Options in Amblyopia
Valerie M. Kattouf
Amblyopia is the most common cause of unilateral vision impairment in patients under 40 years of age. Early detection and proper compliance are strong predictors of successful treatment. The reports of the prevalence of amblyopia in the population vary from 1% to 5% (1). These varying percentages result from the different classifications of amblyopia as well as the age at which the diagnosis is made. In the pediatric population, the incidence of amblyopia is 2% (2). This chapter reviews the proper steps to the diagnosis of functional amblyopia in infants and preschoolers as well as the most successful treatment options that address the condition. The focus of this chapter is on unilateral amblyopia.
Classifications of Amblyopia
To properly diagnose and treat amblyopia, the reduction in visual function detected must fall into the classifications discussed below.
Functional amblyopia is a unilateral (less frequently bilateral) condition in which the visual acuity is less than 20/20. No structural or pathologic anomalies exist and one or more of the following must occur prior to 6 years of age (3):
Constant unilateral strabismus
Amblyogenic anisometropia
Amblyogenic bilateral isometropia
Amblyogenic uni- or bilateral astigmatism
Image degradation
The age of onset is critical to the diagnosis of amblyopia. This definition supports the importance of early detection and treatment.
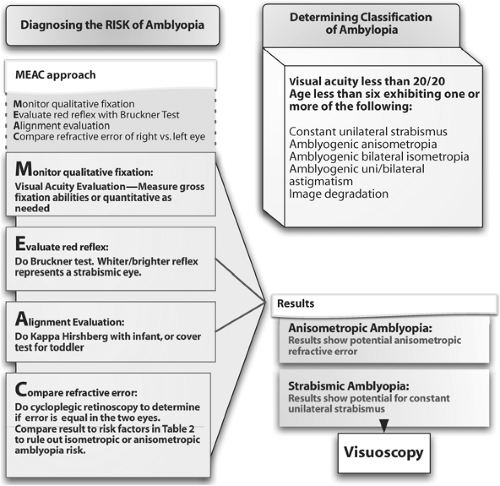
Diagnosis of Amblyopia in Preverbal children
As discussed in the visual acuity chapters (see Chapters 2 and 10), a number of methods are used to determine a quantitative visual acuity measurement in a preverbal child. Although often effective, many of these methods are unavailable to optometric practitioners in various modes of practice. The diagnosis of the risk of unilateral amblyopia is ultimately based on the presence of a potentially anisometropic refractive error or a constant unilateral strabismus. The risk for amblyopia is detected by monitoring qualitative fixation, reaction to occlusion, evaluation of the red reflex (with the Bruckner test), and refractive error of the right eye as compared with the left eye (Fig. 22.1).
Strabismic Amblyopia
Strabismic amblyopia is defined as a unilateral decrease in visual acuity occurring with a constant, unilateral strabismus that onsets before 6 years of age (3). Intermittent and alternating strabismic deviations are rarely causes of amblyopia. The strabismic deviation must be present at distance and near. Strabismic amblyopia is most commonly seen with convergent
strabismus (esotropia). Divergent strabismus is less likely to create amblyopia secondary to its intermittent nature. Patients with vertical deviations often develop anomalous head postures to afford binocularity and avoid amblyopia development (4). A high percentage of patients with constant, unilateral strabismus have amblyopia.
strabismus (esotropia). Divergent strabismus is less likely to create amblyopia secondary to its intermittent nature. Patients with vertical deviations often develop anomalous head postures to afford binocularity and avoid amblyopia development (4). A high percentage of patients with constant, unilateral strabismus have amblyopia.
The development of strabismic amblyopia is secondary to the sensory adaptations made in response to the deviation. The initial deviation of the visual axis in the strabismic eye leads to diplopia and visual confusion. The strabismic deviation then causes the stimulation of noncorresponding retinal points, producing a diplopic image. In addition, a strabismic deviation causes the fovea of the deviated and nondeviated eyes to be directed at two different images, resulting in visual confusion (5). Dipolpia and confusion are important concepts in the development of strabismic amblyopia. To avoid diplopia and confusion, the visual system suppresses the strabismic eye. The inhibition of the deviated eye results in cortical spatial changes and a secondary decrease in visual acuity, resulting in amblyopia. Understanding the mechanism causing the development of strabismic amblyopia aids in determining the appropriate treatment modality for each patient.
The Importance of Eccentric Fixation in Strabismic Amblyopia
Eccentric or monocular fixation is a condition that exists only in amblyopic patients. It is most common in strabismic amblyopia and rare in anisometropic amblyopia. It occurs when the amblyopic eye actively attempts to fixate with an off-foveal point under monocular
conditions (6). Eccentric fixation affects visual acuity, therefore it is important to be aware of it clinically. Testing for eccentric fixation can be completed successfully in a cooperative preschool patient. It is rarely (if ever) tested for in an infant, but should be evaluated as the amblyopic patient matures.
conditions (6). Eccentric fixation affects visual acuity, therefore it is important to be aware of it clinically. Testing for eccentric fixation can be completed successfully in a cooperative preschool patient. It is rarely (if ever) tested for in an infant, but should be evaluated as the amblyopic patient matures.
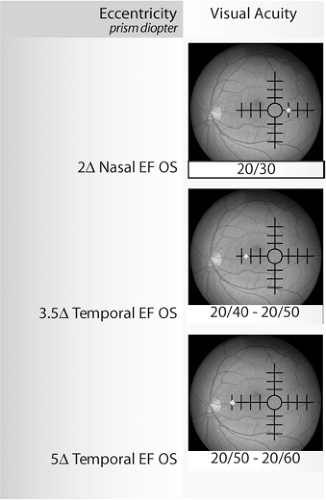
Table 22.1 Visual Acuity Findings in Relation to Retinal Eccentricity. | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
The fovea is the area of the retina with the highest cone density and largest cortical representation. In the amblyopic patient, the fovea remains the area of the retina with the highest visual resolution. Even in amblyopic patients, the best achievable visual acuity is at the fovea. Eccentric fixation with a nonfoveal point leads to a linear decrease in acuity the further fixation is from the fovea (7) (Table 22.1). The maximal magnitude of eccentric fixation observed clinically is 3 to 4 prism diopters from the fovea. Most esotropic patients exhibit nasal eccentric fixation and those who are exotropic exhibit temporal eccentric fixation. The cause of eccentric fixation is not completely known.
A Clinical Tool to Diagnose Eccentric Fixation
Visuoscopy is the most common clinical tool used to assess eccentric fixation (EF) in an amblyopic patient. The grid target on a direct ophthalmoscope is used to determine the presence of eccentric fixation, as well as its magnitude and direction. This procedure is most efficient when done with a dilated pupil (but can be performed on an undilated pupil). Visuoscopy must be done with the patient’s eye not being tested occluded because eccentric fixation is a monocular condition.
In order to perform visuoscopy focus the grid target of the ophthalmoscope on the retina of the amblyopic eye while asking the patient to view the center of the “bull’s eye” target. Central fixation reveals the foveal reflex directly in the center of the grid. Eccentric fixation is represented by the foveal reflex located outside the center of the grid (Fig. 22.2). The examiner must identify the retinal location the patient is using to fixate. The direction of eccentric fixation is represented by where the grid lies in respect to the foveal reflex. Each mark on most ophthalmoscope target represents 1 prism diopter of eccentric fixation (8). In addition to determining the magnitude and direction of eccentric fixation, steadiness must also be addressed. Because of poor fixation abilities, most amblyopic patients demonstrate unsteady fixation. The steadiness of monocular fixation can also be evaluated with the visuoscopy technique. No matter what the location of monocular fixation, central or eccentric, the examiner must look for drifting away from the fixation point with saccadic movements to recover the fixation point (9).
Relevance of Eccentric Fixation Detection
The detection of eccentric fixation in strabismic amblyopia is crucial in determining the patient’s prognosis and treatment plan. The presence of EF does not allow the practitioner to predict an outcome of 20/20 visual acuity in the patient with strabismic amblyopia. The information provided in Table 22.1 aids in predicting the best achievable visual acuity with full refractive error correction and occlusion treatment alone. It is not the scope of this chapter to discuss the treatment of eccentric fixation.
Eccentric Fixation
A 4-year-old boy diagnosed with a 20Δ constant, left esotropia.
No significant refractive error.
Visual acuity OD 20/20, OS 20/200.
Visuoscopy reveals central fixation OD, 3Δ nasal eccentric fixation OS.
Occlusion therapy will be initiated.
The best visual acuity predicted to parents with proper compliance will be approximately 20/40 to 20/50.
Anisometropic Amblyopia
Anisometropic amblyopia is a unilateral decrease in visual acuity occurring with unequal, uncorrected refractive error that is present before 6 years of age (3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree