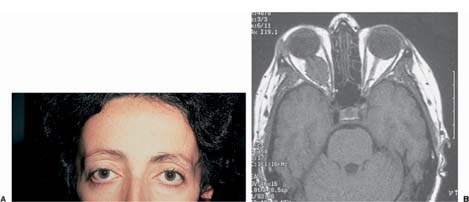
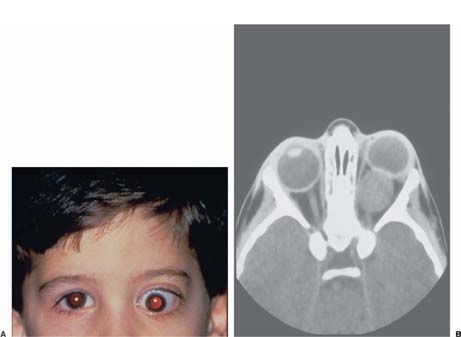
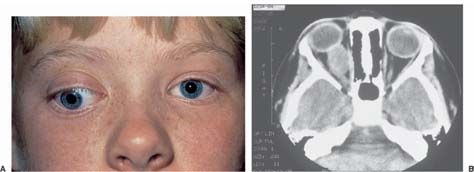
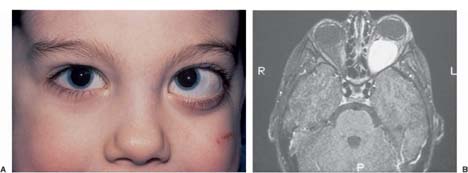
Chapter 27 Tumors of the optic nerve produce damage by infiltrating or compressing nerve tissue and sometimes by both mechanisms.1,2 Many of these lesions are primary tumors of the nerve, such as optic gliomas and meningiomas, but some are secondary, such as carcinomas and lymphoma. A patient with a known or presumed optic nerve tumor who has indolent stable or slowly progressive visual loss (see below) requires an imaging study within 1 or 2 weeks. Patients with acute, stable loss of vision or visual loss that is rapidly progressive require an imaging study within 24 hours. Optic nerve tumors occur in all age groups. Optic nerve gliomas are most common in children,3,4 whereas meningiomas are most common in middle-aged adults.5,6 Metastatic carcinoma occurs most often in middle-aged and older adults,7 whereas metastatic lymphoma occurs in elderly patients and in patients of all ages who are immunosuppressed by drugs or disease.8 Optic nerve tumors occur in both sexes. The frequency with which the sexes are affected depends on the tumor. Optic nerve gliomas occur equally in both sexes3,4 whereas optic nerve sheath meningiomas occur more often in women than in men.5,6 Metastatic breast carcinoma is, as might be expected, much more common in women than in men, whereas metastatic prostate cancer is found exclusively in men. Metastatic lung and bowel carcinoma occur with equal frequency in men and women, as does metastatic lymphoma.9 Visual loss may occur suddenly, or it may develop insidiously and progress slowly over several months. Metastatic cancers usually produce relatively sudden loss of vision over several minutes to days,9 whereas optic nerve sheath meningiomas usually cause slowly progressive loss of vision over months to years.5,10 Optic nerve gliomas also may cause slowly progressive visual loss or be entirely asymptomatic.3,4 Transient monocular visual loss can occur in patients with optic nerve tumors, most often meningiomas.5,10 The visual loss usually occurs only in certain positions of gaze, and vision immediately clears when the direction of gaze is changed.10 It is assumed that either direct pressure on the optic nerve or interruption of blood supply is responsible for this phenomenon.11–13 Depending on their size and location, optic nerve tumors may produce double vision by limiting movement of the affected eye. The diplopia may be horizontal, vertical, or oblique. Pain is not a common symptom in patients with optic nerve tumors, unless the tumor is also affecting the trigeminal nerve. Visual acuity may be reduced substantially, or it may be completely normal. Some patients who complain of reduced vision have visual acuity of 20/20; however, the other eye has vision of 20/15 or better, and many of these patients have other evidence of optic nerve dysfunction, including deficits in color vision, visual field defects, and a relative afferent pupillary defect (see below). Patients who have reduced visual acuity from an optic nerve tumor usually have a deficit in color vision when tested with color plates or when asked to compare the appearance of a red test object with each eye. In addition, patients with normal or near-normal visual acuity may have difficulties with color perception that are not present in the opposite eye. Like visual acuity, the visual field is variably affected by optic nerve tumors. There is no specific field defect that identifies a patient as having an optic nerve tumor. Altitudinal, arcuate, central, and even cecocentral defects may occur, as may generalized or localized reduction in sensitivity in the central field and depression of the peripheral field.3,5,12 Patients with an optic nerve tumor almost always have a relative afferent pupillary defect, unless the tumor is affecting both optic nerves equally. Proptosis may occur in patients with optic nerve tumors, particularly those that surround and compress the nerve, such as optic nerve sheath meningiomas (Fig. 27–1). Optic nerve gliomas may also produce proptosis, particularly when the bulk of the lesion is within the orbit (Fig. 27–2). Metastatic tumors usually do not produce proptosis unless they infiltrate the orbital fat or extraocular muscles. Optic nerve tumors may be associated with strabismus. The strabismus usually results from the mass effect of the tumor on the extraocular muscles rather than from damage to one or more of the ocular motor nerves (Fig. 27–3). In children, loss of vision may result in a sensory strabismus (Fig. 27–4). Tumors that compress or infiltrate the proximal portion of the optic nerve typically produce optic disc swelling. The swelling may be mild or severe, but even when it is severe, there are rarely hemorrhages or exudates present (Fig. 27–5). Tumors that compress or infiltrate the optic nerve in the orbital apex, in the optic canal, or intracranially typically do not cause swelling of the optic disc. In these settings, the optic disc initially appears normal despite other evidence (decreased visual acuity, color vision deficits, visual field defect, relative afferent pupillary defect). Eventually, the optic disc becomes pale. Some patients with optic nerve tumors, most often optic nerve sheath meningiomas, develop one or more dilated, corkscrew vessels that overlie the optic disc and peripapillary region (Fig. 27–6). These retinochoroidal collaterals, which are also called opticociliary shunt veins by some authors, shunt venous blood from the retinal veins to the choroidal venous circulation.5,12,14 When caused by a tumor of the optic nerve, retinochoroidal collaterals generally are associated with reduced visual acuity and optic disc swelling or atrophy.12,14 The common denominator in these cases is prolonged compression of the optic nerve with gradual compression and obstruction of the central retinal vein. The retinal venous blood flow is shunted to the choroid, allowing it to leave the eye via the vortex veins to the cavernous sinus, but this previously existing system becomes dilated, resulting in the visible corkscrew vessels. The triad of visual loss, optic atrophy, and retinochoroidal collaterals occurs most frequently in patients with spheno-orbital meningiomas, but it also occurs in patients with optic nerve gliomas, chronic papilledema, craniopharyngioma, sarcoidosis, and other rare causes of optic nerve compression. FIGURE 27–1 Proptosis from optic nerve sheath meningioma. A: Appearance of a 35-year-old woman with slowly progressive loss of vision in right eye. Note mild, right axial proptosis. B: T1-weighted, axial magnetic resonance image shows mass surrounding the orbital portion of the optic nerve. The appearance of the lesion was thought to be most consistent with an optic nerve sheath meningioma. FIGURE 27–2 Proptosis from an optic nerve glioma. A: Appearance of a 5-year-old boy with progressive visual loss and protrusion of the left eye. Note marked left proptosis and infradisplacement of left eye. B: Axial computed tomographic scan shows large intrinsic tumor of left optic nerve. Surgery confirmed an optic nerve glioma. FIGURE 27–3 Strabismus in a child with an optic nerve glioma. A: Appearance of a 6-year-old girl with progressive loss of vision in the right eye. Note right exotropia and hypotropia. B: Axial computed tomographic scan shows intrinsic tumor of right optic nerve. Surgery confirmed an optic nerve glioma, which was displacing the globe outward and downward. FIGURE 27–4 Strabismus in a child with an optic nerve glioma. A: Appearance of a 4-year-old boy with progressive loss of vision in the left eye. Note left esotropia and hypertropia. B: Magnetic resonance image scan shows large intrinsic tumor of left optic nerve. Surgery confirmed an optic nerve glioma. It was thought that the strabismus was secondary to loss of vision rather than to the mass effect of the tumor.
OPTIC NERVE TUMORS
URGENCY OF EVALUATION
DIAGNOSIS
SYMPTOMS
Demographics
Visual Loss
Gaze-Evoked Amaurosis
Double Vision
Pain
SIGNS
Visual Acuity
Color Vision
Visual Field
Pupils
Proptosis
Strabismus
Optic Disc
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree