Odontogenic Infections
Timothy D. Doerr
Odontogenic infections are common infections primarily treated by dental professionals. These infections are usually associated with dental caries or periodontal disease and are seen more often in underserved populations where regular dental care is lacking. In most cases, odontogenic infections are successfully treated in the early stages by the dental professional with a minor dental procedure and oral antibiotics. The initial treatment commonly consists of drainage of infectious tissue with extraction or endodontic treatment of the diseased tooth.
In some cases, the infection will spread from the dental alveolar structures into the adjacent soft tissue spaces. This can lead to serious infections of the fascial spaces of the face and neck. When these infections are not promptly managed, serious, even life-threatening complications can arise. It is often in the setting of an advanced odontogenic infection that the otolaryngologist first becomes involved. Patients will have local anatomy that can be distorted by infection and are at risk for airway obstruction. The otolaryngologist needs an understanding of the progression of odontogenic infections to properly treat these patients.
This chapter focuses on the microbiology, pathways of spread, and appropriate management of odontogenic infections. This knowledge will allow the surgeon to successfully treat these infections and help prevent major complications. The chapter also highlights the importance of the dental anatomy and fascial spaces in predicting and treating the spread of an odontogenic infection.
DEMOGRAPHICS
The incidence of an odontogenic infection will vary with the population studied. Those individuals with poor dental hygiene and those who are immunosuppressed are most susceptible. The peak incidence of odontogenic infections is in the third and fourth decades with a larger percentage of the complicated infections occurring in diabetic patients (1,2,3,4). There is nearly equal distribution between male and female patients although this has varied in some studies (2,3,5).
MICROBIOLOGY
Normal flora in the oral cavity contains over 1,000,000 organisms per cubic centimeter of which 10% are aerobic cocci and 90% anaerobic bacteria. The bacterial flora varies among the different oral cavity sites and with the health of the individual. The flora is also influenced by patient age, immune status, diet, environment, and host factors (6). Streptococci are the most common aerobic bacteria found in the oral cavity with the viridans species most prevalent. Staph is relatively infrequent in the oral cavity but becomes more prevalent in the setting of a mixed flora infection. Anaerobes increase in number in the setting of chronic infections like periodontitis (7).
An odontogenic infection is primarily caused by bacteria that colonize the mouth. These bacteria, when given the appropriate circumstances, can become pathogens. As a general rule, odontogenic infections are polymicrobial with a large percentage being primarily anaerobic infections (6,8).
Prior studies have shown that approximately one quarter of the infections were caused by aerobic or facultative anaerobic bacteria while about three-fourths were caused by strict anaerobes (9). Studies have also shown that when anaerobes predominate, the clinical infection is more severe. Based on these published culture data, appropriate empiric antibiotic therapy for odontogenic infections requires antimicrobial agents able to treat streptococcus and oral anaerobes species.
SPREAD OF LOCALIZED INFECTIONS
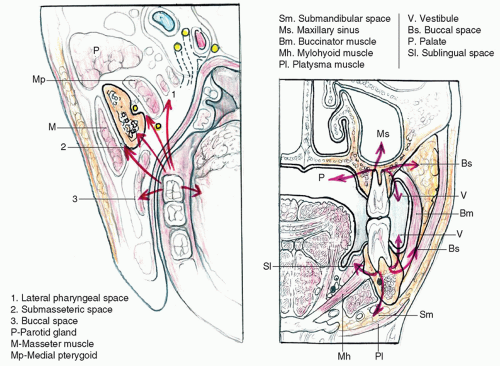
Most odontogenic infections begin with necrosis in the dental pulp from deep caries. Pulp necrosis is then followed by the spread of bacteria through the pulp chamber into the adjacent bone and soft tissues (Fig. 53.1).
Infected teeth are usually tender to percussion and may show a diminished or absent response to electrical tooth vitality testing. With the initial onset of pain, there may be no changes seen on the initial radiograph, but later periapical bony changes can be seen. With a chronic infection, a periapical cyst will be visible on imaging. Typically, treatment during this initial period with either endodontic treatment or extraction should alleviate the tooth pain and can also effectively drain the infection.
It is important to recognize that the initial steps in the development of a severe odontogenic infection may progress very slowly. It may take several months and even years for an infection from dental decay to reach the dental pulp and produce pulp necrosis and periapical abscess. The vast majority of patients will have had several signs and symptoms alerting them to an impending infection. In fact, 100% of patients experienced pain before presentation. In many cases, that pain was intermittent, but the patient did not seek a dental evaluation until severe pain or acute swelling with trismus ensued (10).
Once the infection is in the bone, it will usually follow a path of least resistance until reaching a plate of cortical bone. An infection can remain contained in the medullary bone space or erode through the cortical bone into the soft tissues (Fig. 53.2).
If the infection involves the adjacent soft tissue, it can cause a diffuse inflammatory response with cellulitis or form an abscess. A walled-off abscess in the labial or buccal gingiva is termed a parulis while an infection extending into the alveolar mucosa forms a vestibular space abscess.
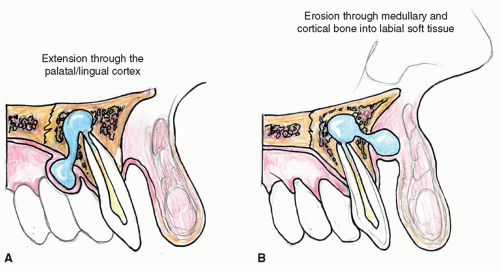 Figure 53.1 Spread of infection from an infected tooth root through the palatal/lingual cortex (A) and labial/buccal cortex (B). |
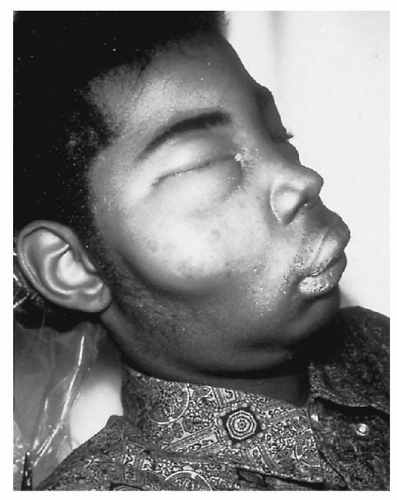
The direction of spread of odontogenic infection is in part predicted by the location of the diseased tooth. Maxillary tooth roots are in closer proximity to the labial and buccal bone plates. The root position combined with the thick alveolar bone in the hard palate usually results in extension of infection to the labial or buccal side. This direction of spread produces swelling of the upper lip (Fig. 53.3).
On the rare occasions when an infection travels medially (lingually), a tender unilateral mass can form on the palate. By comparison, the mandibular tooth roots are closer to the lingual cortex posteriorly, and infections of these teeth can spread through the thinner plate of bone into the floor of the mouth. Despite this anatomic relationship, the vast majority of mandibular tooth infections (both anterior and posterior) will also spread through the buccal cortex.
As a rule, an odontogenic infection produces pain when the necrotic pupal contents are under pressure and also when the soft tissues and periosteum over the cortical bone are distended. The pain associated with a localized infection can decrease significantly as the tissue pressure drops when infection spreads through the bone and periosteum into the soft tissues. The position and root anatomy of an infected tooth are generally predictive of the location of the associated dentoalveolar abscess (Table 53.1).
The treatment of a dental infection at this stage involves a thorough drainage of the infected soft tissues combined with extraction of the offending tooth and administration of systemic antibiotics (Fig. 53.4).
SPREAD OF LOCALIZED INFECTIONS
When the infection of a diseased tooth spreads more deeply into the soft tissue instead of exiting superficially through an oral or cutaneous path, the spread is greatly influenced by the tooth position and the adjacent fascia
attachments. Maxillary and mandibular teeth thus have distinctly different patterns of spread based on these anatomic relationships.
attachments. Maxillary and mandibular teeth thus have distinctly different patterns of spread based on these anatomic relationships.
In general, dental infections of the anterior maxilla will spread superiorly into potential spaces bounded by the mimetic muscles. Maxillary tooth infections occasionally can also spread via the dental roots into the maxillary sinus. The masticator spaces are in close proximity to the roots of the maxillary molars, and they may be involved directly by odontogenic infections from these teeth. Once an infection reaches the masticator and cervicofacial spaces, it can spread into the deeper parapharyngeal space.
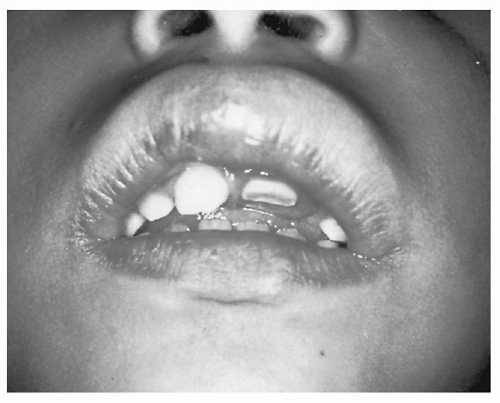 Figure 53.3 Lip cellulitis in a child secondary to a fractured maxillary incisor tooth with pulpal exposure. |
TABLE 53.1 PRESENTATION AND LOCATION OF DENTAL ABSCESSES | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
CANINE SPACE INFECTIONS
The canine space represents a potential space bounded by the muscle heads of the upper lip levators. These lip elevator muscles originate high on the maxilla and insert at the upper lip at the angle of the mouth. Although this space is infrequently involved with dental infections, it becomes involved if an infection from a maxillary cuspid tooth perforates the lateral cortex superior to the attachment of those upper lip elevators. Such an infection usually produces a firm swelling of the medial cheek and lateral surface of the nose that blunts the nasal labial crease. Rarely, this infection can spread from canine space through the valveless facial veins to involve the orbit. Most canine space infections are successfully treated by drainage with an intraoral incision placed high in the maxillary vestibule combined with extraction or root canal therapy of the diseased tooth.
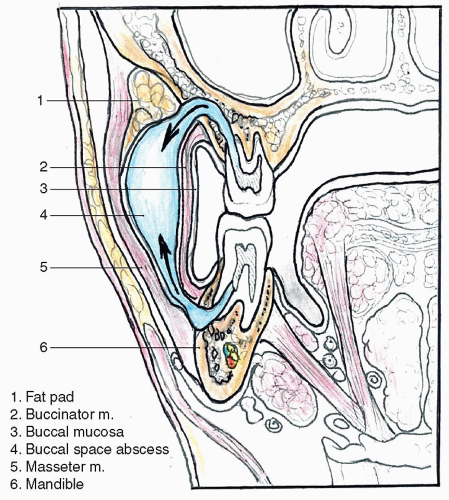
BUCCAL SPACE INFECTIONS
The buccal space is located between the buccal muscle and buccopharyngeal fascia medially and the cheek skin laterally. Its anterior limit is the lip, and its posterior boundary is the pterygomandibular raphe. Superiorly the space is bounded by the zygomatic arch, and inferiorly it extends to the lower aspect of the mandible. As noted previously, infections from mandible and maxillary bicuspids and molars tend to drain in a lateral direction through the buccal cortex. Infection perforating the bone above the attachment of the buccinator muscle on the maxilla or below the attachments of the buccinator muscle on the mandible leads to a buccal space infection or abscess (Fig. 53.5).
Clinically, a buccal space infection produces tender swelling of the cheek that can extend to the mid upper lip. Here the space is limited by orbicularis oris muscle fibers at the philtrum. The buccal space extends posteriorly over the ramus of the mandible and to the border of the parotid. Superior spread of a buccal infection leads to swelling of the soft tissues of the orbit that “closes the eye” (Fig. 53.6).
Usually a buccal infection will be superficial to the orbital septum and not involve the orbital contents. However, the swollen eye needs to be carefully examined to ensure that the infection has remained preseptal and does not put the vision at risk. An infection that becomes postseptal will involve the orbital contents including the extraocular muscle and may extend to the orbital apex and cavernous sinus.
Because of its lax lateral soft tissue boundary, the buccal space has an ability to expand to a surprisingly large volume with purulent secretions. Despite the impressive swelling, a patient may not have much trismus. Although these buccal infections may be approached intraorally, most advocate draining these infection pockets through well-placed skin incisions. Incisions placed at the angle of the mandible allow complete drainage of the space and are cosmetically acceptable. The space should be opened with careful blunt spreading to avoid injuring branches of the facial nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree