a tumor. Diffuse infiltrative orbital lesions usually require incisional biopsy to confirm the diagnosis before other therapy can begin. Fine needle aspiration biopsy (FNAB) of the orbit or lacrimal gland may be considered as a form of incisional biopsy. Accurate diagnosis was achieved in 47% to 92% in large case series10,11,12 There was good concordance between FNAB and histopathologic diagnosis for metastatic or secondary (from adjacent structures) malignant orbital process and decreased yield for benign tumors and lymphomas.11,12 When combined with advanced laboratory techniques (immunohistochemistry, flow cytometry, etc.), improved diagnostic yield for benign tumors and lymphomas has been reported.13 Potential complications and false readings have been reported.14 The technique is described well in the literature.10 Briefly, the needle entry is infiltrated with local anesthesia and the area of interest is well-exposed. A 23G or 25G needle is inserted into the lesion and passed several times in a twisting motion. Some surgeons prefer the needle to be attached to a syringe with a pistol grip vacuum plunger in which case suction is applied after the needle tip is embedded in the lesion and is released before needle exits the lesion to prevent aspiration of tumor cells into the syringe (Fig. 86.5). For deeper, nonpalpable lesions, Bscan or CT guidance can be used. A positive yield is immediately confirmed by cytopathologist and in the case of inadequate specimen, the biopsy is repeated.
An excisional biopsy is performed when an orbital mass is removed in its entirety. Excisional biopsy is performed on lesions that are believed to be benign, well localized, and easy to remove without damage to surrounding orbital tissues. As a general rule, well-circumscribed and encapsulated lesions are treated with excisional biopsy. This is especially important in cases of benign mixed tumors of the lacrimal gland or orbital dermoid cysts where incision through an intact capsule dramatically increases the chance of recurrence and orbital morbidity. In general, malignant lesions of the orbit are not amenable to excisional biopsies, because tumor-free microscopic margins cannot be obtained in orbital fat.
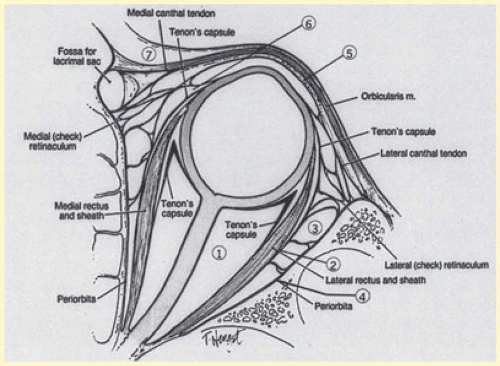
THE SURGICAL SPACES
The other important consideration in planning orbitotomy is the position of the tumor within the orbit. Lesions generally may be categorized as either anterior (superficial) or posterior (deep). They can be further categorized by their relationship to the optic nerve (medial, lateral, superior, or inferior to the optic nerve). It may be helpful to further classify the location of lesions relative to adjacent anatomic structures in the orbit. Many surgeons prefer to conceptualize orbital pathologic processes as being located within one or more of seven “surgical spaces” within or around the orbit (Fig. 86.6). These spaces include the following:
Central surgical space (intraconal space)
Extraocular muscles
Peripheral surgical space (extraconal space)
Subperiosteal space
Preaponeurotic space
Tenon’s space
Periorbital tissues
The central surgical space is bounded by the intermuscular septum, which connects the four rectus muscles in the coronal plane. This space is also described as the retrobulbar or intraconal space, and it contains the optic nerve, intraconal fat, and various vascular and neural structures. Primary orbital tumors such as cavernous hemangiomas or optic nerve meningiomas originate in the central surgical space.
Many orbital processes involve the extraocular muscles, primarily or secondarily, making it useful to classify the extraocular muscles as residing in their own separate surgical “space.” Conditions affecting the extraocular muscles include thyroid orbitopathy, myositis, and a variety of neoplastic conditions.
The peripheral surgical space, also known as the extraconal space, lies outside the intermuscular septum but within the periorbita. This space contains a scant amount of orbital fat, the superior oblique muscle and trochlea, inferior oblique muscle, and lacrimal gland. Other important nerves and vessels extend into the space, such as the superior ophthalmic vein. A variety of pathologic processes may encroach on the peripheral surgical space.
The subperiosteal space is a potential space lying between the orbital bones and the periorbita. The periorbita may provide a barrier to extension of neoplastic and infectious processes originating in the adjacent sinuses or intracranial cavity. Frequently, the subperiosteal space may fill with blood after orbital fracture or infection when associated with a paranasal sinusitis.
The preaponeurotic space is actually an anterior extension of the extraconal space. Because this space is superficial and readily accessible, sometimes it is referred to as its own orbital compartment. Frequently, neoplasms affecting the lacrimal gland, such as lymphoma, extend forward into the preaponeurotic space.
Tenon‘s space is a potential space between the sclera and the Tenon’s capsule. Tumors originating in the eye, such as choroidal melanoma, may extend into Tenon’s space.
Secondary orbital tumors may arise from periorbital tissues and secondarily invade the orbit. Cutaneous malignancies arising in the eyelid or facial skin may extend posteriorly through the orbital septum, whereas nasal and paranasal sinus tumors may grow through the orbital bones into or through the subperiosteal space. Tumors arising within the cranial cavity, such as sphenoid wing meningiomas, may also affect the orbit secondarily.
DEEP VERSUS ANTERIOR ORBITAL APPROACHES
In general, approaches to the orbit can be divided into two categories: those in which a lesion is sufficiently superficial that access may be achieved without removing the orbital walls, and those for deeper lesions in which orbital bones must be removed to gain access. The location of the lesion relative to the optic nerve further dictates the optimal approach. It is always desirable to avoid traversing the nerve while approaching a lesion so as to minimize traction on or trauma to the nerve, which may result in visual dysfunction.
Historically, an exploratory orbitotomy, often with removal of the lateral orbital wall, frequently was required to establish a diagnosis in patients with proptosis and a presumed orbital mass. Fortunately, modern advances in orbital imaging have allowed much more precise and sophisticated refinement of surgical approaches to the orbit.
A large number of innovative anterior surgical approaches have been developed over the years, and whenever possible, anterior approaches to the orbit are preferred to avoid the extra time and potential morbidity of bone removal and refixation. Although deeper orbital lesions may require access by lateral orbitotomy with removal of the lateral wall, transcranial orbitotomy with removal of the orbital roof, medial orbitotomy with removal of the ethmoid sinus (medial orbital wall), or inferior orbitotomy with removal of the orbital floor, increasingly lateral orbitotomy with elevation and incision of the lateral periorbita allow deep orbital access without the need to routinely remove the lateral bony wall.
There may be considerable overlap when characterizing lesions as either deep or superficial, and it is not always possible to determine whether a given external incision approach will or will not require removal of underlying bone to achieve the goals of the procedure. Although one cannot overemphasize the need for intraoperative flexibility when performing orbital surgery, for purposes of discussion here we segregate descriptions of deep and anterior orbital approaches.
DEEP ORBITAL APPROACHES
Lateral Orbitotomy
Lateral orbitotomy originally was popularized by Kronlein in 1888.15 The incision described by Kronlein was a reverse C-shaped incision placed over the lateral rim and extending superiorly toward the hairline and inferiorly toward the ear. This resulted in an unsightly scar and a high likelihood of damage to the seventh cranial nerve. Subsequently, a number of superior skin incisions have been devised to allow exposure of the bony lateral orbital wall and access to the lateral retrobulbar space.16,17,18 Currently, the lateral wall is most often approached through either a canthotomy incision (modified Berke)19 or an upper eyelid crease incision extending into a lateral “laugh line.”20 Rarely, a coronal incision in the hairline with subgaleal dissection of a scalp flap carried down to the lateral rim is useful.21,22
Although percutaneous dissection and orbital bone removal can be performed satisfactorily under local anesthesia, deeper orbital manipulation requires retrobulbar injection, which would alter postoperative pupillary evaluation and visual acuity checks. Because visual loss is a well-recognized complication of orbital surgery,23 most lateral orbitotomies are performed under general anesthesia to allow close postoperative monitoring of vision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree