Fig. 14.1
External photograph of sarcoid granuloma on the face
In children, sarcoidosis usually manifests as a triad of rash, uveitis, and arthritis in children less than 4 years of age. In older children, it could be associated with generalized lymphadenopathy and eyes, skin, liver, and lung involvement. In the developing world where tuberculosis is endemic, the occurrence of generalized lymphadenopathy is usually mistaken for tuberculosis and many of the children are on antitubercular therapy. Childhood sarcoidosis may also be misdiagnosed as juvenile chronic arthritis [2].
Ocular Sarcoidosis
Patients may be asymptomatic or present with blurred vision, floaters, redness, or discomfort. Ocular involvement is usually a chronic disease and has an insidious onset. It can involve the lacrimal glands, orbit, eyelids, conjunctiva, uveal tract, and optic nerve (Figs. 14.2, 14.3, 14.4, 14.5, 14.6, 14.7, 14.8, 14.9, 14.10, and 14.11). The ocular findings in sarcoidosis are summarized in Table 14.1 [2, 4–9, 14–20].
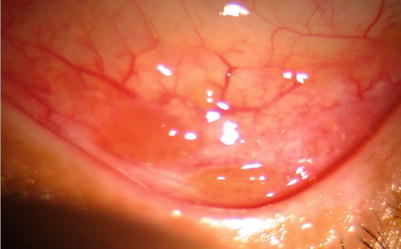
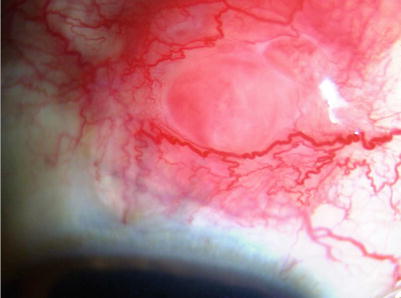
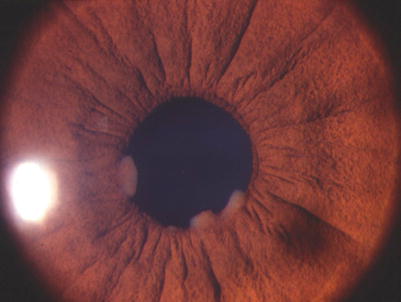
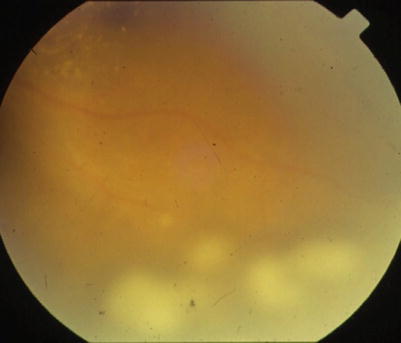
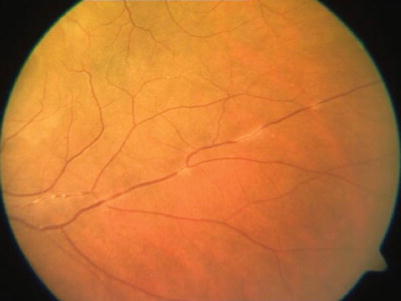
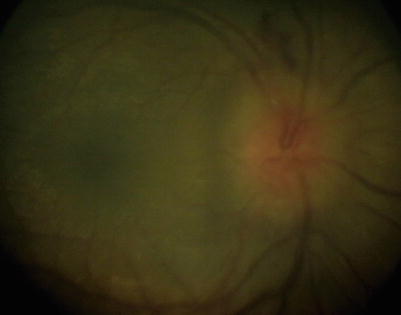
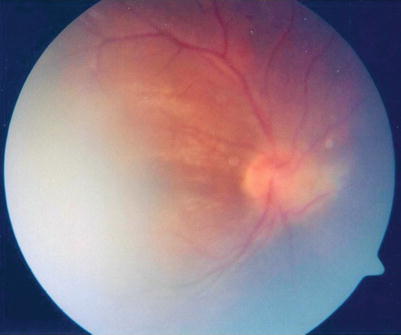
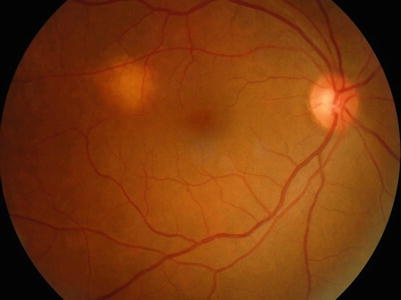
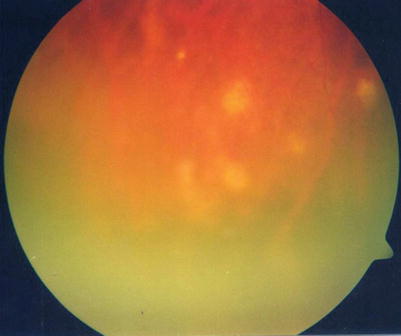

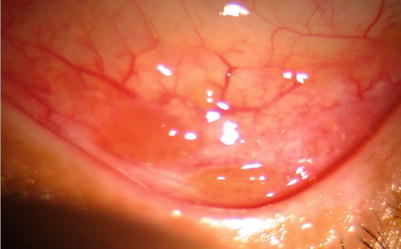
Fig. 14.2
Slit-lamp photograph showing the conjunctival granulomas in a patient with thoracic sarcoid
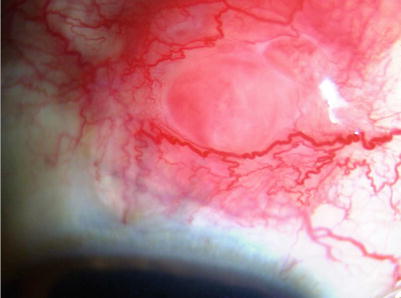
Fig. 14.3
Slit-lamp photograph showing the scleral nodule in a patient with sarcoidosis
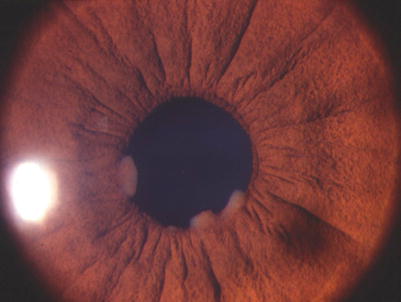
Fig. 14.4
Slit-lamp photograph showing the granulomatous anterior uveitis with large koeppe nodules
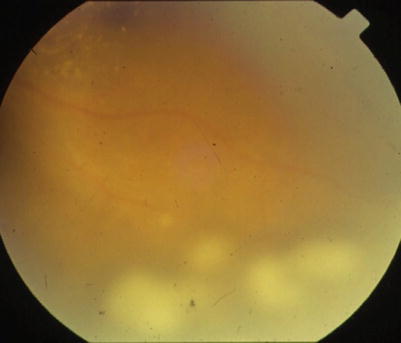
Fig. 14.5
Fundus photograph showing vitritis with snowball opacities in the peripheral retina
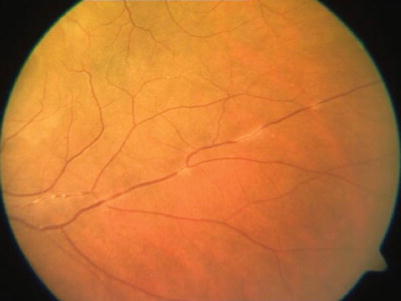
Fig. 14.6
Fundus photograph showing the perivasculitis
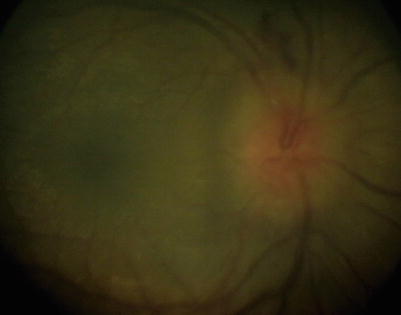
Fig. 14.7
Fundus photograph showing the disk edema
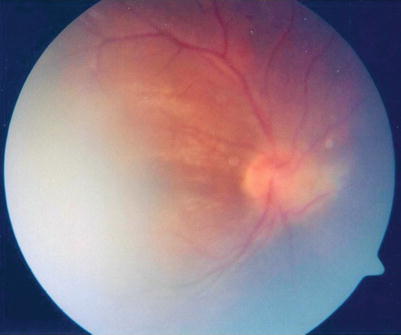
Fig. 14.8
Fundus photograph showing the optic nerve granuloma
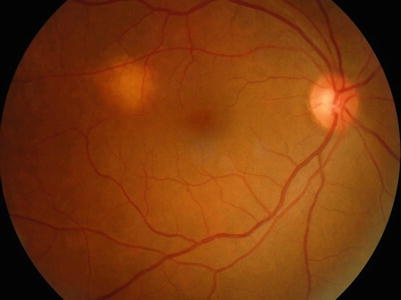
Fig. 14.9
Fundus photograph showing the choroidal granuloma
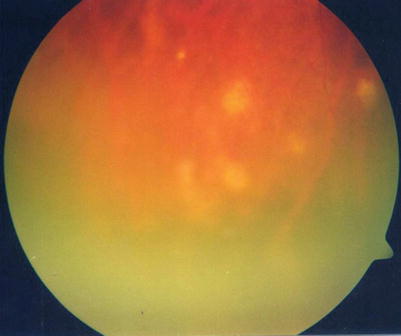
Fig. 14.10
Fundus photograph showing the peripheral chorioretinal punched-out scars in a patient with sarcoidosis

Fig. 14.11
Fundus photograph showing the optic nerve head anastomosis in a patient with cutaneous sarcoidosis
Table 14.1
Ocular findings in sarcoidosis
Bilaterality |
Eye lid and conjunctival granulomas |
Lacrimal gland involvement |
Keratoconjunctivitis sicca |
Nongranulomatous anterior uveitis |
Mutton fat keratic precipitates |
Iris and pupillary nodules/iris mass |
Increase in IOP |
Tent shaped PAS |
Nodules in trabecular meshwork |
Intermediate uveitis |
Snowballs/strings of pearls vitreous opacities |
Multifocal peripheral chorioretinal lesions (active and atrophic) |
Nodular and/or segmental periphlebitis (with or without candle wax exudate) |
Retinal macroaneurysm |
Choroidal granuloma |
Hemorrhagic retinopathy with branch or central retinal venous occlusions |
Acute posterior multifocal placoid pigment epitheliopathy and retinal pigment epithelial detachments |
Optic disk nodules/granuloma/optociliary shunts/dilated collateral veins on the optic nerve head |
Neurological manifestations: cranial nerve palsies, encephalopathy, chiasmal syndromes, motility disorders, disorders of the hypothalamus and pituitary gland, optic atrophy either due to direct sarcoid tissue infiltration, or compression by cerebral mass |
Lacrimal Gland and Orbits
Lacrimal gland involvement is common and may present as a dry eye. Severe keratoconjunctivitis sicca is not uncommon. Reports of sarcoid-induced myositis have been reported. Sarcoidosis coexisting with Grave’s disease has been reported.
Eyelids and Conjunctiva
Conjunctival granulomas are millet-shaped to large cream to brown nodular lesions, which can occur in sarcoidosis. They are usually asymptomatic. However large conjunctival granulomas can cause diplopia. They respond generally to topical steroids. Eyelid granulomas are also seen in sarcoidosis. Long-standing uveitis may lead to corneal band degeneration especially in children.
Uveitis
It is typically a chronic bilateral uveitis and characterized by granulomatous inflammatory reaction in the anterior segment which includes mutton fat keratic precipitates, iris nodules, trabecular meshwork nodules, and tent-shaped peripheral anterior synechiae; snowball and/or “string of pearls” opacities in the vitreous; and, in the posterior segment, nodular periphlebitis, multiple peripheral active or atrophic chorioretinal lesions, optic disk nodules/granuloma, and choroidal nodules. Reports of scleral involvement have also been described in sarcoidosis. In acute-onset sarcoidosis, non-granulomatous anterior uveitis may be seen. The 1st international workshop on ocular sarcoidosis in Tokyo in 2006 laid down diagnostic criteria for ocular sarcoidosis, consisting of 7 ocular signs (Table 14.2), 5 laboratory investigations (Table 14.3), and diagnostic criteria based on a combination of ophthalmic signs and laboratory investigations (Table 14.4) [17].
Table 14.2
Clinical signs suggestive of ocular sarcoidosis
1 | Mutton fat keratic precipitates and/or iris nodules at papillary margin or on stroma |
2 | Trabecular meshwork nodules and/or tent-shaped peripheral anterior synechiae |
3 | Snowballs/strings of pearls vitreous opacities |
4 | Multifocal peripheral chorioretinal lesions (active and atrophic) |
5 | Nodular and/or segmental periphlebitis (with or without candle wax exudate) and/or macroaneurysm |
6 | Optic disk nodules/granuloma and/or solitary choroidal nodule |
7 | Bilateral inflammation (evident on clinical examination or on investigational imaging) |
Table 14.3
Laboratory investigations in suspected ocular sarcoidosis
1 | Negative tuberculin test in a patient who either had BCG vaccination or previously had a positive tuberculin test |
2 | Elevated serum angiotensin-converting enzyme and/or elevated serum lysozymea |
3 | Chest X-ray: bilateral hilar lymphadenopathy |
4 | Abnormal liver enzyme tests (any 2: of alkaline phosphatase, aspartate transaminase, alanine transaminase |
5 | Chest CT scan in patients with normal chest X-ray |
Table 14.4




Diagnostic criteria for ocular sarcoidosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


