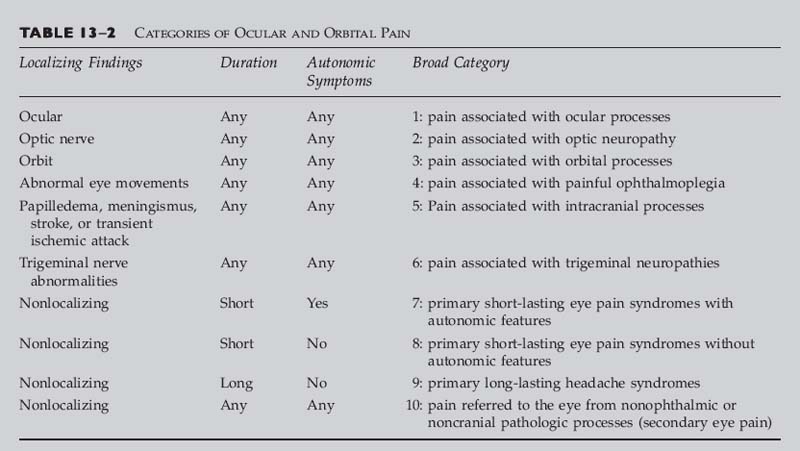
Chapter 13 This chapter can be used to aid in the diagnosis of patients complaining of eye, periorbital, and retro-orbital pain, or headache and facial pain referred to the orbital region. In it, “eye pain” designates any pain or discomfort referred by the patient to the eye itself, pain localized to the retrobulbar, orbital, retro-orbital, or periorbital regions, or headache or facial pain that is especially localized to the eye or surrounding structures. Eye pain is a common complaint often presenting to ophthalmologists, neurologists, neurosurgeons, family practitioners, and internists. In many cases, the symptoms are magnified by the patient’s concerns about possible blindness, the presence of an eye or brain tumor, or the presence of other dangerous processes such as a cerebral aneurysm. Pain in a patient with a “red or inflamed eye” is usually due to infectious or inflammatory diseases affecting the cornea, conjunctiva, episclera, or sclera, which are usually easily diagnosed as such by ophthalmologists. A”quiet eye” is defined clinically as one with a clear cornea without redness or irritation of the conjunctiva or sclera. In this chapter, we discuss various etiologies of eye pain in the “quiet eye” (outlined in Table 13–1). The causes of eye pain are divided into two types: (1) those associated with abnormal localizing ophthalmologic and neuro-ophthalmologic findings (including trigeminal neuropathies); and (2) those with a normal ophthalmologic and neurologic examinations. The latter are further divided into specific short-lasting or long-lasting headache or eye pain syndromes, pain referred to the eye from other pathologic processes (secondary eye pain) sometimes distant from structures concerned with vision, and pain from orbital, superior orbital fissure, cavernous sinus, or intracranial infiltrative, neoplastic, or inflammatory disease processes with normal ophthalmologic and neuro-ophthalmologic exam. Unfortunately, in many patients, no etiology for the pain or characteristic eye pain or headache syndrome is discerned, and one is left with a diagnosis of “idiopathic eye pain,” “eye strain,” or “atypical facial pain.” Before using Table 13–2 (page 132), to determine the category of ocular and orbital pain, you should establish the following: • Is the ocular examination normal? To establish this, it is necessary to examine the anterior segment, measure the intraocular pressure, assess the tear film, and determine if the angle is closed. Are there signs of retinal inflammation, detachment, intraocular tumor, scleritis, iritis, or vitreitis? • Is there evidence of optic nerve abnormality? Evaluate the near and distance visual acuity, color vision, visual fields, the pupil responses, including evaluation for a relative afferent pupillary defect or afferent pupillary defect (APD), and determine whether the disc is normal, atrophic, or edematous. • Is the orbital examination normal? Does palpation reveal a mass? Is there proptosis or other change in globe position? Is there an orbital bruit? Is the lid position normal? • Is the ocular motility normal? • Are there signs of papilledema, meningismus, stroke, or other intracranial processes? • Is there trigeminal sensory loss or dysfunction? Is there sensory loss or unusual sensitivity over the forehead (ophthalmic branch), cheek (maxillary branch), or jaw (mandibular branch) on either side? Is the corneal reflex depressed (trigeminal or facial nerve injury)? • If there are no localizing findings, then determine the following: (1) Is the duration of the pain short or long? (2) Are there associated autonomic symptoms? Examples include lacrimation, nasal congestion and rhinorrhea, forehead and facial sweating, eyelid edema, ptosis, miosis, and conjunctival injection.
OCULAR AND ORBITAL PAIN
Pain Associated with Localizing Ophthalmologic or Neuro-Ophthalmologic Findings I. Ocular processes A. Open-angle glaucoma 1. Primary open-angle glaucoma (rare) 2. Glaucomatocyclitic crisis (Possner-Schlossman syndrome) 3. Lens-induced glaucoma a. Phacolytic glaucoma b. Lens particle glaucoma c. Phacoanaphylaxis 4. Intraocular tumors 5. Trauma a. Angle recession b. Hemolytic c. Ghost cell 6. Closure of a cyclodialysis cleft B. Angle closure glaucoma 1. Primary angle-closure glaucoma 2. Plateau iris 3. Lens-induced angle closure 4. Neovascular 5. Iridocorneal-endothelial (ICE) syndrome 6. Intraocular tumors 7. Ciliary block (malignant) glaucoma 8. Epithelial and fibrous downgrowth 9. Following intraocular surgery 10. Nanophthalmos C. Corneal disease 1. Dry eyes 2. Toxicity 3. Infectious keratitis a. Viral keratitis [e.g., herpes simplex keratitis, varicella zoster keratitis, Epstein Barr (EB) virus] b. Bacterial c. Fungal d. Acanthamoeba 4. Meibomian gland dysfunction 5. Allergic keratitis (e.g., vernal keratoconjunctivitis) 6. Intersitial keratitis 7. Thygeson’s superficial punctate keratitis 8. Superior limbic keratoconjunctivitis 9. Peripheral ulcerative keratitis a. Mooren’s ulcer b. Autoimmune connective tissue disease (e.g., rheumatoid arthritis, Wegener’s granulomatosis, systemic lupus erythematosus, polyarteritis nodosa, ulcerative colitis) 10. Recurrent corneal erosions 11. Corneal abrasion 12. Keratoconus with acute hydrops 13. Foreign bodies: corneal or conjunctival 14. Bullous keratopathy D. Uveitis 1. Idiopathic iridocyclitis 2. Infectious iridocyclitis a. Herpes simplex b. Herpes zoster c. Syphilis 3. Lens induced a. Oversized implant b. Phacotoxic uveitis 4. Sympathetic ophthalmia 5. Uveitis-glaucoma-hyphema (UGH) syndrome 6. Posterior uveitis a. Toxoplasmosis b. Behcet’s disease c. Vogt-Koyanagi Harada’s disease d. Multifocal choroiditis and panuveitis 7. Endophthalmitis a. Endogenous (e.g., bacterial, fungal) b. Exogenous (e.g., trauma, postoperative) E. Scleritis and episcleritis 1. Idiopathic 2. Infectious a. Bacterial b. Fungal c. Tuberculosis d. Syphilis e. Leprosy f. Herpes simplex g. Herpes zoster 3. Connective tissue disease a. Rheumatoid arthritis b. Wegener’s granulomatosis c. Polyarteritis nodosa d. Systemic lupus erythematosus e. Relapsing polychondritis f. Crohn’s disease 4. Ocular surgery 5. Sarcoidosis 1. Uveal melanoma 2. Metastasis 3. Following radiotherapy G. Ocular ischemia 1. Previous eye muscle surgery 2. Previous scleral buckling surgery 3. Sickle cell disease H. Suprachoroidal hemorrhage I. Trauma: scleral laceration or rupture J. Retina/choroid process 1. Photocoagulation 2. Inflammatory disease [e.g., bird-shot chorioretinopathy, acute posterior multifocal placoid pigment epitheliopathy (APMPPE)] II. Processes affecting the optic nerve A. Optic neuritis B. Ischemic optic neuropathy C. Compressive optic neuropathy 1. Intracranial or intraorbital benign and malignant tumors a. Meningioma b. Glioma c. Craniopharyngioma d. Pituitary adenoma e. Lymphoma and leukemia f. Germinoma g. Sinus histiocytosis with lymphadenopathy h. Nasopharyngeal cancer i. Metastasis 2. Extramedullary hematopoiesis 3. Orbital fractures with bone fragment, hematoma, or edema 4. Pneumatocele 5. Inflammatory or infectious diseases (e.g., mucoceles) 6. Idiopathic hypertrophic cranial pachymeningitis 7. Primary bone diseases (e.g., osteopetrosis, fibrous dysplasia, craniometaphyseal dysplasia, Paget’s disease, aneurysmal bone cyst, pneumosinus dilatans, etc.) 8. Vascular etiologies a. Orbital hemorrhage b. Orbital venous anomalies c. Carotid artery and anterior communicating artery aneurysms d. Supraclinoid carotid artery compression e. Arteriovenous malformations 9. Thyroid ophthalmopathy 10. Iatrogenic (e.g., intracranial catheters, postoperative). D. Infiltrative or inflammatory optic neuropathy 1. Neoplastic (e.g., plasmacytoma and multiple myeloma, carcinomatous meningitis, leukemia, lymphoma) 2. Infectious etiologies a. Bacteria [e.g., syphilis, tuberculosis, Lyme disease, Bartonella henselae (cat-scratch disease), Mycoplasma, Whipple’s disease, brucellosis, β-hemolytic streptococcus, meningococcus] b. Focal infection or inflammation (e.g., paranasal sinusitis or mucocele, postinfectious, malignant otitis externa) c. Fungi (e.g., Aspergillus, histoplasmosis, cryptococcus, mucormycosis) d. Rickettsiae (e.g., Q fever, epidemic typhus) e. Protozoa (e.g., toxoplasmosis) f. Parasites (e.g., toxocariasis, cysticercosis) g. Viruses [e.g., adenovirus, hepatitis A, hepatitis B, cytomegalovirus (CMV), Coxsackie B, rubella, chickenpox, herpes zoster, herpes simplex virus I, EB virus (infectious mononucleosis), measles, mumps, influenza, HTLV-1, HIV (AIDS) related] 3. Inflammatory diseases a. Churg-Strauss angiitis b. Contiguous sinus disease c. Behcet’s disease d. Sarcoidosis e. Wegener’s granulomatosis f. Systemic lupus erythematosus g. Sjögren’s syndrome h. Relapsing polychondritis i. Polyarteritis nodosa j. Rheumatoid arthritis k. Inflammatory bowel disease III. Orbital processes A. Tumor 1. Primary (including meningioma, adenoma, lacrimal gland carcinoma, neurilemmoma, melanoma, lymphoma, Hodgkin’s disease) 2. Metastatic B. Infection (orbital cellulitis, dacryoadenitis) 1. Bacterial (e.g., septicemia, penetrating trauma, adjacent sinusitis, sinus mucocele) 2. Viral (e.g., herpes zoster) 3. Fungal (e.g., mucormycosis, aspergillus, Bipolaris hawaiiensis, actinomycosis) 4. Parasites (e.g., cysticercosis, trichinosis) C. Inflammatory and infiltrative processes 1. Thyroid orbitopathy 3. Lymphoid hyperplasia 4. Giant cell arteritis 5. Orbital polymyositis and giant cell myocarditis 6. Sarcoidosis 7. Wegener’s granulomatosis 8. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) 9. Erdheim-Chester disease 10. Orbital amyloidosis 11. Bilateral nonspecific inflammatory or Graves’-like orbitopathy with seminoma D. Vascular 1. Arteriovenous malformation 2. Orbital hemorrhage 3. Orbital venous anomalies 4. Dural-cavernous sinus fistula 5. Carotid-cavernous sinus fistula E. Posttraumatic (e.g., amputation neuroma, photo-oculodynia syndrome) and postoperative (e.g., postscleral buckle procedure, postevisceration) eye pain IV. Cavernous sinus and superior orbital fissure processes A. Aneurysm of the internal carotid artery B. Tumors (e.g., meningioma, pituitary adenoma, nasopharyngeal carcinoma, cavernous hemangioma, hemangiopericytoma, lymphoma, myeloma, metastasis, Waldenstrom’s macroglobulinemia) C. Cavernous sinus thrombosis D. Infections (e.g., herpes zoster, aspergillus, mucormycosis) E. Tolosa-Hunt syndrome (idiopathic granulomatous inflammation of cavernous sinus) F. Inflammatory processes (e.g., sarcoidosis, Wegener’s granulomatosis) G. Carotid-cavernous sinus or dural-cavernous sinus fistula H. Ischemic ocular motor nerve palsies (e.g., due to diabetes mellitus, giant cell arteritis, vasculitis, etc.; localization of process may be anywhere along course of ocular motor nerve) I. Neurosurgical complications J. Posttraumatic V. Intracranial processes A. Tumors 1. Primary (e.g., pituitary adenoma, meningioma, craniopharyngioma, chondroma, lymphoma) 2. Secondary (e.g., metastasis, nasopharyngeal carcinoma, carcinomatous meningitis. B. Pseudotumor cerebri C. Infections or inflammatory conditions (e.g., sarcoidosis, Wegener’s granulomatosis) D. Vascular 1. Aneurysms 2. Arteriovenous malformation 3. Cerebral infarction, transient ischemic attacks (TIAs), or hemorrhage (e.g., ophthalmic pain with posterior cerebral artery infarction) 4. Venous sinus thrombosis 5. Posttraumatic (e.g., subdural hematoma) 6. Pituitary apoplexy 7. Cerebral vasculitis 8. Hypertensive encephalopathy E. Low-pressure headache (intracranial hypotension) VI. Trigeminal neuropathies A. Tumors 1. Primary (e.g., meningioma, schwannoma, etc.) 2. Secondary (e.g., metastasis, carcinomatous meningitis, squamous cell tumor of skin, nasopharyngeal carcinoma, etc.) B. Posttraumatic (e.g., basal skull fracture, neurosurgical procedures) C. Infectious/inflammatory processes (e.g., aspergilloma, amyloidoma, sarcoidosis, Wegener’s granulomatosis, herpetic and postherpetic neuralgia) D. Vascular (e.g., carotid aneurysm, cavernous hemangioma, dural-cavernous sinus fistula) VII. Raeder’s paratrigeminal syndrome A. Neuroparalytic (neurotropic) keratitis B. Isolated trigeminal neuropathy 1. Systemic lupus erythematosus 2. Scleroderma 3. Sjögren’s syndrome 4. Dermatomyositis 5. Rheumatoid arthritis 6. Mixed connective tissue disease 7. Idiopathic Pain Syndromes with a Normal Ophthalmologic and Neuro-Ophthalmologic Examination I. Primary short-lasting headache syndromes A. With autonomic features 1. Cluster headache a. Episodic b. Chronic 2. Cluster-tic syndrome 3. Paroxysmal hemicranias a. Chronic (CPH) 4. Chronic paroxysmal hemicrania (CPH): tic syndrome 5. SUNCT (short-lasting unilateral neuralgiform pain with conjunctival injection and tearing) syndrome B. Without autonomic features 1. Trigeminal neuralgia 2. Sphenopalatine neuralgia 3. Idiopathic stabbing headache (jabs and jolts syndrome, ice-pick headache, “needle-in-the-eye” syndrome) 4. Valsalva maneuver headache a. Cough headache b. Benign exertional headache 5. Headache associated with sexual activity 6. Cold stimulus (ice cream) headache 7. Hypnic headache II. Primary long-lasting headache syndromes A. Migraine 1. With aura 2. Without aura B. Tension headache and eye strain (e.g., due to uncorrected refractive error or heterophoria) C. Hemicrania continua (episodic and chronic) D. Idiopathic eye pain (includes atypical facial pain and psychogenic pain) III. Pain referred to the eye from nonophthalmic or noncranial pathologic processes (secondary eye pain) A. Sinus disease (e.g., sphenoid and frontal sinusitis) B. Diseases of the teeth, jaw, and related structures C. Vascular disease 1. Carotodynia 2. Carotid artery dissection 3. Carotid artery occlusion or stenosis (including the ocular ischemic syndrome) 4. Postcarotid endarterectomy 5. Giant cell arteritis D. Eye pain with neck disease (cervicogenic headache or eye pain) E. Face pain with lung cancer IV. Orbital, superior orbital fissure, cavernous sinus, or intracranial infiltrative, neoplastic, or inflammatory disease processes with normal ophthalmologic and neuro-ophthalmologic exam |
From Brazis PW, Lee, AG, Stewart M, and Capobianco D. Clinical Review: The differential diagnosis of pain in the quiet eye. The Neurologist 2002;8:82–100.
BROAD CATEGORY 1: PAIN ASSOCIATED WITH LOCALIZING NEURO-OPHTHALMOLOGIC OR OPHTHALMOLOGIC FINDINGS–OCULAR PROCESSES
QUESTIONS TO ASK AND POINTS TO KEEP IN MIND
1. Is the eye pain associated with subjective or objective visual loss?
2. If the eye pain is episodic and associated with blurred vision or halos, always assess for angle closure glaucoma (best assessed by gonioscopy).
3. If the pain seems superficial (e.g., foreign body sensation), consider dry eyes as an etiology.
4. Patients with deep, boring eye pain need careful funduscopy to evaluate for changes of scleritis, which may be subtle, or the presence of a choroidal tumor.
GLAUCOMA
Classic Presentation
• Pain is rare with primary open-angle glaucoma.
• Pain may occur with other etiologies of secondary open-angle glaucoma (Table 13–1).
• Patients with angle-closure glaucoma may have associated nausea or vomiting that could be confused with migraine, cluster headache, or an intracranial structural lesion.
• Subacute, primary angle-closure glaucoma with pupillary block refers to intermittent episodes of angle-closure glaucoma during which patients may report only blurred vision or halos around lights, often with mild to moderate eye pain.
• Patients with intermittent angle closure have pain episodes lasting minutes to hours, and the eye may appear normal between attacks with the exception of a shallow anterior chamber angle.
Red Flags
 Always consider acute angle-closure glaucoma in any patients with severe, especially acute, head pain localized within or around the eye.
Always consider acute angle-closure glaucoma in any patients with severe, especially acute, head pain localized within or around the eye.
 Any patient with episodes of eye pain associated with visual blur or loss should undergo thorough ophthalmologic examination, including gonioscopy.
Any patient with episodes of eye pain associated with visual blur or loss should undergo thorough ophthalmologic examination, including gonioscopy.
CORNEAL DISEASE
Classic Presentation
• Mechanical stimulation of cornea may cause eye pain often described as a “scratched eye” or a “foreign-body sensation.”
• Corneal pain may be referred to the frontal head regions.
• The differential diagnosis for corneal irritation is outlined in Table 13–1.
Red Flags
 Most patients with corneal problems also manifest excessive tearing, photophobia, blepharospasm, and conjunctival injection.
Most patients with corneal problems also manifest excessive tearing, photophobia, blepharospasm, and conjunctival injection.
 Always consider dry eyes as a potential cause of such pain.
Always consider dry eyes as a potential cause of such pain.
ANTERIOR UVEITIS (IRITIS)
Classic Presentation
• Acute anterior uveitis presents with photophobia, eye pain, redness, lacrimation, and decreased vision in the affected eye.
• Eye pain may be quite severe, may be throbbing, and may radiate to other head and facial areas, including the teeth and sinuses.
• Pain may be prominent at night or in early morning.
• Cell and flare in the anterior chamber and keratic precipitates are usually present.
• Uveitis-glaucoma-hyphema (UGH) syndrome may cause transient monocular visual loss of gradual onset (minutes) and slow recovery (hours to days). This syndrome may follow cataract extraction and intraocular lens implantation.1
• Patients with UGH syndrome may relate a gradual misting of vision sometimes associated with erythropsia (reddening of vision) and variable eye pain.
POSTERIOR AND INTERMEDIATE UVEITIS
Classic Presentation
• Patients usually do not have pain.
• Symptoms include floaters, reduced vision with little or no photophobia, redness, or lacrimation.
Red Flag
 The presence of cell and flare in the anterior chamber and/or keratic precipitates suggests anterior uveitis.
The presence of cell and flare in the anterior chamber and/or keratic precipitates suggests anterior uveitis.
EPISCLERITIS AND SCLERITIS
Classic Presentation
• Episcleritis is a benign, self-limited but recurrent disorder.
• Episcleritis is associated with relatively mild eye pain and redness, injection of the episcleral tissue, eye tenderness, and some tearing.
• Scleritis usually presents with intense, boring pain associated with photophobia and tearing.
• Necrotizing scleritis without inflammation may not cause pain.
• Pain of scleritis is often localized to the eye but may radiate into sinuses, jaw, frontal regions, or temple.
• Anterior necrotizing scleritis with inflammation is the most severe form and presents with severe pain and redness.
• Posterior scleritis is often difficult to diagnose and may present with prominent eye pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree