Gradual Loss of Vision
In evaluating reduced vision in pathologic terms, best-corrected visual acuity must first be achieved to eliminate the physiologic abnormalities. The three most common causes of gradual loss of vision are cataract, senile macular degeneration, and glaucoma.
Cataract formation, the loss of transparency of the crystalline lens, is common. Increased density of the lens fibers
and changes in protein content occur, almost without exception, to some degree in every person with increasing age; however, the loss of transparency can be so marked that visual function is seriously hampered. The term
cataract usually is reserved for the latter situation. Cataract formation usually is evolutional, but it occasionally has a specific cause, such as galactosemia, galactokinase deficiency, diabetic ketoacidosis, postradiation therapy, or trauma. If a metabolic abnormality can be corrected early in the course of cataract formation, some lens opacity can be reversed; however, there is no known reversal of lens changes due to senile cataract. Treatment is surgical removal of the cataract. The need for surgery usually depends on the patient’s visual requirements and desires. In rare instances, the cataract damages the eye because of high pressure from rapid swelling and may have to be removed for other than optical reasons.
The operation usually is performed by means of opening the anterior capsule and extracting the lens material. The posterior capsule is left intact and the lens substance removed by phacoemulsification. After a person is aphakic, the optical power of the lens must be replaced to provide focusing ability. The patient can be fitted with spectacles or contact lenses after the eye has healed, but usually, a polymer intraocular lens is implanted during the surgical procedure, with the appropriate lens strength being determined preoperatively. It is comforting to inform patients that cataract surgery is one of the most successful operations performed.
A second important cause of gradual progressive decrease in vision among older persons is senile macular degeneration. The cause of this condition is unknown, but it may be related to a decrease in the blood supply to the macular area associated with hardening of the arteries in the posterior eye, which begins as a pigmentary disturbance in the macula and usually progresses slowly but steadily with increased scarring and often hemorrhage into the tissues. The disease is bilateral but usually asymmetrical. No effective treatment exists, and normal use of the eyes, as for sewing and reading, does not accelerate the process. Patients should be assured that macular degeneration is not a blinding disease because the peripheral vision is not disturbed. Patients with this condition always are able to move around unaided, even though their useful reading vision may be markedly decreased.
Unlike the two aforementioned visually disabling conditions, glaucoma characteristically produces a decrease in peripheral visual ability, but good reading vision is maintained until late in the disease. Mild glaucoma can normally be controlled with daily topical eye drops.
Sudden Loss of Vision
Sudden loss of vision is a dramatic event and usually is caused by an identifiable pathologic process. Some processes can be treated and controlled to allow restoration of vision, while others produce permanent loss of visual function. Vitreous hemorrhage unrelated to trauma can occur in advanced diabetes mellitus as a result of disease of the retinal blood vessels. The vitreous “haze” prevents complete examination of the retinal blood vessels, and the offending area often remains unidentified until the blood is reabsorbed. It can take months or years for the vitreous to clear in a relatively young person, producing marked disability, while it may never clear in an older person.
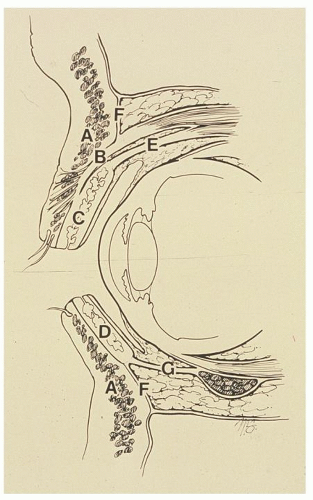
Central retinal arterial occlusion causes total and permanent loss of vision and abolishment of the direct pupillary reaction to light. On ophthalmoscopic examination, the fundus will appear pale with development of a cherryred spot in the macula. The spot is caused by continued choroidal blood supply to the macula with the contrasting loss of circulation to the rest of the retina. The retinal arteries are narrow and may have fragmented blood columns (“boxcar sign”). The cause usually is an embolus from diseased carotid arteries, abnormal heart valves, or thrombosis from long-standing atherosclerosis. In rare instances, central retinal arterial occlusion is a vasospastic event associated with an inflammatory disease. Treatment aimed at relieving the obstruction through drug-induced vasodilation, ocular massage, and inhalation of 5% carbon dioxide and 95% oxygen usually is unsuccessful. Attacks of
amaurosis fugax and central or branch retinal artery occlusion have been shown to be related to internal carotid artery stenosis (
3). An increase in ulcerated free plaque surfaces appears, which might lead to arterial embolization. Duplex ultrasonography and continuous-wave Doppler ultrasonography can be used for obtaining a noninvasive diagnosis; however, magnetic resonance angiography (MRA) is rapidly gaining favor as a sensitive screening test for carotid stenosis.
Central retinal venous occlusion is more common and less dramatic than arterial occlusion, and it has a markedly better prognosis. On ophthalmoscopic examination, the fundus has a dramatic appearance, as if the entire view has been splattered with blood, and the observed vessels appear engorged and tortuous. Much of the hemorrhage clears with time, vision returns, and late complications of retinal anoxia are managed by the ophthalmologist.
Retinal detachment is not a rare occurrence. It is much more common among persons with high myopia (those with long eyeballs), after cataract surgery (˜1 in 100), and following facial trauma. The mode of visual loss varies. The patient commonly reports a shadow or curtain in front of the eye, ascending or descending, depending on the direction of the spreading separation of the retina. Associated flashing lights and floaters may be seen as the retinal structure is disturbed. If the macula becomes detached, central vision is abruptly lost. At ophthalmoscopy, the detached retina is found to be pale and wrinkled and to project forward into the vitreous, often to the point at which objects viewed cannot be focused by the lens onto the retina. Surgical reattachment of the retina is successful in 60% to 80% of cases, but return of vision depends on early
diagnosis, length of time detached, and avoidance of late surgical complications.
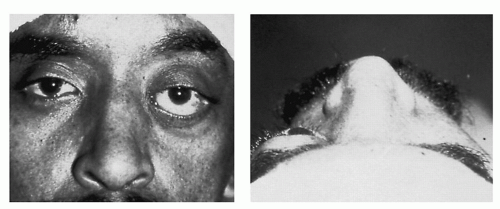
Optic nerve compromise, whether in the form of ischemia or inflammation, is not as common as retinal detachment, but it is equally dramatic and important. A patient older than 55 years who has sudden loss of vision and perhaps has vague arthritic symptoms, low-grade fever, or temporal scalp tenderness should have the erythrocyte sedimentation rate (ESR) measured. If the ESR is elevated, the diagnosis is most likely
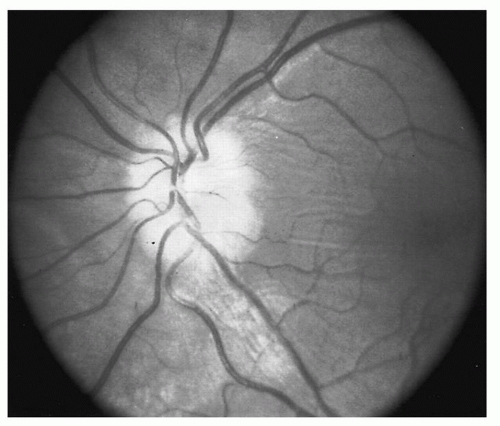
temporal arteritis, with the opposite eye being at risk for parallel visual loss. Systemic steroid therapy should be initiated early to prevent the onset of inflammation in the other eye. For a younger person, if loss of vision is associated with edema of the optic disk, the diagnosis is likely
optic neuritis (
Fig. 14.4). The prognosis for return of vision is good, but the possibility that a demyelinating disorder, such as multiple sclerosis, is present must be strongly considered.
Sometimes, the report of sudden loss of vision is unfounded. This usually occurs when an older patient suddenly “discovers” a loss of sight that has existed for some time. Chance occlusion of the seeing eye reveals the visual loss, which is erroneously reported as being acute. The report of sudden loss of vision also can be associated with hysteria or malingering and the desire for secondary gain. This is especially true in young adolescents.
Transient Loss of Vision
Transient loss of vision can be part of the aura of migraine or a consequence of chronic papilledema. Visual blackouts are common in vertebral-basilar insufficiency after at least 80% narrowing of this vascular system from atherosclerosis. These blackouts are ominous because repeated attacks often are not transient and can be permanent. Abnormalities in the carotid system can cause temporary, usually unilateral, loss of vision (amaurosis fugax). Associated cerebral symptoms and hemiparesis may be noted. Because 15% to 20% of these patients later have a stroke, they need a complete vascular evaluation.
Diplopia
Diplopia is another symptom of visual abnormality. Physiologic diplopia is a normal phenomenon in which objects not within the area of fixation are seen as double. This is easily seen when one looks at a near object with attention directed at a distant object, which then appears double. Usually, this is not in one’s conscious awareness. Diplopia can either be monocular or binocular, and this must be determined initially through eye cover testing (
4). Pathologic diplopia is a cardinal sign of weakness of one or more of the extraocular muscles and usually is caused by neurologic disease, trauma, or diabetes mellitus. Diplopia also can occur with normal muscle function if the globe is displaced, as in slowly progressive e orbital disease or tumors that prevent proper alignment of visual stimuli. Monocular diplopia (that which does not go away when one eye is covered) is rare and usually due to splitting of light rays by an irregularity in the cornea, certain types of cataracts, or misaligned photoreceptors in the macula. More commonly, monocular diplopia is a neurotic or functional disorder.