Ocular Pharmacology of Antifungal Drugs
Denis M. O’Day
W. Steven Head
Supported in part by an unrestricted grant from Research to Prevent Blindness
Fungi are complex eukaryotic organisms. Unlike bacteria, they contain a nucleus, nucleolus, mitochondria, ribosomes, and centrioles. An important feature is the cell wall, which is composed principally of chitin and, in some instances, cellulose. Fungi that are ocular pathogens exist in either a filamentous or yeast form, but certain fungi such as Candida albicans are dimorphic, depending on culture conditions.
The development of antifungal therapy has been a slow process. The similarities between fungal and mammalian cells have proved to be formidable barriers to progress. Attention has focused on agents that would disrupt the cell wall or interfere with metabolic processes within the fungal cell. Although many different compounds with antifungal activity in vitro have been identified, the polyene antibiotics (most notably amphotericin B and natamycin) were the first to demonstrate effective clinical activity for ocular infections. With the discovery of the antifungal activity of the azole compounds, and now the echinocandins, however, two new classes of agents have slowly evolved. As a result, the future of antifungal therapy is considerably brighter now than it appeared to be just a few years ago.
Regrettably, little effort has been expended by drug companies to develop agents with pharmacologic profiles appropriate for the eye. This is despite the high prevalence of ocular fungal infections, particularly in tropical areas of the world, where the population at risk is also the greatest. Instead, systemic preparations have been adapted by ophthalmologists for topical, subconjunctival, or intraocular use. In many instances, there is imperfect knowledge of the ocular pharmacology of these agents, and what is known has had to be gleaned in great part from experimental studies in animals and experience in treating individual cases or small, uncontrolled case series. More recently, treatment studies of much larger patient cohorts have begun to supplement this earlier experience.
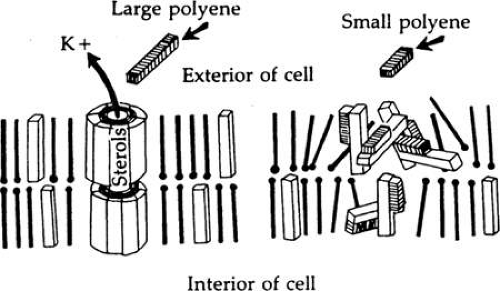
Polyenes
Polyene antibiotics, the first effective antifungal agents to be discovered, are produced by the genus Streptomyces.1 They share a common molecular structure, consisting of a conjugated double-bond system of variable size, which is linked to mycosamine, an amino acid sugar. The polyenes are classified according to the number of double bonds present. Their primary mode of action is to bind to ergosterol in the cell membrane, causing increased permeability and cell leakage. This general disruption of the cell membrane causes cell death.2,3 Although all polyenes, regardless of size, show this binding, the mechanism by which cell damage occurs differs depending on whether the polyene is large, with 35 or more carbon atoms (e.g., amphotericin B), or small, with less than 30 carbon atoms (e.g., natamycin). Large polyenes have the ability, because of size, to form channels in the cell membrane; this allows for electrolyte movement and leads to potassium loss.3 Small polyenes are unable to span the width of the cell membrane; instead, they are believed to accumulate in the membrane, forming “blisters” that then disrupt cellular integrity (Fig. 1).4 The polyenes bind to the sterol in the cell membrane of eukaryotic cells preferentially to ergosterol over cholesterol. It is this preferential affinity for ergosterol that makes the polyene attractive as an antifungal agent, because the primary fungal cell membrane sterol is ergosterol. Cholesterol is the dominant sterol in human cell membranes. Nonetheless, there is enough binding to cholesterol to create toxic side effects with these agents, whether used systemically or topically. There is also evidence that they can cause oxidative damage to the cells.3,5,6 Attempts to reduce toxicity by altering the chemistry of these compounds have so far been unsuccessful. In this chapter, only two polyenes will be considered: amphotericin B and natamycin. Nystatin, the first polyene to be discovered (in 1950), does not have any practical applications in ophthalmology.
Amphotericin B
Amphotericin B (Fig. 2), produced by Streptomyces nodosus,1 was the first polyene shown to be effective in treating systemic mycoses.7 It is poorly soluble in water and has a tendency to degrade when exposed to light.8 In vivo, the rapid tissue binding of amphotericin B limits the actual amount of bioactive drug. Several approaches have been tried in an effort to increase solubility and drug bioavailability while limiting toxicity, including methyl esterification and combination with liposomes and other vehicular compounds. Methyl esterification appeared promising initially because of enhanced solubility9; however, severe toxicity led to abandonment of this approach.10 Amphotericin B lipid complexes, such as Abelcet (Enzon, Piscataway NJ), Amphocil (Sequus Pharmaceuticals, Menlo Park, CA), and the liposomal encapsulated Amphotericin B compounds, Fungisome (Lifecare Innovations Pvt. Ltd., Haryana, India) and AmBisome (Astellas Pharma, Deerfield, IL.), are now available, and we can expect new formulations of amphotericin B in other lipid vehicles. These promising new preparations eliminate the need for the deoxycholate solubilizer, the prime cause of pain and poor compliance when administered topically to the eye. Consequently, reduced toxicity allows the use of more drug both systemically and locally in the eye.3,11 In another experimental approach, the application of heat to deoxycholate –amphotericin B to induce a supra-molecular rearrangement has resulted in reduced mammalian cell toxicity in vitro without affecting antifungal activity.12
Amphotericin B is available for intravenous use in 20-mL vials containing 50 mg of amphotericin B powder, 41 mg of sodium deoxycholate, and a sodium phosphate buffer. Before intravenous injection, the powder is reconstituted to a concentration of 5 mg/mL in 10 mL of distilled water.
Amphotericin B has been used intravenously since its discovery for the treatment of ocular infections; however, its pharmacokinetic profile for ocular tissues is not particularly good. The most useful application appears to be for the treatment of endogenous and exogenous endophthalmitis caused by Candida species. Levels achievable within the vitreous and posterior eye structures appear to be sufficient for these highly susceptible organisms, although not for other filamentous fungi. Concentrations of biologically active amphotericin B in the cornea and the anterior eye after intravenous administration have consistently been low.13,14,15,16 However, Goldblum et al. have reported recently high levels of amphotericin B in the cornea, aqueous, and vitreous of inflamed eyes of rabbits following the intravenous administration of liposomal Amphotericin B.17,18 The apparent therapeutic success of both intravenous amphotericin B lipid complex and liposomal amphotericin B has also been documented in case reports of endophthalmitis caused by Candida albicans and filamentous fungi.19,20
Topical Administration
Although there is no preparation of amphotericin B specifically designed for ophthalmic use, this agent has been used topically for the treatment of fungal keratitis since the late 1950s. Toxicity is a troublesome complication. Because of this problem, Wood and Williford21 evaluated amphotericin B (Fungizone) that had been diluted with distilled water to a concentration of 0.15% in a series of patients with mycotic keratitis. They demonstrated both efficacy and markedly reduced toxicity. In a further series, reduction of the concentration of amphotericin B to 0.05% virtually abolished toxic reactions. Animal studies likewise showed that concentrations as low as 0.03% were remarkably efficacious against susceptible Candida species.22,23 The use of topical concentrations greater than 0.15% has been reported, but this is not recommended because of toxicity; there is little evidence of superior efficacy in the higher concentrations. The topical preparation, when stored at 36°C, retains potency for 1 week. Care should be taken to handle the solution aseptically, because it does not contain a bacteriostatic agent.24
There have been numerous clinical and experimental studies of the efficacy of topical amphotericin B in concentrations ranging from 0.05% to 1%. The pharmacokinetic profile is not particularly good (Table 1). In particular, the corneal epithelium appears to be a powerful barrier to corneal penetration. This is an important issue because the epithelium may heal over fungal lesions in the cornea.25,26 In animal studies, topical amphotericin B 0.15% was virtually unable to penetrate the corneal stroma when the epithelium was intact. Removal of the epithelium was associated with greatly increased penetration, and the degree of penetration was found to be proportional to the size of the epithelial defect.27 Efficacy was also greatly enhanced in these models.
Table 62.1. Ocular Drug Concentrations of Polyenes* | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
When the epithelium is absent, amphotericin B also appears to pass through the cornea to the anterior chamber. Penetration of inflamed corneas is also good. Amphotericin B (0.15%) administered topically was present in the cornea and aqueous of rabbit eyes inflamed by the intrastromal injection of clove oil, even in the presence of an intact epithelium.
The high concentrations of drug are mitigated by a very low bioactivity due to tissue binding. In Dutch-belted rabbits, this bioactivity has been measured at 7% of the total drug in the cornea and 5% of the total drug in aqueous humor.26 Despite this, a therapeutic concentration of drug is achievable in the cornea with intense topical therapy.
The optimal frequency for the topical administration of amphotericin B is unknown. However, animal studies suggest that an initial loading approach of one drop every 5 minutes for 1 hour leads to a rapid accumulation of drug within the cornea with drug still detectable 24 hours after the last drop.28 In the clinical setting, a practical approach is to give one drop every half hour initially with a gradual reduction to six to eight drops per day. After the infection is under control, this can be further reduced to three to four drops daily.
In some studies, collagen shields impregnated with amphotericin B were applied directly to infected corneas as a means of enhancing drug levels.29,30,31 The pharmacologic advantage of this approach over less-expensive topical therapy is uncertain. In one study, the use of topically applied liposome-encapsulated amphotericin B was not associated with significantly increased corneal drug concentration.32
Subconjunctival Administration
Subconjunctival injections of amphotericin B have been recommended for the treatment of fungal keratitis and scleritis. Experience with human cases33 and experimental studies in animals34 demonstrate the severe toxicity of this approach. Ulceration and necrosis of the conjunctiva may occur with inflammation of the underlying sclera and ciliary body. This appears to be due to both the deoxycholate salt that is used as an emulsifying agent and the amphotericin B itself.33 The injections are also associated with severe pain. Studies in animal models suggest that the amount of drug that enters the cornea, anterior chamber, or vitreous cavity is negligible (see Table 1).35 This form of therapy is no longer recommended.
Intracameral Administration
With knowledge of the limited efficacy of systemic and topical amphotericin B in severe intraocular infections, clinicians have advocated the use of intravitreal injections. There is good evidence that the intravitreal injection of 5 μg of amphotericin B can be efficacious in the treatment of Candida sp. infections36,37 alone or in combination with systemic amphotericin B or other drugs. The toxicity of intravitreal amphotericin B in a single injection appears to be low and within the acceptable range.37,38,39 Repeated injections do carry an increased risk of toxicity, although a number of cases have been reported in which repeated injections in these concentrations led to no after effects in the eye.40,41,42,43,44 Injection of liposomal amphotericin B has the theoretic potential to increase the half-life while reducing toxic side effects.11 This formulation was also found in an animal model to exhibit less toxicity than either amphotericin B deoxycholate or amphotericin B lipid complex when administered by intravitreal injection.44 For cases in which there is evidence of anterior endophthalmitis due to progression of infection from the cornea into the anterior chamber, amphotericin B can be irrigated into the anterior chamber.45 Our experience using this drug in concentrations of 5 μg/mL is largely limited to cases at surgery when the chamber is irrigated before penetrating keratoplasty is performed.
Susceptibility of Organisms to Amphotericin B
Amphotericin B has a rather narrow spectrum of activity. It is most effective against yeasts, particularly Candida and Cryptococcus species, but is much less useful for the treatment of filamentous fungus infections. This experience with systemic mycoses is confirmed mostly in the treatment of ocular mycoses. Although clinical and experimental evidence suggests that Candida albicans keratitis is very susceptible to topically applied amphotericin B in concentrations of 0.03% to 0.15%, and that Candida endophthalmitis can be effectively treated by intraocular and/or systemic amphotericin B, there is little evidence that endophthalmitis due to filamentous organisms can be treated by this route. Amphotericin B does exert some antifungal activity against Aspergillus, but experience in saving eyes with Aspergillus endophthalmitis has been disappointing.45,46
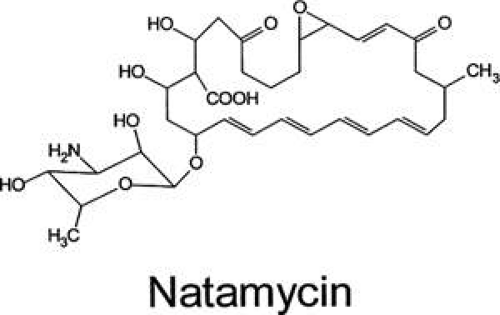
Natamycin (Pimaricin)
The other important polyene for use in ocular disease is natamycin (Fig. 3). This tetraene polyene is the only antifungal agent commercially available in the United States for use as an ophthalmic preparation. It is marketed by Alcon Laboratories as a 5% suspension (Natacyn). It can be stored at room temperature or refrigerated, but it should not be frozen or exposed to light or high temperatures.
Natamycin was discovered in 1958. Because of its physical characteristics, natamycin is extremely difficult to study. Much of what is known about the drug has been learned, therefore, from clinical experience. However, some laboratory work does provide information about its pharmacokinetics and pharmacology (see Table 1). Natacyn is available in volumes of 15 mL, stored in glass bottles. As is the case with most polyenes, natamycin is insoluble in water, and the commercial preparation is a microfine suspension that must be shaken well before each use. After topical administration, the drug often adheres to the area of corneal ulceration and may be seen in the fornices.
Pharmacokinetics and Pharmacology
Natamycin is easily absorbed into the cornea; however, it exhibits a high degree of binding in tissue, which severely limits its bioactivity.28 In addition, the corneal epithelium is a substantial barrier to corneal penetration. These characteristics account for the poor pharmacokinetic profile of this drug. However, extensive clinical experience with several fungi48,49 in addition to laboratory studies,25,50,51,52 supports its value as an effective antifungal agent. In experimental pharmacokinetic studies using 14C radiolabeled natamycin, high concentrations of the agent were detected in the cornea by radioassay after intensive topical administration. High levels were also detected in the aqueous.28 Because of tissue binding, only 2% of this drug is bioactive. The relatively high total corneal drug levels achievable by intensive administration assure that adequate therapeutic levels in the cornea are available. In experimental studies, it has been demonstrated that removal of the corneal epithelium dramatically increases penetration and efficacy.25,51,52
Topical Administration
As with amphotericin B, an initial loading approach is recommended. This consists of the administration of one drop every half hour with a gradual reduction to six to eight times and then three to four times a day. No other routes of administration are practical with this drug.
Toxicity
Topical natamycin 5% suspension is well tolerated in the cornea. Corneal toxicity does occur, however, with prolonged use, usually in the form of a punctate keratitis. Diffuse conjunctival inflammation is also seen, and a consistent low-grade inflammation has been reported.23,53 In an animal model, natamycin did not retard the healing of corneal epithelial defects.54 Natamycin has been shown to be most effective against the filamentous fungi, especially Fusarium, Aspergillus and Curvularia spp. Infections,48,53,55 which are the most common causes of filamentous fungal keratitis worldwide. Numerous clinical series in the United States and elsewhere have established the primacy of natamycin in the treatment of fungal infections caused by filamentous fungi; it is less effective against yeast infections.24 It should be noted, however, that treatment failures presumably due to organism resistance occur in both Fusarium and Aspergillus keratitis as well as with other organisms.
Azoles
A new era in antifungal therapy began in the mid-1960s with the discovery of the antifungal properties of the antiprotozoan azole compounds. In the succeeding 40 years, the list of these agents with antifungal activity has slowly but steadily grown. There are two major types of azoles used in ophthalmology. Imidazoles, the first to be discovered, are five-membered ring structures containing two nitrogen atoms. A complex side chain is attached to one of the nitrogen atoms (Fig. 4). The triazoles, developed more recently, contain three nitrogen atoms in a five-membered ring (Fig. 5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree