 Orbital Primary Melanocytic Tumors
Orbital Primary Melanocytic TumorsOrbital Melanoma Arising from Ocular Melanocytosis and Blue Nevus
General Considerations
Primary melanocytic orbital tumors include melanoma, melanocytic hamartoma, and melanotic neuroectodermal tumor (MNET) of infancy (retinal anlage tumor). Primary orbital melanoma usually originates from congenital ocular melanocytosis or hypercellular blue nevus that affects the orbital tissue (1,2,3,4,5,6,7,8,9,10). Rarely, it can arise from the optic nerve (9) or after orbital irradiation for rhabdomyosarcoma (10). Melanoma from melanocytosis and from blue nevus are similar and are grouped together here. In the authors’ review of personal cases, the 10 primary orbital melanomas accounted for 1% of all orbital tumors (2).
Clinical Features
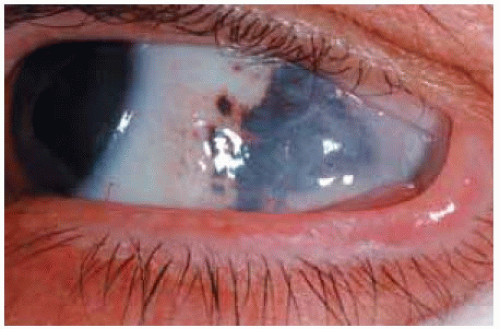
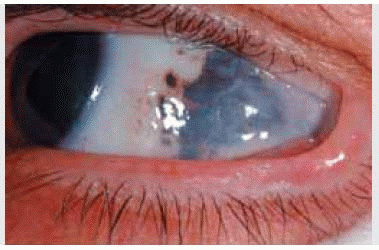
The underlying congenital melanocytic lesion may be evident anteriorly as ocular melanocytosis or blue nevus, but it is often subclinical in the orbit more posteriorly, until it spawns a melanoma later in life. The melanoma that arises from blue nevus or congenital melanocytosis is generally circumscribed, even though the underlying congenital pigmentation is diffuse or patchy. Proptosis in a patient with either congenital ocular melanocytosis or episcleral blue nevus should arouse suspicion for a primary orbital melanoma or orbital extension of uveal melanoma.
Diagnostic Approaches
Computed tomography (CT) and magnetic resonance imaging (MRI) show a circumscribed, enhancing mass in orbital soft tissue, usually in the extraconal space, sometimes in an extraocular muscle. MRI may help to detect the melanin content in the lesion. With time, the tumor can breach its pseudocapsule and diffusely invade the orbit. As part of a diagnostic workup for proptosis, the clinician should inspect the eyelid skin and episclera to look for a blue nevus and perform ophthalmoscopy to rule out uveal melanoma.
Pathology
Grossly and at surgery, orbital melanoma is generally a brown or black circumscribed mass. Microscopically, it is composed of spindle or epithelioid melanoma cells. In many cases, residual areas of cellular blue nevus can be identified. Extensive tumor necrosis is common. Immunohistochemistry demonstrates a positive reaction to melanoma-specific antigens.
Management
Because orbital melanoma is usually well circumscribed, an attempt should be made to remove the entire tumor intact. An incisional biopsy of a circumscribed orbital mass in the setting of congenital ocular melanocytosis is contraindicated if there is a chance of removing the tumor intact. We believe that orbital melanoma is more likely to recur locally or metastasize to distant organs if it is not removed intact. The surrounding flat congenital pigment should be examined at surgery, biopsied, and treated with heavy cryotherapy. Residual or recurrent orbital melanoma should usually be managed by eyelid-sparing orbital exenteration.
Selected References
1. Shields, JA, Shields CL. Orbital malignant melanoma. The 2002 Sean B. Murphy Lecture. Ophthalmic Plast Reconstr Surg 2003;19:262-269.
2. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
3. Gunduz K, Shields JA, Shields CL, et al. Periorbital cellular blue nevus leading to orbitopalpebral and intracranial melanoma. Ophthalmology 1998;105:2046-2050.
4. Tellado M, Specht CS, McLean IW, et al. Primary orbital melanoma. Ophthalmology 1996;103:929-932.
5. Dutton JJ, Anderson RL, Schleper RL, et al. Orbital malignant melanoma and oculodermal melanocytosis. Report of two cases and review of the literature. Ophthalmology 1984;91:497-507.
6. Wilkes SR, Uthman EO, Thornton CN, et al. Malignant melanoma of the orbit in a black patient with ocular melanocytosis. Arch Ophthalmol 1984;102:904-906.
7. Mandeville JT, Grove AS Jr, Dadras SS, et al. Primary orbital melanoma associated with an occult episcleral nevus. Arch Ophthalmol 2004;122:287-290.
8. Shields JA, Shields CL, Demirci H, et al. Experience with eyelid-sparing orbital exenteration: the 2000 Tullos O. Coston Lecture. Ophthal Plast Reconstr Surg 2001;17:355-361.
9. DePotter P, Shields CL, Eagle RC Jr, et al. Malignant melanoma of the optic nerve. Arch Ophthalmol 1996;114:608-612.
10. Lumbroso L, Sigal-Zafrani B, Jouffroy T, et al. Late malignant melanoma after treatment of rhabdomyosarcoma of the orbit during childhood. Arch Ophthalmol 2002;120:1087-1090.
Orbital Melanoma Arising From Blue Nevus
Wilkes SR, Uthman EO, Thornton CN, et al. Malignant melanoma of the orbit in a black patient with ocular melanocytosis. Arch Ophthalmol 1984;102:904-906.
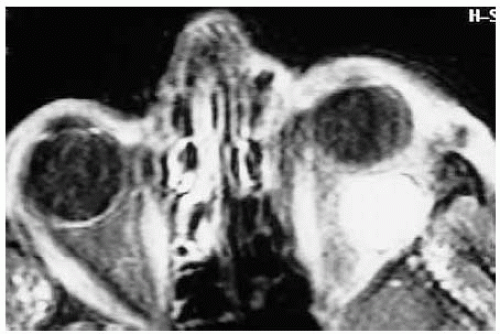 Figure 36.2. Axial orbital magnetic resonance imaging with gadolinium enhancement in T1-weighted image of patient shown in Figure 36.1. Note the circumscribed mass temporal to the optic nerve. At the time of surgery, marked pigmentation was found throughout the temporal portion of the orbit, including the sheath of the lateral rectus muscle. |
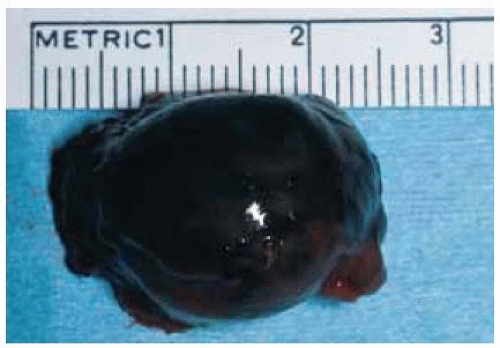 Figure 36.3. Appearance of the orbital mass shown in Figure 36.2 after surgical removal. Care was taken to remove the mass intact. |
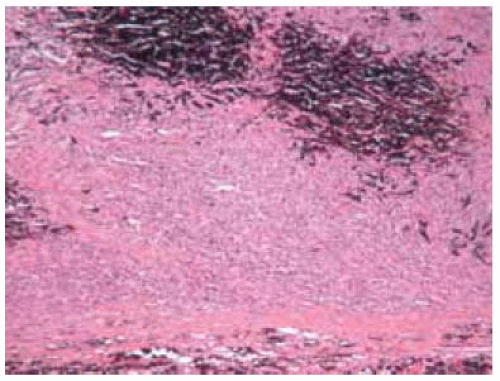 Figure 36.4. Histopathology of lesion shown in Figure 36.3 demonstrating densely pigmented blue nevus (above) and amelanotic spindle and epithelioid melanoma cells (below). (Hematoxylin-eosin 50.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|