 Orbital Peripheral Nerve Tumors
Orbital Peripheral Nerve TumorsOrbital Schwannoma (Neurilemoma)
General Considerations
Schwannoma (neurilemoma) is a benign, encapsulated tumor that arises from the Schwann cells that ensheath peripheral nerves. It can arise primarily in the orbit or extend into the orbit from adjacent peripheral nerves (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18). It accounts for about 1% of all orbital masses (1,2,3,4). In the authors’ series of 1,264 consecutive space-occupying orbital lesions, the 14 schwannomas accounted for 61% of the 23 peripheral nerve tumors and for 1% of all lesions. It was diagnosed at a median age of 37 years with a range from 10 to 84 years.
Clinical Features
Orbital schwannoma usually produces proptosis and displacement of the globe with signs and symptoms similar to those described for orbital cavernous hemangioma. Even though it is a tumor of peripheral nerve sheath origin, it does not usually cause pain. In contrast with neurofibroma, solitary orbital schwannoma is not usually associated with neurofibromatosis.
Diagnostic Approaches
Imaging studies disclose a solid ovoid to elongated mass usually outside the muscle cone along the course of the supraorbital or supratrochlear nerve and occasionally along the infraorbital nerve. Magnetic resonance imaging (MRI) reveals an enhancing mass with signals that vary depending on whether the tumor is solid or cystic. It shows very low signal on T1-weighted images and homogeneous postcontrast enhancement (10).
Pathology
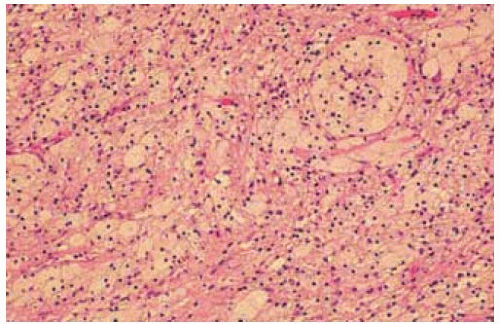
Histopathologically, schwannoma is a benign proliferation of Schwann cells that can show several variations in one tumor. Some areas are characterized by ribbons or fascicles of spindle cells (Antoni A pattern) and other areas have ovoid clear cells (Antoni B pattern). Large cystoid spaces are sometimes present and can even occupy most of the tumor, suggesting a cystic, rather than a solid lesion.
Ancient schwannoma is a variant of schwannoma that can be confused with a malignant mesenchymal tumor because of increased cellular, nuclear pleomorphism, and hyperchromatism. The variant often shows cyst formation, calcification, hemorrhage, and hyalinization (5).
Although there are no immunohistochemical stains that are specific for Schwann cells, immunohistochemistry can be used to exclude the diagnosis of other spindle cell tumors, like melanoma, leiomyoma, and rhabdomyosarcoma, thus lending support to the diagnosis of schwannoma. Electron microscopy can be used to demonstrate the cytoplasmic wide-spacing collagen that characterizes Schwann cells (1,5).
Management
The management of orbital schwannoma is surgical excision. Axial and coronal MRI and/or computed tomography (CT) are essential in determining the best approach to surgical excision. An incisional biopsy should generally not be done for this circumscribed orbital tumor. If the tumor is not completely excised at a fairly early stage, it can show progressive growth, attain a large size, and be more difficult to excise.
Selected References
1. Shields JA. Peripheral nerve tumors of the orbit. Neurilemoma (benign schwannoma). In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:152-157.
2. Shields JA, Bakewell B, Augsburger DG, et al. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 1984;102:1606-1611.
3. Shields JA, Bakewell B, Augsburger DG, et al. Space-occupying orbital masses in children. A review of 250 consecutive biopsies. Ophthalmology 1986;93:379-384.
4. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
5. Weiss SW, Goldblum JR. Benign tumors of peripheral nerves. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s Soft Tissue Tumors. 4th ed. St. Louis: CV Mosby; 2001:1146-1167.
6. DePotter P, Dolinskas C, Shields JA, et al. Peripheral nerve tumors. In: DePotter P, Shields JA, Shields CL, eds. MRI of the Eye and Orbit. Philadelphia: JB Lippincott; 1994:183-191
7. Rootman J, Goldberg C, Robertson W. Primary orbital schwannomas. Br J Ophthalmol 1982;66:194-204.
8. Shields JA, Kapustiak J, Arbizo V, et al. Orbital neurilemoma with extension through the superior orbital fissure. Arch Ophthalmol 1986;104:871-873.
9. Tsuzuki N, Katoh H, Ohnuki A, et al. Cystic schwannoma of the orbit: case report. Surg Neurol 2000;54:385-387.
10. Abe T, Kawamura N, Homma H, et al. MRI of orbital schwannomas. Neuroradiology 2000;42:466-468.
11. Khwarg SI, Lucarelli MJ, Lemke BN, et al. Ancient schwannoma of the orbit. Arch Ophthalmol 1999;117:262-264.
12. Carroll GS, Haik BG, Fleming JC, et al. Peripheral nerve tumors of the orbit. Radiol Clin North Am 1999;37:195-202.
13. Lam DS, Ng JS, To KF, et al. Cystic schwannoma of the orbit. Eye 1997;11:798-800.
14. Gunalp I, Gunduz K, Duruk K, et al. Neurogenic tumors of the orbit. Jpn J Ophthalmol 1994;38:185-190.
15. Shen WC, Yang DY, Ho WL, et al. Neurilemmoma of the oculomotor nerve presenting as an orbital mass: MR findings. AJNR Am J Neuroradiol 1993;14:1253-1254.
16. Rose GE, Wright JE. Isolated peripheral nerve sheath tumours of the orbit. Eye 1991;5:668-673.
17. Faucett DC, Dutton JJ, Bullard DE. Gasserian ganglion schwannoma with orbital extension. Ophthal Plast Reconstr Surg 1989;5:235-238.
18. Konrad EA, Thiel HJ. Schwannoma of the orbit. Ophthalmologica 1984; 188:118-127.
Orbital Schwannoma
Orbital schwannoma most typically occurs in the superior extraconal portion of the orbit and apparently arises from the sheath of the supraorbital nerve. When it is in that location, it is best approached by a superolateral orbitotomy. Most can be successfully removed by a soft tissue approach; osteotomy is only occasionally necessary. A clinicopathologic correlation is presented.
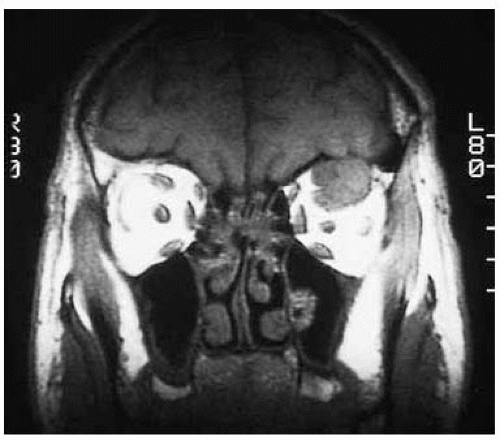 Figure 29.2. Coronal magnetic resonance imaging in T1-weighted image showing circum scribed superior orbital mass. The tumor is hypointense to orbital fat. |
 Figure 29.3. Sagittal magnetic resonance imaging in T1-weighted image showing ovoid shape of the superior orbital mass. |
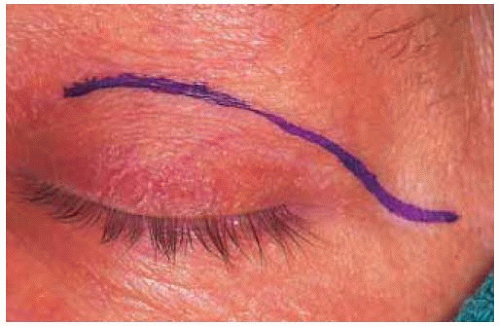 Figure 29.4. Outline of cutaneous incision for removal of the mass. The lesion was removed without complications. |
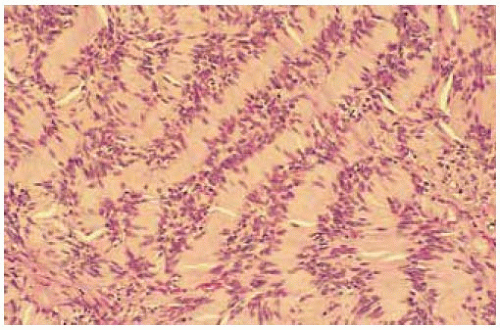 Figure 29.5. Histopathology showing an area of Antoni A pattern with fascicles of nuclei with a ribbon arrangement. (Hematoxylin-eosin 150.) |
Orbital Schwannoma
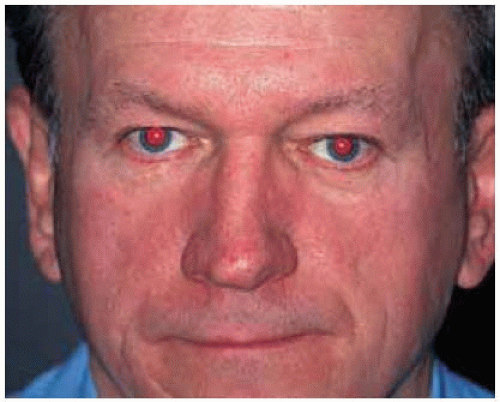
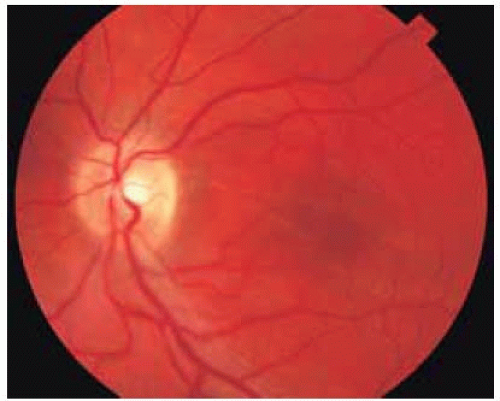
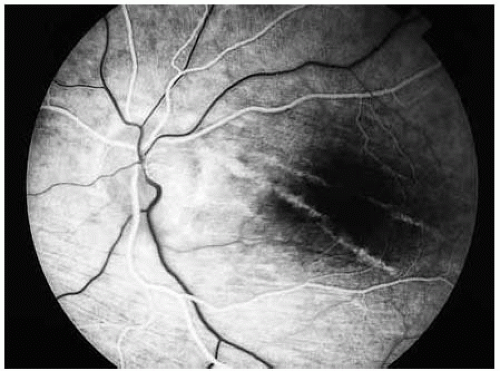
Orbital schwannoma is a benign, slowly growing tumor that can cause compression of the optic nerve and visual impairment. Once the tumor is removed, the optic disc swelling can resolve and the visual acuity can return to normal. However, the choroidal folds tend to remain.
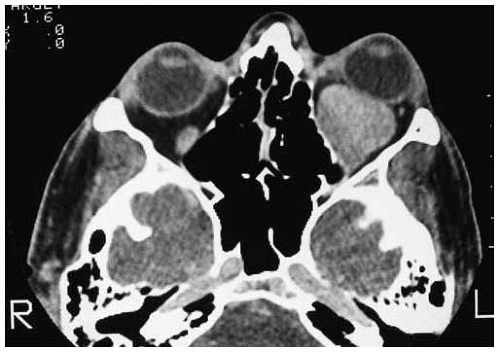 Figure 29.8. Axial computed tomography showing large superior orbital mass. Other sections showed compression of the optic nerve. |
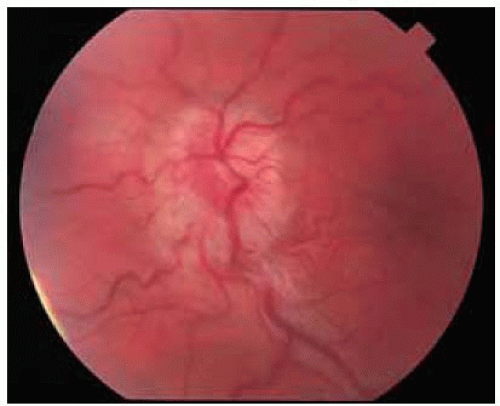 Figure 29.9. Fundus photograph showing edem a of left optic nerve, tortuous retinal blood vessels, and choroidal folds. Visual acuity was 6/60. |
 Figure 29.10. Gross appearance of the circumscribed tumor immediately after removal through a superolateral orbitotomy. |
Orbital Schwannoma
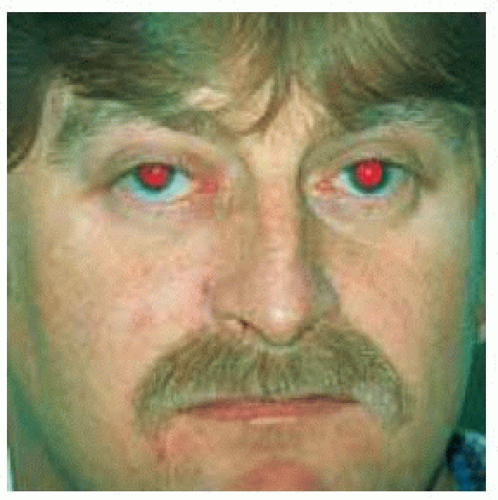
Because orbital schwannoma is a well-circumscribed, encapsulated tumor, it can sometimes be removed intact by way of lateral orbitotomy despite its large size and posterior location. Illustrated is a clinicopathologic correlation of a large schwannoma in a 33-year-old man who declined a recommended neurosurgical approach and sought another opinion to see if it could be removed without a craniotomy. It was removed intact by way of a superolateral orbitotomy despite the fact that it protruded posteriorly through the superior orbital fissure.
Shields JA, Kapustiak J, Arbizo V, et al. Orbital neurilemoma with extension through the superior orbital fissure. Arch Ophthalmol 1986;104:871-873.
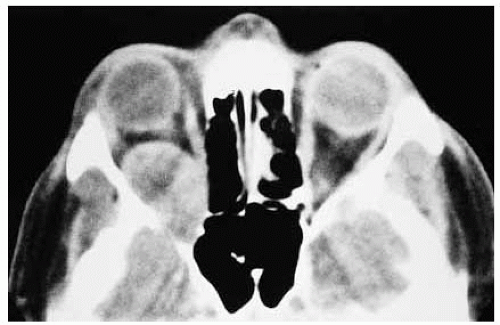 Figure 29.14. Axial CT showing a large, circumscribed mass occupying most of posterior orbit and extending through the superior orbital fissure into the brain. |
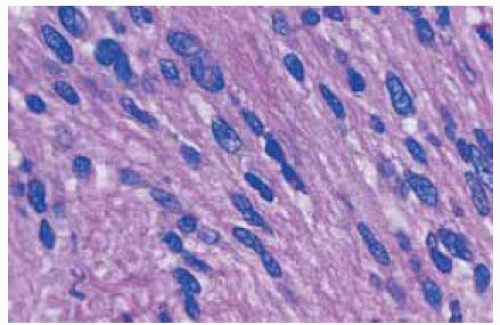 Figure 29.16. Histopathology of an area of tumor showing schwannoma with Antoni A pattem. (Hematoxylin-eosin 200.) |
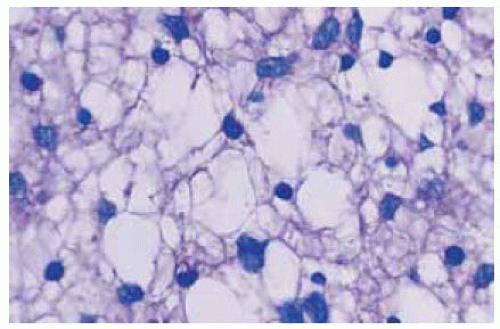 Figure 29.17. Histopathology of another area of tumor showing Antoni B pattem. (Hematoxylin-eosin 200.) |
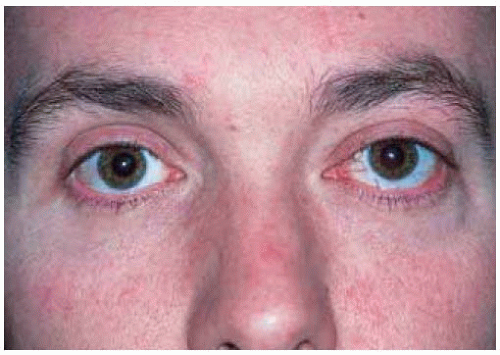
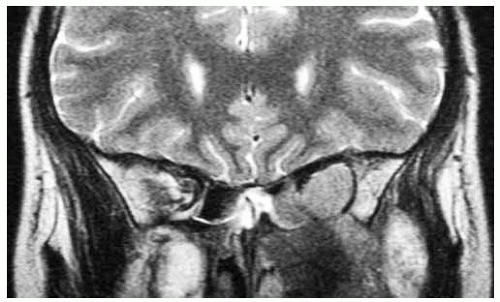
Orbital Schwannoma: Intracranial Extension
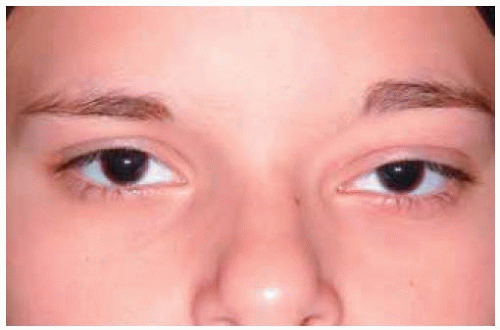
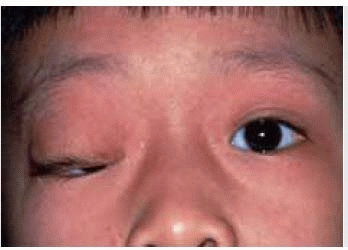
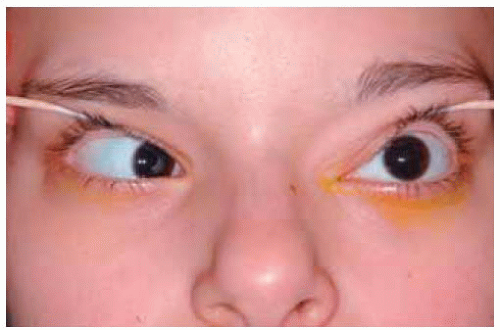 Figure 29.21. On lifting the eyelid, it was found that the left eye had complete absence of ocular motility (“frozen globe”). |
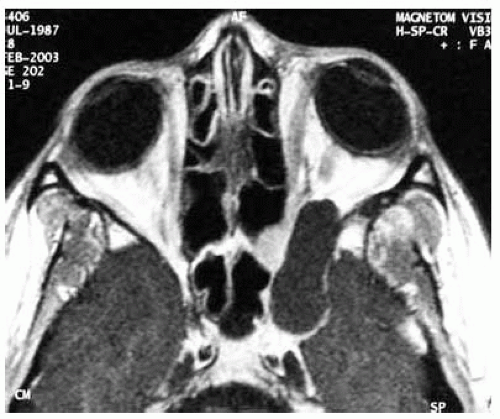
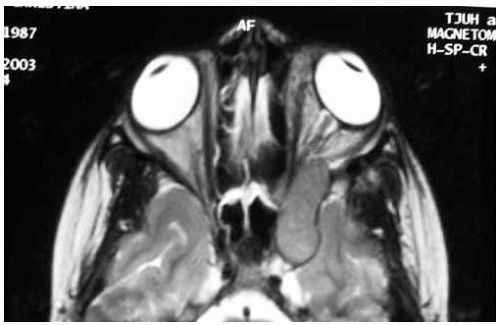 Figure 29.23. Axial magnetic resonance imaging in T2-weighted image, further delineating the well-circumscribed mass. |
Orbital Neurofibroma
General Considerations
Neurofibroma is a benign peripheral nerve tumor that can affect the orbit (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28). In the authors’ series of 1,264 consecutive space-occupying orbital lesions, the 6 neurofibromas accounted for 26% of the 23 peripheral nerve lesions and for, 1% of all lesions. It can be divided into localized, diffuse, and plexiform types (17). Among our 6 cases, there were 4 plexiform and 2 solitary neurofibromas. The localized type is clinically and radiographically similar to schwannoma and is associated with neurofibromatosis type 1 in about 10% of cases (25). The diffuse type has a variable association with neurofibromatosis and the plexiform type is almost always seen in association with neurofibromatosis.
Clinical Features
Localized neurofibroma produces clinical symptoms and signs similar to schwannoma and other circumscribed orbital tumors and can manifest as proptosis, globe displacement, diplopia, and optic nerve compression. It is usually diagnosed in middle-aged or adult patients and, as mentioned, does not occur in patients with neurofibromatosis type 1. Localized neurofibroma can sometimes occur as multiple orbital tumors in patients without clear evidence of neurofibromatosis. In such cases, pain may be a prominent symptom (27).
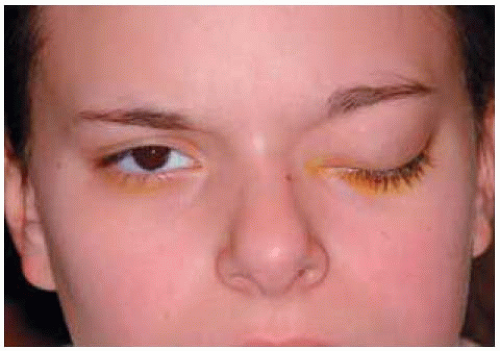
Diffuse and plexiform neurofibromas are very similar clinically and radiographically, but are classified separately because of subtle histopathologic differences (5). They generally become clinically apparent in the first decade of life and show gradual progression, often with involvement of other periocular and ocular tissues, including the uveal tract. The diffuse, poorly defined mass can cause the classic S-shaped curve to the upper eyelid owing to subcutaneous involvement by the tumor. The plexiform form can be very extensive with massive involvement of the orbit, eyelids, and intraocular structures. In addition, patients with neurofibromatosis can have congenital defects in the sphenoid bone that can produce a characteristic pulsating proptosis similar to that seen with encephalocele.
Diagnostic Approaches
With orbital computed tomography and magnetic resonance imaging, localized neurofibroma appears as a circumscribed mass that is indistinguishable from schwannoma, described previously (6). Plexiform and diffuse neurofibromas show an irregular, ill-defined mass, often with extensive periorbital involvement, as mentioned.
Pathology
Localized orbital neurofibroma is circumscribed but lacks a true capsule. The classical case shows interlacing bundles of elongated spindle cells with variable quantities of mucoid material. Diffuse and plexiform neurofibromas are composed of a complex intertwining of bundles of enlarged nerves with proliferation of Schwann cells and endoneural fibroblasts in a mucoid matrix. A distinct perineural sheath defines the individual tumor cores. The histopathologic findings of neurofibroma are discussed in more detail elsewhere (5).
Management
A patient with suspected localized orbital neurofibroma should be evaluated and managed as described for other localized orbital tumors. Clinical findings and imaging studies should be done and complete surgical excision should be considered for symptomatic lesions.
The diffuse, unresectable plexiform type should be managed more conservatively. However, surgical intervention is often necessary because of bothersome symptoms, threatened vision, or an unacceptable cosmetic appearance. In such instances, debulking surgery is often done, because complete surgical removal may not be possible. Depending on the extent of the disease, a combined approach with neurosurgeons and otolaryngologists may be prudent (19,24).
Selected References
1. Shields JA. Peripheral nerve tumors of the orbit. Neurofibroma. In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:149-152.
2. Shields JA, Bakewell B, Augsburger DG, et al. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 1984;102:1606-1611.
3. Shields JA, Bakewell B, Augsburger DG, et al. Space-occupying orbital masses in children. A review of 250 consecutive biopsies. Ophthalmology 1986;93:379-384.
4. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
5. Weiss SW, Goldblum JR. Benign tumors of peripheral nerves. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s Soft Tissue Tumors. 4th ed. St. Louis: CV Mosby; 2001:1122-1126.
6. DePotter P, Dolinskas C, Shields JA, et al. Peripheral nerve tumors. In: DePotter P, Shields JA, Shields CL, eds. MRI of the Eye and Orbit. Philadelphia: JB Lippincott; 1994:183-191
7. Tada M, Sawamura Y, Ishii N, et al. Massive plexiform neurofibroma in the orbit in a child with von Recklinghausen’s disease. Childs Nerv Syst 1998; 14:210-212.
8. Pittet B, Gumener R, Montandon D. Gigantic neurofibromatosis of the orbit. J Craniofac Surg 1997;8:497-500.
9. Gunalp I, Gunduz K, Duruk K, et al. Neurogenic tumors of the orbit. Jpn J Ophthalmol 1994;38:185-190.
10. De Potter P, Shields CL, Shields JA, et al. The CT and MRI features of an unusual case of isolated orbital neurofibroma. Ophthal Plast Reconstr Surg 1992;8:221-227.
11. Rose GE, Wright JE. Isolated peripheral nerve sheath tumours of the orbit. Eye 1991;5:668-673.
12. Kennerdell JS, Maroon JC. Use of the carbon dioxide laser in the management of orbital plexiform neurofibromas. Ophthalmic Surg 1990;2:138-140.
13. Shields JA, Shields CL, Lieb WE, et al. Multiple orbital neurofibromas unassociated with von Recklinghausen’s disease. Arch Ophthalmol 1990; 108:80-83.
14. Lyons CJ, McNab AA, Garner A, et al. Orbital malignant peripheral nerve sheath tumours. Br J Ophthalmol 1989;73:731-738.
15. Reed D, Robertson WD, Rootman J, et al. Plexiform neurofibromatosis of the orbit: CT evaluation. AJNR Am J Neuroradiol 1986;7:259-263.
16. Della Rocca RC, Roen J, Labay GR, et al. Isolated neurofibroma of the orbit. Ophthalmic Surg 1985;16:634-638.
17. Krohel GB, Rosenberg PN, Wright JE, et al. Localized orbital neurofibromas. Am J Ophthalmol 1985;100:458-464.
18. Wiesenfeld D, James PL. Pulsating exophthalmos associated with neuro-fibromatosis. J Maxillofac Surg 1984;12:11-13.
19. Jackson IT, Laws ER Jr, Martin RD. The surgical management of orbital neurofibromatosis. Plast Reconstr Surg 1983;71:751-758.
20. Woog JJ, Albert DM, Solt LC, et al. Neurofibromatosis of the eyelid and orbit. Int Ophthalmol Clin 1982;22:157-187.
21. Jackson IT. Management of craniofacial neurofibromatosis. Facial Plast Surg Clin North Am 2001;9:59-75.
22. Gurland JE, Tenner M, Hornblass A, et al. Orbital neurofibromatosis: involvement of the orbital floor. Arch Ophthalmol 1976;94 :1723-1725.
23. Lee LR, Gigantelli JW, Kincaid MC. Localized neurofibroma of the orbit: a radiographic and histopathologic study. Ophthal Plast Reconstr Surg 2000; 16:241-246.
24. Snyder BJ, Hanieh A, Trott JA, et al. Transcranial correction of orbital neurofibromatosis. Plast Reconstr Surg 1998;102:633-642.
25. Krohel GB, Rosenberg PN, Wright JE, et al. Localized orbital neurofibromas. Am J Ophthalmol 1985;100:458-464.
26. Kobrin JL, Blodi FC, Weingiest TA, et al. Ocular and orbital manifestations of neurofibromatosis. Surv Ophthalmol 1979;24:45-51.
27. Shields JA, Shields CL, Lieb WE, et al. Multiple orbital neurofibromas unassociated with von Recklinghausen’s disease. Arch Ophthalmol 1990;108:80-83.
28. Brownstein S, Little JM. Ocular neurofibromatosis. Ophthalmology 1983;91:1595-1599.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree