 Questions
Questions
1. A patient presents complaining of decreased vision in the left eye. His acuities are 20/20 in the right eye and 20/100 in the left eye. The examination is entirely unremarkable, and the diagnosis of factitious visual loss is considered. The test that would be most useful in establishing this diagnosis is
a. optokinetic nystagmus testing.
b. gently rocking a large mirror in front of the patient with the good eye occluded.
c. introducing a prism base up in front of the left eye while the patient is reading binocularly.
d. performing a fogging refraction.
2. Which one of the following concerning the visual evoked response (VER) is false?
a. The VER is an electrical signal that must be extracted from the simultaneously generated electroencephalogram (EEG).
b. The stimulus may consist of either a flash of white light or a pattern, presented either transiently or continuously via pattern reversal.
c. The two critical parameters used for functional evaluation include the height of the first positive or upward wave (amplitude) and the amount of time between stimulus presentation and the appearance of this wave (latency).
d. Uses of the flash VER include visual acuity assessment in preverbal children, assessment of optic nerve function in suspected multiple sclerosis, and reliable establishment of factitious visual loss.
3. Which of the following is true of cancer-associated retinopathy (CAR)?
a. ERG findings are typically normal.
b. The underlying tumor expresses an antigen that is homologous to a 23-kd retinal photoreceptor protein identified as the calciumbinding protein recoverin.
c. The underlying cancer is typically breast cancer.
d. Vision loss is stationary.
4. Which of the following is true of melanoma-associated retinopathy (MAR)?
a. This syndrome primarily involves the rods.
b. ERG is typically normal.
c. Treatment is effective for MAR.
d. MAR is a common syndrome in patients diagnosed with melanoma.
5. Which of the following concerning magnetic resonance imaging (MRI) is true?
a. Long repetition times (TR) and long echo times (TE) are used to generate T1-weighted images.
b. On a T1-weighted image, vitreous is dark, and on a T2-weighted image, vitreous is bright.
c. Air and cortical bone give a bright (hyperintense) signal on MRI.
d. T1-weighted images tend to show pathology well, whereas T2-weighted images tend to show anatomy well.
6. Which one of the following concerning the intracranial portion of the optic nerve is false?
a. It is typically 10 to 17 mm in length.
b. It enters the intracranial cavity medial to the internal carotid artery.
c. There is generally some redundancy within the intracranial optic nerve.
d. Once it enters the intracranial cavity, the optic nerve no longer has a sheath.
7. Which of the following concerning the optic chiasm is true?
a. As many fibers cross as do not cross.
b. The posterior portion of the chiasm has a high density of macular fibers.
c. The chiasm typically lies 1 mm above the anterior pituitary gland.
d. The superior fibers are the first to cross.
8. Which of the following retrochiasmal locations can induce a monocular visual field defect with a single lesion alone?
a. lateral geniculate body.
b. parietal lobe.
c. temporal lobe.
d. occipital lobe.
9. The lateral geniculate body is divided into six layers and they are segregated depending on which eye the axons originate. Which layers of the lateral geniculate receive axons from the ipsilateral eye versus the contralateral eye?
a. The contralateral eye terminates in layers 1, 2, and 3; the ipsilateral eye terminates in layers 4, 5, and 6.
b. The contralateral eye terminates in layers 1, 3, and 6; the ipsilateral eye terminates in layers 2, 4, and 5.
c. The contralateral eye terminates in layers 1, 4, and 6; the ipsilateral eye terminates in layers 2, 3, and 5.
d. The contraleral eye terminates in layer 2, 3, and 5; the ipsilateral eye terminates in layers 1, 4, and 6.
10. Which of the following features is consistent with a temporal lobe lesion?
a. unformed visual hallucinations.
b. optokinetic nystagmus (OKN) abnormalities.
c. formed visual hallucinations.
d. high congruity of visual field deficits.
11. Which of the following features is not consistent with a parietal lobe lesion?
a. agnosia.
b. right–left confusion.
c. OKN abnormalities.
d. homonymous hemianopia denser superiorly.
12. Which of the following features is not consistent with an occipital lobe lesion?
a. OKN abnormalities.
b. unformed hallucinations.
c. macular sparing.
d. sparing of the temporal crescent.
13. The cause of optic disc edema is
a. swollen peripapillary myelinated nerve fiber layer.
b. extracellular fluid accumulation.
c. interruption of axonal transport.
d. breakdown of the blood retinal barrier.
14. Which of the following concerning papilledema is true?
a. Loss of venous pulsations is a particularly specific finding.
b. Symptoms accompanying papilledema may include visual loss and transient obscurations of vision.
c. The most typical visual field finding in chronic papilledema is an enlarged blind spot.
d. Papilledema is more commonly unilateral.
15. Which of the following are universal findings in patients with pseudotumor cerebri?
a. papilledema.
b. abnormal cerebrospinal fluid composition.
c. normal neurologic examination.
d. increased intracranial pressure.
16. Indication for treatment of pseudotumor cerebri includes which of the following?
a. papilledema.
b. obesity.
c. visual field loss.
d. optic disc drusen.
17. Pseudotumor cerebri, also known as idiopathic intracranial hypertension (IIH), can be associated with the use of all of the exogenous substances except
a. acetylsalicylic acid.
b. nalidixic acid.
c. tetracycline.
d. vitamin A.
18. The most common cause of permanent visual loss in patients with cavernous sinus–dural fistulae is
a. neovascular glaucoma.
b. corneal exposure.
c. open-angle glaucoma.
d. choroidal effusions.
19. All of following concerning giant cell arteritis are true except:
a. It is exceedingly rare in patients <50 years old and is more common in females.
b. Forty percent of untreated patients will develop some form of permanent visual loss.
c. Ninety-five percent of untreated patients will have contralateral involvement of the other eye, within days to weeks.
d. Visual loss is typically mild with visual acuity being better than 20/100 in 60% of the patients.
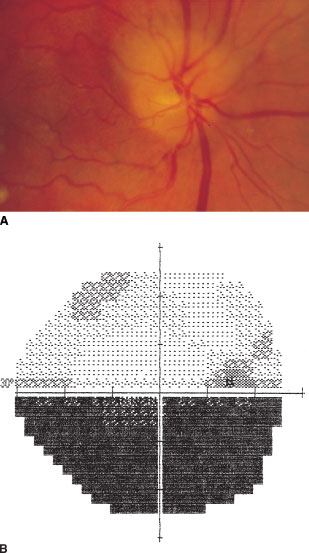
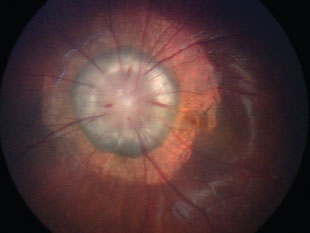
20. A 63-year-old male walks in with complaints of sudden onset of blurring of vision in his right eye. His visual acuity when checked is 20/30 in that eye. The patient’s history includes hypertension and diabetes. The patient currently has no other systemic symptoms. A photo of his right optic nerve and his visual field is shown at the top of the next column (images A and B). His left optic nerve is normal with a cup/disc ratio of 0.1. What is his most likely diagnosis?
a. arteritic anterior ischemic optic neuropathy (AAION).
b. nonarteritic anterior ischemic optic neuropathy (NAION).
c. myelinated nerve fiber layer.
d. optic disc drusen.
21. Which one of the following concerning the patient in question 20 is not true?
a. Visual loss is generally less severe than in the arteritic variety.
b. The condition most frequently associated with it is hypertension.
c. Fluorescein angiography is usually not of benefit in differentiating optic neuritis from this condition.
d. There is approximately a 15% chance of subsequent occurrence in the contralateral eye within 5 years.
22. Treatment for the condition in question 20 is
a. observation.
b. corticosteroids.
c. immunomodulators.
d. hyperbaric oxygen.
23. Approximately what percentage of patients with optic neuritis (and no lesions observed on MRI at the time of the attack) will develop multiple sclerosis (MS) at 15-year follow-up?
a. 1%.
b. 5%.
c. 10%.
d. 25%.
24. What percentage of patients with severe MS will, on autopsy examination, have demyelinated lesions of the optic nerves?
a. 10%.
b. 25%.
c. 50%.
d. more than 90%.
25. Which of the following concerning optic nerve glioma is true?
a. Optic nerve glioma is more frequently seen in children than adults.
b. The vast majority of patients will have associated neurofibromatosis.
c. Optociliary shunt vessels of the disc occur more commonly with optic nerve gliomas than with meningiomas of the optic nerve.
d. These tumors are more likely to be aggressively malignant in children than in adults.
26. Which of the following concerning optic nerve meningiomas is true?
a. It primarily affects children.
b. The majority of patients will have associated neurofibromatosis.
c. On computed tomography (CT) scanning, affected optic nerves have a “kinked” appearance.
d. These tumors are more likely to be aggressively malignant in children than in adults.
27. All of the following are true regarding autosomal dominant optic atrophy except:
a. The most common hereditary optic neuropathy.
b. Dominant optic atrophy is usually slowly progressive throughout life.
c. Presentation typically occurs in the first decade of life.
d. At detection, visual acuity loss is usually moderate, in the range of 20/50 to 20/70.
28. Which of the following concerning Leber’s hereditary optic neuropathy (LHON) is false?
a. All offspring of a female carrier are either affected or carriers.
b. Ten percent of female carriers will be affected.
c. LHON is generally unilateral with vision loss occurring only in the affected eye.
d. A small percentage of patients will enjoy partial recovery late in their course.
29. LHON mitochondrial DNA mutation occurs most frequently at which position of the mito-chondrial DNA?
a. 11778.
b. 3460.
c. 14484.
d. 8280.
30. A 23-year-old man presents complaining of sudden loss of vision in his right eye. His acuities are 20/200 in the right eye and 20/20 in the left eye. Examination is normal with exception of a swollen optic nerve, dilated retinal veins, and scattered dense retinal hemorrhages. The factor that most convincingly argues against the diagnosis of papillophlebitis is the patient’s
a. age.
b. sex.
c. visual acuity.
d. retinal hemorrhages.
31. A patient comes in for a routine eye exam. He does not have any visual complaints and his vision is 20/20 OU. The photo of the right optic nerve is seen below (images A and B). What is the diagnosis?
a. papilledema.
b. myelinated nerve fiber layer.
c. optic disc drusen.
d. optic nerve hypoplasia.
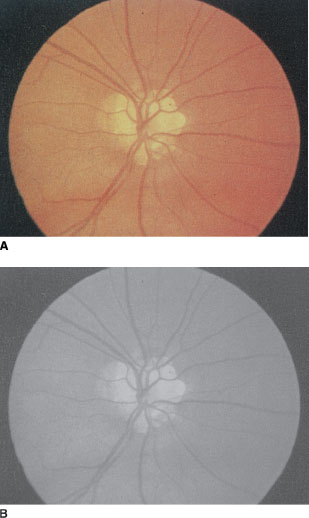
32. Which one of the following concerning the patient in question 31 is not true?
a. Associated loss of acuity is unusual.
b. They are common in African Americans and Asians.
c. They are generally bilateral.
d. Associated visual field defects may resemble those of glaucoma.
33. Which of the following is true regarding morning glory disc anomaly?
a. Occult transsphenoidal basal encephaloceles may be present.
b. It is more common in males than females.
c. Visual acuity is normal in these patients.
d. Retinal vessels emanate from the center of the optic disc.
34. A 49-year-old female notices objects seen out of the right eye tend to shimmer for a couple seconds numerous times per day. At the slit lamp, you are fortunate to see very fine movements of only the right eye. What is the most likely diagnosis?
a. latent nystagmus.
b. superior oblique myokymia.
c. neuromyotonia.
d. periodic alternating nystagmus.
35. Which of the following is true regarding optic pits?
a. Serous detachment of the macula can occur.
b. Optic pits are typically located nasally.
c. Visual field defects are not seen.
d. Optic pits are typically bilateral.
36. Which of the following is true regarding the treatment for optic neuritis?
a. Corticosteroid therapy has no long-term beneficial effect for vision.
b. Oral prednisone is preferred over intravenous methylprednisolone as initial therapy.
c. Intravenous methylprednisolone is proven to reduce the long-term risk of multiple sclerosis.
d. Intravenous methylprednisolone improves the long-term visual acuity compared to no treatment.
37. The most common location for a cerebral aneurysm associated with acute third nerve palsy is
a. The junction of posterior communicating and posterior cerebral arteries.
b. The junction of the vertebral and superior cerebellar arteries.
c. The junction of the posterior cerebral artery and the internal carotid artery.
d. The junction of posterior communicating artery and the internal carotid artery.
38. A 42-year-old diabetic man presents with a painful partial third nerve palsy. On his first follow-up visit, you notice that, when looking down, his upper eyelid appears to retract or lag. This finding essentially rules out the possibility of
a. diabetic third nerve palsy.
b. aneurysm.
c. meningioma.
d. trauma.
39. The most common cause of acquired fourth nerve palsy in adults is
a. tumor.
b. trauma.
c. vascular.
d. idiopathic.
40. The best method for detecting a decompensated congenital fourth nerve palsy is
a. the three-step (Bielschowsky head tilt) test.
b. distance and near prismatic measurements.
c. double Maddox rod testing.
d. vertical fusional amplitude measurements.
41. In a patient with a right fourth nerve palsy, you would expect a
a. left hyperdeviation in primary position that worsens on right gaze and left head tilt.
b. right hyperdeviation in primary position that worsens on left gaze and right head tilt.
c. right hyperdeviation in primary position that worsens on right gaze and right head tilt.
d. right hyperdeviation in primary position that worsens on left gaze and left head tilt.
42. A 35-year-old Chinese man presents with right ptosis and an abduction deficit, facial hypesthe-sia, and keratoconjunctivitis sicca in the right eye. This scenario is highly suggestive of
a. meningioma.
b. diabetic vascular neuropathies.
c. nasopharyngeal carcinoma.
d. aneurysm.
43. The most common cause of isolated sixth nerve palsy is
a. raised intracranial pressure.
b. ischemia.
c. tumor.
d. aneurysm.
44. A 62-year-old female complains of diplopia lasting typically 30 to 60 seconds. The patient has had previous radiation therapy for a cranial meningioma. In the office, the patient has full motility, but you notice the patient has an episode in which the left eye abducts for 30 seconds. The most likely diagnosis is
a. neuromyotonia.
b. intermittent exotropia.
c. third nerve palsy.
d. sixth nerve palsy.
45. A 77-year-old patient with end-stage glaucoma with count fingers vision in both eyes states that he sees what appears to be little green men walking around his house. He knows that these images are not real. What is the most likely diagnosis?
a. schizophrenia.
b. Anton’s syndrome.
c. Charles Bonnet’s syndrome.
d. visual allesthesia.
46. A 69-year-old female was found to have an intra-cranial neoplasm on MRI after complaining of severe headaches. The patient has miosis of his left eye and is unable to abduct that eye. The neoplasm is most likely found in the
a. cerebellopontine angle.
b. left cavernous sinus.
c. superior orbital fissure.
d. petrous bone.
47. A 72-year-old female presents with normal visual acuity, diminished corneal sensation, and global impairment of ocular motility of the right eye. The patient also has a severe boring headache. The MRI shows an enhancing mass within the right cavernous sinus. The pain and ophthalmoplegia respond dramatically to corticosteroid therapy. The most likely diagnosis is
a. carotid cavernous sinus fistula.
b. meningioma of the cavernous sinus.
c. internal carotid aneurysm.
d. Tolosa-Hunt syndrome.
48. The finding that all three types of Duane’s syndrome share is
a. a deficit of abduction.
b. a deficit of adduction.
c. globe retraction with adduction.
d. esotropia.
49. Which one of the following concerning oculomotor apraxia is false?
a. Pursuits are generally affected more than saccades.
b. Horizontal movements are generally affected much more than vertical movements.
c. In the acquired form, blinks are frequently used to break fixation.
d. In the congenital form, children frequently use compensatory exaggerated head turns to refixate.
50. The saccadic movement that is often affected in progressive supranuclear palsy (PSP) is
a. upward.
b. downward.
c. leftward.
d. rightward.
51. Hypertropia associated with ipsilateral adduction weakness is most suggestive of
a. decompensated congenital fourth nerve palsy.
b. dorsal midbrain syndrome.
c. “One-and-a-half ” syndrome.
d. skew deviation with internuclear ophthalmoplegia (INO).
52. The dorsal midbrain syndrome is associated with all of the following except
a. upward gaze paresis.
b. paradoxic OKN.
c. light-near dissociation.
d. lid retraction.
53. Which of the following would not normally be found in congenital nystagmus?
a. oscillopsia.
b. amplitude increased by distance fixation.
c. paradoxic OKN.
d. amplitude dampened by convergence.
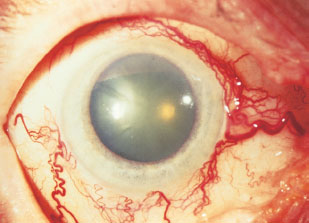
54. A 43-year-old man presents complaining of persistent red eye in the right eye (seen in the image below), present ever since a car accident 6 weeks earlier. Besides redness, he has noted intermittent horizontal diplopia without pain. The results of his examination are normal, except for 4 mm of proptosis on the right, a mild deficit in abduction, and prominent conjunctival vessels. His left eye is entirely normal. What is the most likely diagnosis?
a. carotid cavernous sinus fistula.
b. dural sinus fistula.
c. cavernous sinus thrombosis.
d. viral conjunctivitis.
55. Which of the following ocular motor disorders is most associated with malignancy?
a. square-wave jerks.
b. opsoclonus.
c. dysmetria.
d. ocular bobbing.
56. Monocular nystagmus in a toddler raises the specter of
a. optic nerve meningioma.
b. craniopharyngioma.
c. rhabdomyosarcoma.
d. chiasmal glioma.
57. According to Alexander’s law, in which position should upbeat nystagmus be most prominent?
a. upgaze.
b. downgaze.
c. left gaze.
d. right gaze.
58. Which pattern of nystagmus is most commonly found in patients with large tumors in the para-sellar region?
a. upbeat nystagmus.
b. vestibular nystagmus.
c. downbeat nystagmus.
d. see-saw nystagmus.
59. Which visual field defect is most likely to be associated with see-saw nystagmus?
a. central scotoma.
b. bitemporal hemianopia.
c. incongruous hemianopia.
d. congruous hemianopia.
60. Which of the following eye movements is not matched correctly with its corresponding site of origin?
a. Vestibular ocular reflex—Brainstem.
b. Saccades—Contralateral frontal lobe.
c. Pursuit—Ipsilateral parietal lobe.
d. Vergence—Brainstem.
61. Which one of the following concerning the facial nerve is false?
a. The sensory innervation of the anterior twothirds of the tongue terminates in the nucleus solitarius, and the motor innervation to the lacrimal gland arises, in part, from the superior salivatory nucleus.
b. The first branch of the facial nerve is the greater superficial petrosal nerve, which synapses in the geniculate ganglion.
c. Within the fallopian canal, the facial nerve gives off a motor branch to the stapedius muscle and sensory branches for the skin behind the ear.
d. Nerves from the chorda tympani synapse in the geniculate ganglion, carrying sensory innervation to the tongue and motor innovation to the salivary glands.
62. Which of the following concerning Marcus Gun jaw-winking syndrome is false?
a. It is an example of aberrant regeneration.
b. The patient can present with ptosis.
c. The eyelid can elevate upon opening of the mouth.
d. It is a synkinetic movement of the eyelid associated with jaw movement.
63. A 26-year-old female presents to your office with blurred vision for 3 days in her left eye. Fundus examination reveals disc edema with a macular star. She has no medical problems including diabetes or hypertension. You astutely diagnose her has having neuroretinitis. What is the most likely cause?
a. underlying hypertension.
b. underlying diabetes.
c. Bartonella henselae.
d. multiple sclerosis.
64. Which of the following cranial nerves is most frequently involved cranial nerve in sarcoidosis?
a. CN II.
b. CN III.
c. CN VII.
d. CN VIII.
65. Which of the following is true regarding hemifacial spasm?
a. It is bilateral.
b. Most commonly occurs because of compression of the seventh nerve root by an aberrant vessel.
c. Functional neuroimaging suggests that it may be caused by basal ganglia dysfunction.
d. It is a benign condition, so neuroimaging is not needed once it is diagnosed.
66. Facial myokymia in a child is frequently associated with
a. chiasmal glioma.
b. spasmus nutans.
c. cerebellar hemangioblastoma.
d. pontine glioma.
67. Which of the following is false regarding essential blepharospasm?
a. Onset typically occurs after age 65.
b. Causes of reflex blepharospasm, for example, dry eyes or ocular irritation should be ruled out.
c. It is a bilateral condition.
d. Treatment of choice is injection of botulinum toxin into the orbicularis muscle.
68. Which of the following regarding the pupillary reflex is true?
a. The pupil pathway terminates in pretectal nuclei after passing, without synapsing, through the lateral geniculate body (LGB).
b. The decussation at the chiasm is responsible for a normal consensual pupillary response.
c. Sympathetic pupillary fibers originate in the superior cervical ganglion, travel in the cranial vault with the internal carotid artery, and enter the orbit with the ophthalmic artery through the optic foramen.
d. The pathway for accommodative miosis enters the Edinger-Westphal nucleus anterior to the pathway for light-induced miosis.
69. Which of the following statements concerning these conditions with light-near dissociation is true?
a. A key finding in the diagnosis of Argyll Robertson pupils is the presence of mydriasis.
b. Argyll Robertson pupils react to light, but do not have a near response.
c. The most common etiology of the dorsal midbrain syndrome in a child under 10 years of age is a pineal gland tumor.
d. The most common etiology for the dorsal midbrain syndrome in a patient over the age of 60 is multiple sclerosis (MS).
70. Which one of the following concerning Adie’s tonic pupil is false?
a. The majority of affected patients will have unilateral involvement.
b. Patients may have accommodative symptoms or photophobia.
c. Pupillary constriction in response to pilocarpine 1% is conclusive evidence of denervation hypersensitivity.
d. The differential diagnosis of a tonic pupil includes herpes zoster, syphilis, and giant cell arteritis.
71. Which of the following concerning Horner’s syndrome is true?
a. The distribution of anhidrosis does not help in localizing the lesion.
b. Cocaine 4% will dilate the pupil of the patient with Horner’s syndrome, whereas it will leave a normal pupil unchanged.
c. The evaluation of a patient whose miotic pupil does not dilate with topical cocaine, but does dilate with topical hydroxyamphetamine consists, in part, of chest x-ray and careful neurologic examination.
d. Horner’s syndrome with coincident ipsilateral headache is benign and requires no further neuroimaging.
72. Which of the following statements regarding the condition shown below is false?
a. The successful use of photodynamic therapy (PDT) to treat this condition has been reported.
b. Vitreous hemorrhage can occur spontaneously in this condition.
c. Patients with no other medical history presenting with a similar fundus should undergo neuroimaging.
d. An orbital bruit can be heard in patients with this condition.
73. Which of the following statements regarding the condition shown below is false?
a. The condition is unilateral.
b. Retinal vessels originating from the periphery of the disc is a classic finding.
c. Visual acuity is often good.
d. The patient may have an RAPD.
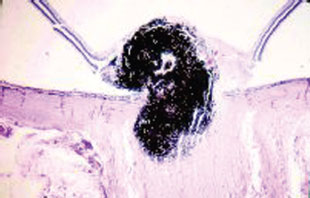
74. A patient with the lesion shown in the pathology slide below most likely has
a. choroidal melanoma.
b. medulloepithelioma.
c. congenital hypertrophy of the retinal pigment epithelium.
d. melanocytoma.
75. Pheochromocytoma may be seen in patients with
a. Sturge-Weber syndrome.
b. tuberous sclerosis.
c. von Hippel-Lindau disease.
d. ataxia–telangiectasia.
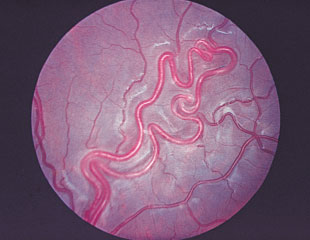
76. A 23-year-old male was found to have to have the retinal abnormality found below. This is a
a. retinal cavernous hemangioma.
b. racemose angioma.
c. retinal capillary hemangioma.
d. astrocytic hamartoma.
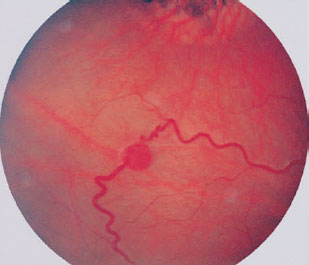
77. The lesion above is associated with which phakomatoses?
a. Sturge-Weber syndrome.
b. von Hippel-Lindau disease.
c. tuberous sclerosis.
d. ataxia–telangiectasia.
78. The next step following examination of the patient in question 76 would be
a. observation.
b. radiation therapy.
c. prompt referral of the patient for a thorough systemic investigation.
d. prescription of epileptic medications.
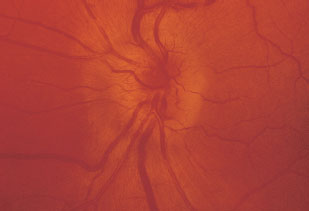
79. A 42-year-old male’s retinal findings are seen at the top of the next page. What is the diagnosis?
a. retinal cavernous hemangioma.
b. racemose angioma.
c. retinal capillary hemangioma.
d. astrocytic hamartoma.

80. The lesion shown in question 79 is more commonly associated with which phakomatoses?
a. Sturge-Weber syndrome.
b. von Hippel-Lindau disease.
c. tuberous sclerosis.
d. ataxia–telangiectasia.
81. The next step following examination of the patient in question 79 would be
a. observation.
b. laser therapy.
c. I-125 plaque therapy.
d. chemotherapy.
82. Glaucoma is associated with which phakomatoses?
a. von Hippel-Lindau disease.
b. tuberous sclerosis.
c. Sturge-Weber syndrome.
d. ataxia–telangiectasia.
83. Chronic sinopulmonary infections may be seen as part of
a. neurofibromatosis.
b. tuberous sclerosis.
c. angiomatosis retinae.
d. ataxia–telangiectasia.
84. All of the following can have chronic progressive external ophthalmoplegia (CPEO) except
a. myotonic dystrophy.
b. oculopharyngeal dystrophy.
c. thyroid eye disease.
d. Kearns-Sayre syndrome.
85. Which one of the following concerning Kearns-Sayre syndrome is false?
a. The complete syndrome has an onset of symptoms or signs before age 20 years.
b. The pigmentary retinopathy is generally associated with good visual function throughout life.
c. The progressive external ophthalmoplegia associated with the syndrome typically presents as diplopia.
d. Heart block develops late in the course of the syndrome.
86. Which of the following statements is false regarding monocular diplopia?
a. There are no genetic syndromes associated with monocular diplopia.
b. It can be caused by retinal pathologies.
c. It can be caused by lenticonus.
d. It can be caused by high astigmatism.
87. The most common sign of Graves’ ophthalmopathy is
a. lid retraction.
b. conjunctival injection over the horizontal rectus muscles.
c. esotropia.
d. proptosis.
88. The most frequently involved extraocular muscle in Graves’ ophthalmopathy is the
a. inferior rectus.
b. lateral rectus.
c. superior rectus.
d. medial rectus.
89. A patient with a history of bilateral occipital lobe infarcts adamantly states that he can see quite well and confabulates visual images. He most likely suffers from
a. Anton’s syndrome.
b. palinopsia.
c. Charles Bonnet’s syndrome.
d. blindsight.

90. What percentage of patients with myasthenia gravis (MG) present with ocular findings only?
a. 10%.
b. 25%.
c. 50%.
d. 75%.
91. What percentage of patients with myasthenia gravis will develop Graves’ disease?
a. 5%.
b. 10%.
c. 15%.
d. 20%.
92. What percentage of patients with myasthenia gravis have thymomas visible on CT?
a. 1%.
b. 10%.
c. 25%.
d. 50%.
93. For a patient to be reassured that systemic disease is unlikely, ocular myasthenia should remain localized for what length of time?
a. 6 months.
b. 1 year.
c. 2 years.
d. 5 years.
94. Animal studies show that irreversible ischemic retinal damage occurs after what duration of retinal vascular occlusion?
a. 30 minutes.
b. 90 to 100 minutes.
c. 3 hours.
d. 6 hours.
95. Typical symptoms in vertebrobasilar insuffi-ciency include all of the following except
a. ataxia.
b. hemiparesis.
c. vertigo.
d. monocular blurring or loss of vision.
96. A 29-year-old woman presents to an ophthalmologist complaining of pain on eye movements and blurry vision in her right eye. Review of systems documents a 3-week history of paresthesias in the right lower leg approximately 6 months prior to the onset of her visual disturbance. The patient reports that she noticed her visual disturbance develop over the 2 or 3 days prior to presentation. Examination discloses a visual acuity of 20/60 in the right eye and 20/20 in the left eye. She is able to interpret correctly 4 of 11 Ishihara plates with her right eye and 10 of 11 plates with her left eye. Visual fields disclose a central scotoma in the right eye and are normal for the left eye. There is no afferent pupillary defect (APD) noted. Which one of the following is most likely true?
a. The patient probably has an acute maculopathy.
b. The patient probably has factitious visual loss.
c. The patient probably had a similar episode affect her left eye sometime in the past.
d. Oral steroid therapy is indicated.
97. Which of the following diseases have been observed in association with Coats’ disease?
a. facioscapulohumeral muscular dystrophy.
b. myotonic dystrophy.
c. cerebral angiitis.
d. chronic progressive external ophthalmoplegia.
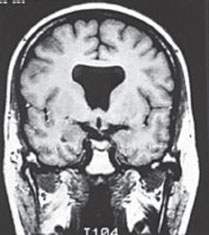
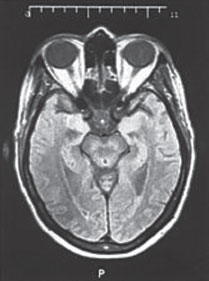
98. A 14-year-old girl is brought to the ophthalmologist by her parents after complaining that ”the page swims when I try to read.” The examination is normal with the exception of pronounced downbeat nystagmus. A careful review of systems documents the presence of intermittent headaches in the occipital region, which are intensified with anger or sudden head movement. The patient denies any use of prescription or illicit drugs, including alcohol. Which of the following CT scans (in the left column at the top of the next page) is most likely depicts her condition?
99. Modalities likely to relieve the patient’s reading difficulties successfully include
a. clonazepam (Klonopin).
b. carbamazepine (Tegretol).
c. bifocals.
d. psychotherapy.
100. A 9-year-old boy presents to the ophthalmologist complaining that he has lost his position on the school basketball team because he cannot see the basket. He notes occasional morning headaches but denies any nausea or vomiting. Examination reveals visual acuity of 20/40 in the right eye and 20/25 in the left eye. The patient has marked symmetric weakness of upgaze bilaterally. His pupils are 7 mm and poorly reactive to light with better reaction to a near target. There is approximately 2 mm of superior scleral show bilaterally. Fundus examination suggests optic atrophy in both eyes. Review of systems documents increased consumption of water with frequent urination at night. The most likely diagnosis is
a. pinealoma.
b. cerebellar astrocytoma.
c. chiasmal glioma.
d. hereditary optic atrophy.
101. After neuroimaging, an important step in diagnostic evaluation of the patient in question 100 would be
a. visual evoked responses (VERs).
b. EEG.
c. Farnsworth D-15 color vision testing.
d. lumbar puncture.
102. Which of the following concerning optic neuritis in childhood is true?
a. It is more commonly bilateral than unilateral.
b. The visual prognosis is almost always very poor.
c. The pathophysiology is believed to be ischemia of the optic nerve.
d. Enlargement of optic nerves on neuroimaging implies another, more ominous, diagnosis.
103. Posterior ischemic optic neuropathy (PION) typically occurs in what setting?
a. post radiation therapy.
b. post spinal surgery.
c. 1 to 2 weeks after viral infection.
d. raised intracranial pressure.
104. In a patient complaining of headache and transient visual obscurations whose examination reveals bilateral disc edema, the first diagnostic intervention to be undertaken is
a. lumbar puncture.
b. measurement of sedimentation rate.
c. CT scanning.
d. measurement of blood pressure.
105. Which of the following disorders is clearly associated with optic nerve drusen?
a. migraines.
b. pseudotumor cerebri.
c. giant cell arteritis.
d. retinitis pigmentosa.
106. Which histopathologic variety of meningioma is most commonly seen within the orbit?
a. angioblastic.
b. meningothelial.
c. fibroblastic.
d. pilocytic.
107. Optociliary shunt vessels are most commonly seen in what condition?
a. optic nerve sheath meningioma.
b. optic glioma.
c. carotid occlusive disease.
d. central retinal artery occlusion.
108. Important blood tests in the evaluation of patient with bilateral optic atrophy and cecocentral scotomas include all of the following except
a. serum B12 level.
b. fluorescent treponemal antibody-absorption test (FTA-Abs).
c. serum folate level.
d. serum cyanide level.
109. A 58-year-old gentleman appears in your office with bilateral blurry vision. He appears disheveled and gaunt. He has been unemployed for 1 year and smells of alcohol. The patient’s visual acuity was 20/200 in both eyes with no RAPD. Images A and B at the top of the right column are the patient’s visual fields. What is the most likely diagnosis?
a. NAION.
b. dominant optic atrophy.

c. toxic/nutritional optic neuropathy.
d. nonorganic vision loss.
110. The most common fundus finding in a patient with acute traumatic optic neuropathy is
a. disc edema.
b. disc pallor.
c. choroidal ruptures.
d. unremarkable fundus.
111. Which of the following concerning diabetic papillopathy is true?
a. It is typically painful.
b. Development of the disorder seems to be independent of the degree of blood sugar control.
c. The papillopathy is generally followed by the development of florid neovascularization.
d. Visual loss is generally severe.
112. Modalities useful in the treatment of optic neuropathy secondary to thyroid eye disease include all of the following except
a. subtotal thyroidectomy.
b. orbital radiation.
c. corticosteroid therapy.
d. orbital decompression surgery.
113. Bromocriptine treatment may be indicated in the management of a patient with a pituitary tumor that is secreting
a. prolactin.
b. growth hormone.
c. thyrotropin.
d. nonsecreting.
114. The development of sudden severe headache with accompanying acute visual loss is a well-recognized complication of
a. meningioma.
b. intracavernous carotid artery aneurysm.
c. pituitary adenoma.
d. hypothalamic glioma.
115. Which one of the following nerves supplies the cornea?
a. frontal nerve.
b. lacrimal nerve.
c. nasociliary nerve.
d. supraorbital nerve.
116. Which feature is necessary to conclude a motility disturbance is a skew deviation?
a. a horizontal component.
b. comitance in all gaze directions.
c. pattern of motility inconsistent with a single muscle or nerve dysfunction.
d. other obvious brainstem abnormalities.
117. Brainstem nuclei critical for the generation of normal vertical eye movements includes which of the following?
a. paramedian pontine reticular formation.
b. the rostral interstitial nucleus of the medial longitudinal fasciculus.
c. the abducens nucleus.
d. the inferior olivary nucleus.
118. What finding in a child with isolated abduction deficit most strongly argues for the diagnosis of Duane’s retraction syndrome rather than congenital sixth nerve palsy?
a. inability to fully abduct the eye volitionally.
b. involvement of the left eye.
c. orthotropia in primary gaze.
d. normal adduction.
119. Which of the following features is found in all cases of internuclear ophthalmoplegia (INO)?
a. ipsilateral adduction slowing or weakness.
b. exotropia.
c. contralateral adduction nystagmus.
d. skew deviation.
120. A feature frequently found coincidentally with bilateral internuclear ophthalmoplegia (INO) is
a. rotary nystagmus.
b. vertical nystagmus.
c. convergence–retraction nystagmus.
d. see-saw nystagmus.
121. A brainstem lesion that involves the medial longitudinal fasciculus as well as the ipsilateral abducens nucleus will most likely cause
a. internuclear ophthalmoplegia with skew.
b. Foville’s syndrome.
c. Walleyed bilateral internuclear ophthalmoplegia (WEBINO).
d. “One-and-a-half” syndrome.
122. A lesion that involves both medial longitudinal fasciculi near their junctions with the third nerve nuclei may cause
a. “One-and-a-half” syndrome.
b. Walleyed bilateral internuclear ophthalmoplegia (WEBINO).
c. Fisher’s syndrome.
d. internuclear ophthalmoplegia with skew.
123. A variant of Guillain-Barré syndrome that only involves only the brainstem and cranial nerves is known as
a. internuclear ophthalmoplegia skew.
b. Foville’s syndrome.
c. Miller-Fisher syndrome.
d. “One-and-a-half” syndrome.
124. The clinical distinction between a cavernous sinus syndrome and an orbital apex syndrome is best made by the dysfunction of which cranial nerve?
a. CN II.
b. CN III.
c. CN V.
d. CN VI.
125. Potential complications of carotid-cavernous fistulae include all of the following except
a. retinal neovascularization.
b. retinal vasculitis.
c. glaucomatous optic nerve damage.
d. corneal ulceration.
126. A 59-year-old man presents to the emergency room complaining of sudden-onset oscillopsia and diplopia. Examination reveals an alcohol smell on his breath, normal acuity, bilateral abduction deficits, and coarse binocular nystagmus. Appropriate intervention should include
a. intravenous glucose.
b. intravenous naloxone.
c. intravenous chlordiazepoxide.
d. intravenous thiamine.
127. Which of the following optic disc lesions are distinguished by autofluorescence?
a. myelinated nerve fibers.
b. optic nerve neovascularization.
c. optic nerve pits.
d. astrocytic hamartoma.
128. The approximate prevalence of giant cell arteritis in Scandinavians is one in
a. 10.
b. 100.
c. 1,000.
d. 10,000.
129. The approximate prevalence of polymyalgia rheumatica (PMR) in the population over the age of 50 is one in
a. 20.
b. 200.
c. 2,000.
d. 20,000.
130. Clinical characteristics that may be seen with chiasmal compression include all of the following except
a. congruous homonymous hemifield defect.
b. postfixation blindness.
c. temporal color desaturation.
d. diplopia.
131. Afferent pupillary fibers from the optic tract exit at
a. the lateral geniculate body.
b. the pretectal olivary nuclei.
c. the occipital cortex.
d. the medial longitudinal fasciculus.
132. A woman with known multiple sclerosis (MS) presents to an ophthalmologist complaining of ”a tiny blind spot in my right eye.” Examination discloses a right afferent pupillary defect and slight ocular tenderness in the right eye. The examiner attempts to confirm diagnostic suspicions by eliciting the Pulfrich phenomenon. To do this, the examiner
a. asks the patient to glance quickly back and forth horizontally and report any photopsias.
b. asks the patient to climb briskly several flights of stairs and report any visual loss.
c. asks the patient to watch the pendulum on the grandfather clock across the room and report any three-dimensional movement.
d. spins the examining chair while the patient fixates her outstretched thumb, watching for any nystagmus.
133. The test that best correlates with the pathophysiology underlying the Pulfrich phenomenon is
a. electrooculography (EOG).
b. visual evoked response (VER).
c. electroretinography (ERG).
d. calorics and electronystagmography.
134. A 23-year-old male presents to his ophthalmologist complaining that colors do not seem as bright as they used to appear. His acuities are 20/20 in the right eye and 20/200 in the left eye. He is able to name 10 of 12 color plates correctly with the right eye, but only one of 12 with the left. Visual fields show a cecocentral scotoma in the left eye only. His color photo of his left optic nerve is shown below. A fluorescein angiogram did not show any leakage or staining of his left optic nerve. Which of the following is not true?
a. The right eye is likely to be similarly affected within the next several months.
b. Diagnostic evaluation must include electrocardiography.
c. He should be counseled to avoid tobacco and heavy alcohol consumption.
d. He should be counseled to expect no improvement in the left eye over time.
135. Each of the following regarding the disorder in question 134 is true, except
a. The patient’s brothers are more likely to be similarly affected than his sisters.
b. Other than siblings, similarly affected family members are far more likely to be maternally related than paternally related.
c. The disease is frequently associated with abnormalities of the X chromosome.
d. Unfortunately, no specific test exists to confirm the suspected diagnosis.
136. A 42-year-old woman presents to her ophthalmologist complaining of double vision. Her eye movements are shown in the figures below (images A-D). Figure A shows her in primary position. Figure B shows her immediately after being requested to look to her right. Figure C shows her immediately after being asked to look to her left. Figure D shows her approximately 10 to 15 seconds after being requested to look to her left. Each of the following is true regarding her case except
a. She may have intermittent nystagmus.
b. The responsible lesion is on the left side of her brainstem.
c. There may be a history of recent closed head trauma.
d. The right eye may adduct normally with convergence.
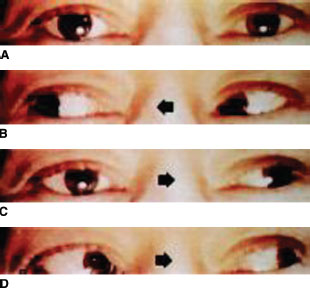
137. The patient in question 136 may demonstrate nystagmus while looking in which field of gaze, as depicted by the figures in that question?
a. Figure A.
b. Figure B.
c. Figure C.
d. The patient will have nystagmus in all of the above fields.
138. A 63-year-old man presents with the pupillary findings shown in Figure A (below). Figure B shows his pupils after bilateral installation of 4% cocaine. Figure C shows his pupils after bilateral installation of 1% hydroxyamphetamine. Each of the following regarding his situation is true except:
a. His anisocoria is worse in low ambient illumination.
b. No workup is necessary if the findings can be shown to be longstanding.
c. Associated findings might include unilateral hypotony or a mild anterior chamber reaction.
d. One potential etiology might be occult lung cancer.
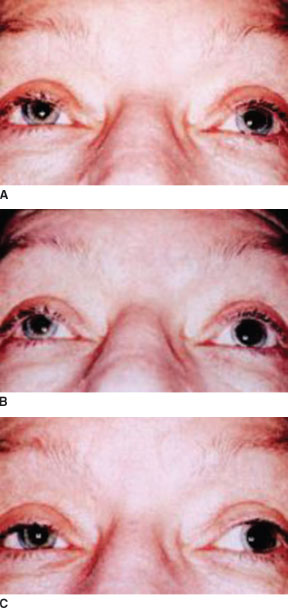
139. If the patient in question 138 presents with acute headache, the workup must include urgent
a. cranial MRI.
b. carotid angiography.
c. lumbar puncture.
d. chest CT.
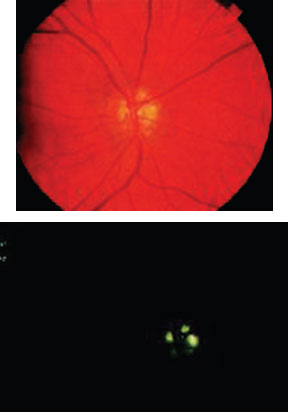
140. A 23-year-old obese woman is seen for routine ophthalmologic examination. The examination is entirely normal with the exception of bilaterally elevated discs with indistinct margins. The right optic nerve is shown in the color photo below (top). The second figure (bottom of page) is a preinjection photo from fluorescein angiography. Which one of the following regarding this patient is true?
a. The condition depicted is typically associated with mild to moderate visual loss.
b. There may be an associated arcuate field defect.
c. The clinical and histologic findings reflect axoplasmic stasis and congestion.
d. The filters on the fluorescein camera are of poor quality.
141. Select the CT scan that is most likely to create the visual field disturbance shown in the figures below.
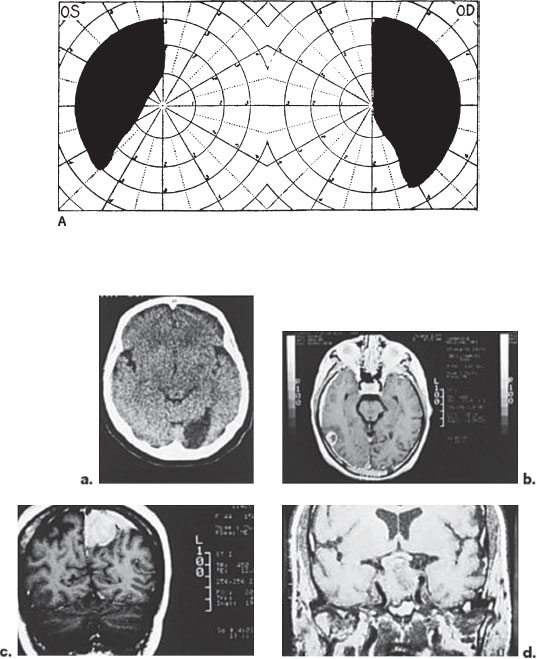
142. Which one of the following abnormalities might be expected in a young child with bilaterally poor vision and the CT scan shown below?
a. precocious puberty.
b. ash-leaf macules.
c. panhypopituitarism.
d. pheochromocytoma.
143. A unilateral brainstem lesion at the level of the central nervous system shown below is most likely to produce which one of the following neurologic deficits?
a. corneal hypesthesia.
b. third nerve palsy and contralateral hemiplegia.
c. combined abducens and facial palsies.
d. “One-and-a-half” syndrome.
144. Which of the following would be the best choice for treatment of acute, severe migraine headache?
a. sumatriptan.
b. acetaminophen.
c. methysergide.
d. propranolol.
145. Which of the following would be the best initial choice for prophylaxis of acute, severe migraine headache?
a. sumatriptan.
b. acetaminophen.
c. methysergide.
d. propranolol.
146. Which one of the following regarding the Ischemic Optic Neuropathy Decompression Trial (IONDT) is false?
a. Spontaneous improvement of vision was seen in over 40% of control (nonsurgical) cases.
b. Patients in both the surgical and the nonsurgical groups were equally likely to gain three or more lines of visual acuity.
c. Patients in both the surgical and the nonsurgical groups were equally likely to lose three or more lines of visual acuity.
d. The study represented the first randomized controlled prospective clinical trial of optic nerve sheath decompression (ONSD) for AION.
147. Which one of the following regarding pseudotumor cerebri is true?
a. Headache is the sine qua non of the disease (i.e., it is a universal symptom among patients with the disorder).
b. Neurologic abnormalities, including abducens palsy, are common.
c. Opening pressure and CSF protein levels are typically elevated.
d. Many cases are probably on the basis of decreased reabsorption of CSF.
148. Which one of the following autoantibodies are most commonly found in patients with generalized myasthenia gravis (MG)?
a. binding antibodies to acetylcholine receptors.
b. blocking antibodies to acetylcholinesterase.
c. blocking antibodies to acetylcholine receptors.
d. blocking antibodies to acetylcholine.
149. Relative to generalized myasthenia, ocular myasthenia is
a. more commonly associated with Graves’ disease.
b. more responsive to anticholinesterase drugs.
c. more responsive to steroids.
d. completely localized to ocular or bulbar involvement.
150. Which of the following medications is most clearly associated with drug-induced myasthenia?
a. warfarin.
b. D-penicillamine.
c. diltiazem.
d. ranitidine.
1. d. Although optokinetic nystagmus, the rocking mirror test, and the base-up prism test can help discover factitious monocular blindness, they are not sensitive enough to diagnose factitious visual deficit at the 20/100 level. For such mild visual deficits, a fogging refraction, stereo acuity, and red–green glasses may be useful in diagnosing factitious visual loss.
2. d. A pattern VER (as opposed to a flash VER) is required for visual acuity assessment in preverbal children. Although the VER is useful in establishing factitious visual loss, its reliability is limited by the fact that patients can produce false readings by using accommodation to fog their vision. Abnormalities in VER latency and amplitude have been reported in various maculopathies and retinopathies and thus cannot distinguish optic neuropathy from retinal disorders with complete reliability.
3. b. Cancer-associated retinopathy (CAR) presents with photopsias, nyctalopia, impaired dark adaptation, dimming, ring scotoma, and peripheral or central visual field loss. The underlying malignancy is usually small cell carcinoma of the lung, although other lung tumors and breast, uterine, and cervical malignancies have been reported. ERG is typically markedly reduced in amplitude. Deterioration is progressive, with eventual bilateral involvement and severe visual loss. The retinal arterioles become attenuated, the RPE thinned and mottled, and the optic discs atrophic.
4. a. Melanoma-associated retinopathy (MAR) is an extremely rare syndrome that primarily involves rods. Symptoms include photopsia, nyctalopia, and bilateral peripheral visual loss. Visual symptoms typically develop in the setting of previously diagnosed melanoma, and investigation of visual loss often reveals metastasis. The fundus may be normal, or may show RPE irregularity, retinal arteriolar attenuation, and optic disc pallor. There is no treatment that has been proven effective.
5. b. MRI is based on applying a radiofrequency pulse to tissue within a strong magnetic field and measuring the change in tissue’s nuclear spin and magnetic vector. The longitudinal relaxation time is termed T1. Fat is bright and water is dark on T1-weighted images. In contrast, fat is dark, and water is bright on T2-weighted images. Some tissues such as cortical bone, rapidly flowing fluid (blood), and air give no signal at all on MRI. T1-weighted images are optimal for demonstrating anatomy. T2-weighted images maximize the differences in tissue water content and state. Therefore, T2-weighted images are the most sensitive to inflammatory, ischemic, or neoplastic alterations in tissue.
6. c. Although there is some redundancy of the optic nerve within the orbit, the intracranial optic nerve has little “slack.” The dimensional characteristics of the optic nerve can be remembered with the mnemonic phone number 125-1017, which stands for the lengths of the intraocular (1), intraorbital (25), intracanalicular (10), and intracranial (17) portions of the optic nerve.
7. b. Fifty-three percent of the retinal ganglion cells cross in the chiasm (this difference is occasionally important clinically). The macular fibers constitute a large portion of the optic chiasm and most decussate in the posterior chiasm. The chiasm lies approximately 1 cm (not 1 mm) above the anterior pituitary gland. The inferior nasal retinal fibers cross in the anterior chiasm and were thought to loop anteriorly in the contralateral optic nerve before traveling posteriorly—leading to the term Wilbrand’s knee. It is now thought that Wilbrand’s knee may be an artifact.
8. d. The temporal 30° of a binocular visual field is perceived by the nasal-most retina of the ipsi-lateral eye only. These “temporal crescents” are represented in the most anterior portion of the occipital lobe. Thus, a lesion in this area will produce a monocular visual field defect in the far temporal periphery of the contralateral eye, the so-called temporal crescent syndrome. For example, a right anterior occipital lobe lesion would produce a far temporal field defect in the left eye. Similarly, a right posterior occipital lobe lesion may spare the far temporal field in the left eye.
9. c. The retinal ganglion cell terminals are segregated by eye. The ipsilateral ganglion cells synapse in layers 2, 3, and 5, whereas the contralateral ganglion cells synapse in layers 1, 4, and 6.
10. c. OKN abnormalities indicate lesions of the parietooccipital (slow-phase pursuit abnormalities) or the frontal lobe (fast-phase recovery abnormalities). High congruity of visual field deficits indicates a lesion in the occipital lobe. Formed visual hallucinations, partial complex seizures, and olfactory hallucinations may be seen with temporal lobe lesions. Unformed hallucinations are common with disorders of the occipital lobe. Inferior nerve fibers from the superior retina course anteriorly in Meyer’s loop; thus lesions affecting Meyer’s loop will result in pie-in-the-sky defects contralateral to the lesion.
11. d. Parietal lobe lesions are associated with agnosia and right–left confusion. A parietal lobe lesion will also affect slow-phase pursuit movements toward the ipsilateral side. Unlike temporal lobe lesions, which produce hemianopias that are denser superiorly, parietal lobe lesions produce hemianopias that are denser inferiorly.
12. a. Formed hallucinations occur with temporal lobe pathology. Depending on the location of the occipital lobe lesion, the temporal crescent, the representation of which is located in the most anterior visual cortex, may be either spared (more common) or affected. Although OKN asymmetry may rarely occur with occipital lesions, this finding is generally indicative of a parietal locus of disease.
13. c. Key events in the development of true disc edema include cessation of axonal transport with swelling of axons. The increase in disc volume is due to enlargement of axons, rather than increased extracellular fluid, as seen in edema of other tissues. Breakdown of the blood–retinal barrier does occur, detected as leakage on fluorescein angiography, but this is not important in the development of disc edema.
14. b. Although loss of spontaneous venous pulsations is an early sign of papilledema, remember that about 20% of normal patients lack venous pulsations. Transient obscurations of vision (TOV) often accompany papilledema and are episodes of unilateral or bilateral visual loss lasting only a few seconds. The most typical visual field finding in acute papilledema is an enlarged blind spot. Although rare, unilateral papilledema may occur. For example, if contralateral optic atrophy exists, papilledema may be detectable only in the viable disc.
15. d. Pseudotumor cerebri is characterized by increased intracranial pressure on lumbar puncture, normal neuroimaging studies (although the ventricles may be small), and normal cerebrospinal fluid (CSF). Papilledema need not be present for the diagnosis. Although the neurologic examination is usually normal, sixth nerve palsy may occur with increased intracranial pressure of any etiology.
16. c. Obesity is not an indication for treatment, although weight loss (even as little as 6% of total body weight) often improves the condition. Most cases of pseudopapilledema are due to the presence of optic disc drusen.
17. a. Acetylsalicylic acid or aspirin is not associated with pseudotumor cerebri. Pseudotumor cerebri can be associated with the use of vitamin A, tetracycline, nalidixic acid, cyclosporine, oral contraceptives, as well as the use of or withdrawal from corticosteroids.
18. c. Studies have documented that up to 80% with cavernous sinus–dural fistulae will develop ocular hypertension. Twenty-five percent will develop optic disc cupping and 20% visual field defects. Any entity that raises episcleral venous pressure can cause secondary open-angle glaucoma.
19. d. Visual loss is typically severe. Visual acuity is less than 20/200 in over 60% of patients.
20. b. The most likely diagnosis in this vaculopathic patient is NAION. Risk factors for NAION include hypertension, diabetes, smoking, hyperlipidemia, and crowding of the contralateral disc (“Disc at risk”). Altitudinal visual field loss is also more common in patients with NAION.
21. c. NAION is far more common than AAION, approximately 95% vs. 5%, and patients have a lower mean age at diagnosis than patients with AAION, 60 years versus 70 years. It usually occurs in a younger age group, and may resemble optic neuritis. Ways to differentiate NAION from optic neuritis include (a) lack of pain with eye movement; (b) the age group affected; (c) delayed optic disc filling present in 75% of NAION cases (whereas filling should be normal in optic neuritis). The role of aspirin in reducing the incidence of fellow eye involvement after the initial episode is unclear.
22. a. There is no proven therapy for NAION.
23. d. The 15-year data from the optic neuritis treatment trial (ONTT) demonstrate a risk for MS of 25% in patients with zero lesions on MRI versus 72% with at least one lesion, with the highest rate of conversion within the first 5 years. Visual recovery to a level of 20/40 or better occurs in 92% of patients with optic neuritis.
24. d. In a retrospective review of autopsy findings, nearly 100% of patients dying of MS had some degree of optic nerve demyelination.
25. a. Ninety percent of optic gliomas occur in the first two decades of life. The most common presenting findings are proptosis, visual loss, optic disc pallor, disc edema, and strabismus. The number of patients with optic nerve glioma that have associated neurofibromatosis (NF-1) ranges from 14% to 60%. Optociliary shunt vessels are less commonly seen with optic gliomas than with optic nerve meningiomas. Malignant gliomas of the visual pathways, although rare, occur more frequently in middle-aged adults than in children. Survival averages 6 to 12 months after diagnosis.
26. d. In contrast to optic nerve gliomas, meningiomas occur primarily in adults, and are three times more common in women. Although persons with NF-1 have a higher incidence of meningiomas than the general population, only a minority of people with meningiomas have NF-1. With contrast CT scanning, the peripheral part of the involved optic nerve may show enhancement, resulting in the “railroad track” or “tram track” sign. “Kinking” is specific for optic nerve glioma.
27. b. Dominant (Kjer) optic neuropathy (DOA) manifests between age 5 and 10 years. Visual loss may progress until the midteens, at which point it usually stabilizes. Color defects are almost universally present, and tritanopia (which can be detected with the Farnsworth-100 hue testing) is suggestive of DOA. Inheritance is naturally autosomal dominant, and DOA is linked to the OPA1 gene on chromosome 3.
28. c. LHON typically affects males age 10 to 30 years. The syndrome presents with acute, severe vision loss (<20/200), which is initially monocular, but then sequentially affects the fellow eye. Classic fundus findings include hyperemia of the optic disc, peripapillary telangiectasia, and tortuosity of the medium-sized retinal arterioles. The incidence of spontaneous partial recovery of vision has been reported to be as high as 10%. LHON exhibits mitochondrial inheritance (inheritance from the mother).
29. a. LHON is related to a mitochondrial DNA mutation, most frequently at the 11778 position, and less commonly at the 3460 or 14484 location. The corresponding single base-pair nucleotide substitution results in impaired mitochondrial adenosine triphosphate production, which tends to affect highly energy-dependent tissues, such as the optic nerve.
30. c. Patients with “papillophlebitis” have normal or near normal visual acuity. An RAPD is absent, color vision is normal, and visual field testing shows enlargement of the blind spot. Fundus examination shows marked retinal venous engorgement associated with hyperemic optic disc edema. Retinal hemorrhages extending to the equatorial region are common. It may be a form of incomplete CRVO, and usually resolves spontaneously within 12 months.
31. c. Optic disc drusen are refractile, often calcified nodules located on the optic nerve head. In childhood, optic disc drusen tend to be buried, but they become more visible over the years. When visible, optic drusen appear as round, whitish yellow refractile bodies.
32. b. Optic disc drusen occur almost exclusively in whites. They are bilateral in 75% to 86% of cases.
33. a. Morning glory disc anomaly is a funnelshaped staphylomatous excavation of the optic nerve and peripapillary retina. It is more common in females and is most often unilateral. White glial tissue is present on the central disc surface. The characteristic feature is the emanation of retinal vessels from the periphery of the disc. Visual acuity is often 20/200 or worse, and an RAPD and a visual field defect are present. Serous retinal detachments can occur in 30% of cases. Transsphenoidal basal encephaloceles may be present.
34. b. Superior oblique myokymia is a disorder that produces paroxysmal, monocular, high frequency bursts of contraction of the superior oblique muscle. They usually produce vertical or torsional oscillopsia.
35. a. Optics pits are depressions of the optic disc surface that is often gray or white. They are most often located temporally, and can be associated with a mild visual field defect. Optic pits are unilateral but can be bilateral in 15% of cases. Serous detachment of the macula develops in 25% to 75% of cases.
36. a. The optic neuritis treatment trial (ONTT) demonstrated that corticosteroid therapy had no long-term beneficial effect for vision. Intravenous methylprednisolone for 3 days followed by 11 days of oral prednisone accelerated recovery by 1 to 2 weeks. Oral prednisone as the initiating therapy was associated with an increased recurrence rate. Intravenous therapy demonstrated a reduction in the rate of development of clinical MS in the subgroup of patients with MRI scans showing two or more lesions at year two, but by year 3, this protective effect was lost. The value of intravenous corticosteroids to reduce the longterm risk of MS is unproven.
37. d. The most common location for a cerebral aneurysm with third nerve palsy is the junction of posterior communicating artery and internal carotid artery.
38. a. Third nerve aberrant regeneration never occurs with diabetic oculomotor neuropathy. Aberrant regeneration of the third nerve implies another etiology, such as aneurysm, tumor, inflammation, or trauma. Other classic findings of aberrant regeneration include persistent vertical gaze limitation secondary to simultaneous contraction of superior and inferior recti, and pupillary miosis with elevation, adduction, or depression.
39. b. The long intracranial course of the trochlear nerve leaves it especially susceptible to damage from closed head trauma. This occurs due to contrecoup injury from the free tentorial edge. Ischemic damage, usually due to diabetes mellitus, is second, and idiopathic palsies are third. Hydrocephalus, vascular loops, or tumor can compress the trochlear nerve as well.
40. d. The three-step test is useful for diagnosis but does not differentiate between congenital and acquired trochlear nerve palsy. Large vertical fusional amplitudes (greater than five prism diopters) and facial asymmetry from childhood head tilting suggest a decompensated congenital lesion.
41. b. The three steps of the Parks-Bielschowsky three-step test in order are (a) find the side of the hypertropia; (b) determine if the hypertropia is greater on left or right gaze; (c) determine if the hypertropia is greater on left or right head tilt. A right fourth nerve palsy shows a right hyperdevia-tion in primary position that worsens on left gaze and right head tilt. The opposite is true of a left fourth nerve palsy.
42. c. Nasopharyngeal carcinoma can involve numerous cranial nerves because of its proximity to the prepontine basal cistern. Most frequently, the trigeminal nerve is involved, causing facial hypesthesia or facial pain. The abducens nerve is the second most common. The hallmark of nasopharyngeal carcinoma is its propensity to involve multiple cranial nerves noncontiguously. Nasopharyngeal carcinoma is common in Chinese men. The least differentiated forms are also known as Schmincke’s and Regaud’s tumors.
43. b. An ischemic mononeuropathy is the most common cause of isolated sixth nerve palsy. At the onset of isolated sixth nerve palsy in a vasculopathic patient, neuroimaging is not required. Ocular motility typically resolves within 3 months. If improvement has not occurred after 3 months, a cranial MRI is mandatory. Impaired abduction in patients under 50 requires special attention because few cases are due to an ischemic neuropathy. Younger patients should undergo appropriate neuroimaging.
44. a. Neuromyotonia is a rare cause of episodic diplopia. Prior skull-base radiation therapy, typically for a neoplasm such as a meningioma is the most common historical feature. Months to years postradiation, patients experience episodic diplopia lasting typically 30 to 60 seconds. Neuromyotonia may affect the oculomotor, trochlear, or abducens nerve.
45. c. Charles Bonnet’s syndrome is the triad of visual hallucinations, ocular pathology causing bilateral visual deterioration, and preserved cognitive status. Hallucinations may be simple or highly organized and complex. Patients with visual allesthesia see their environment rotated, flipped, or inverted.
46. b. The hallmark of ophthalmoplegia secondary to a lesion of the cavernous sinus is multiple, ipsilateral ocular motor nerve dysfunction with some combination of third, fourth, fifth, and sixth A cranial nerves and sympathetic fibers. If only I one oculomotor nerve is involved, it is usually the sixth nerve, which is the only ocular motor nerve not protected within the dural wall of the cavernous sinus. Within the cavernous sinus, sympathetic branches of the paracarotid plexus joins the sixth nerve briefly. Occasionally, an intracavernous lesion can produce sixth nerve palsy with postganglionic Horner’s syndrome, producing pupillary miosis. Lesions of the cerebellopontine angle may involve the sixth cranial nerve as well as involve cranial nerves V, VII, and VIII. Chronic inflammation of the petrous bone may cause ipsilateral abducens palsy and facial pain called Gradenigo’s syndrome.
47. d. Tolosa-Hunt syndrome is an idiopathic, sterile inflammation that primarily affects the cavernous sinus. The pain in patients with Tolosa-Hunt syndrome typically responds rapidly and dramatically to corticosteroid therapy. Tolosa-Hunt syndrome is a diagnosis of exclusion.
48. c. Duane’s syndrome may be secondary to hypoplasia or aplasia of the abducens nucleus, with lateral rectus innervation via the oculomotor nerve. It has various presentations, but retraction of the adducted globe appears most consistently. The three types of Duane’s syndrome are distinguished by the relative ability to adduct or abduct: type 1, limited abduction but full adduction; type 2, normal abduction but limited adduction; and type 3, both abduction and adduction are limited.
49. a. Oculomotor apraxia is an inability to initiate voluntary saccades. Congenital oculomotor apraxia is characterized by using horizontal head thrusts past the points of interest. Acquired lesions results from bilateral lesions of the supranuclear gaze pathways of the frontal and parietal lobes, such as from bilateral strokes. Patients may blink to break fixation, and then turn their head to fixate on something else. Pursuits remain relatively unaffected.
50. b. In PSP, downward gaze is generally affected, becoming smaller and slower. Saccades are affected more than pursuits. This is in distinction to the dorsal midbrain syndrome, where upward saccades are generally affected. Patients with PSP have slow volitional saccades, but their reflexive saccades (saccades directed toward an unanticipated target) often are initially normal.
51. d. Skew deviation is, by definition, a vertical misalignment of gaze that cannot be assigned to a single nerve or muscle weakness. In the presence of an INO, the hypertropic eye is often on the same side as the adduction deficit (medial rectus dysfunction). Fourth nerve palsy does not produce difficulty with adduction. The “one-and-a-half” syndrome results in, among other things, complete horizontal paralysis of one eye and limitation of the other to abduction only. Dorsal midbrain syndrome (Parinaud’s syndrome) does not feature an adduction deficit.
52. b. Upward gaze paresis, light-near dissociation, lid retraction, skew deviation, retraction of the lids in primary position (Collier’s sign,) and convergence–retraction nystagmus are all features of the dorsal midbrain (Parinaud’s) syndrome. Convergence–retraction nystagmus is also a response to an effort at upgaze that triggers medial rectus contractions. Hence, this form of “nystagmus” is worsened by upward OKN testing. Paradoxic OKN is not a feature.
53. a. Congenital motor nystagmus has several features including paradoxic OKN characterized by the slow phase of eye movements moving in the direction opposite that of a rotating optokinetic drum, dampening by convergence, increased by distance fixation, and presence of a null point. Fortunately, oscillopsia, the sensation of the world moving, is not normally a problem.
54. a. The corkscrewed conjunctival vessels, all the way to the limbus, are highly suggestive of arte-rialization of the orbital venous system. Dural low flow fistulas could have a similar appearance, but the history of trauma is more suggestive of a carotid cavernous sinus fistula. On imaging, enlargement and tortuosity of the superior ophthalmic vein can be seen. Cavernous sinus thrombosis can occur in septic or aseptic individuals. Signs include ophthalmoplegia and orbital congestion with treatment being antibiotics, anticoagulants, or corticosteroids and surgery.
55. b. Opsoclonus consists of nonstop, random, directionally unpredictable saccades. Ocular flutter consists of spontaneous groups of back-and-forth horizontal saccades that may occur during fixation or at the end of a normal horizontal saccade. Both ocular flutter and opsoclonus may be associated with malignancy such as metastatic neuroblastoma in children, or small cell CA of the lung in adults. These eye movements may be the first presenting sign of cancer. MS can also cause ocular flutter. Square-wave jerks are a microsaccadic fixation disturbance associated with cerebellar disease of various kinds. Ocular motor dysmetria is a back-and-forth saccadic motion about the point of fixation that occurs following an otherwise normal saccade. It is felt to represent “overshooting” of the intended fixation point. Ocular bobbing is most commonly seen in comatose and/or quadriplegic patients with large infarcts or brainstem hemorrhages.
56. d. Monocular nystagmus has been associated with chiasmal and hypothalamic gliomas. It is also seen in blind eyes, multiple sclerosis, and spasmus nutans—a transient, fast-beating, but low- amplitude nystagmus with abnormal head movements and posture found during the first 5 years of life.
57. a. Alexander’s law describes the increased frequency and amplitude of nystagmus movements accompanying gaze in the direction of the fast phase.
58. d. Upbeat nystagmus can be due to lesions of the anterior vermis and lower brainstem, as well as drugs and Wernicke’s encephalopathy. Downbeat nystagmus may be localized to anatomic structures at the craniocervical junction (e.g., Arnold-Chiari malformation) and may be seen in certain intoxications (alcohol, lithium). Vestibular nystagmus has its etiology within the vestibular system. Periodic alternating nystagmus also can localize to the craniocervical junction but may be seen in other forms of posterior fossa disease. See-saw nystagmus may be congenital, but is most commonly found in patients with large parasellar tumors, frequently craniopharyngiomas.
59. b. Bitemporal hemianopia may be seen in acquired see-saw nystagmus because the posterior chiasm is most vulnerable to diencephalic lesions, which may provoke it.
60. a. Vestibular ocular reflex responses are driven both by semicircular canals and by the otoliths of the utricles and saccule. Brainstem neurons that drive vergence movements are located in the mesencephalic reticular formation, just dorsal to the third nerve nuclei. Saccades originate in the contralateral frontal lobe, whereas pursuits arise in the ipsilateral parietal lobe.
61. b. The greater superficial petrosal nerve synapses in the pterygopalatine ganglion, not in the geniculate ganglion.
62. a. The Marcus Gunn “jaw-wink” reflex is an example of synkinesis (abnormal innervation connecting two groups of normally unrelated muscles, such that they contract together), but it is not synkinesis as a result of aberrant regeneration, which usually follows a peripheral neuropathy or trauma to nerve. The “jaw-wink” is a congenital/neurogenic phenomenon.
63. c. Neuroretinitis is a clinical syndrome characterized by acute loss of vision in association with disc edema and a star pattern of exudates in the macula. Two-thirds of patients with neuroretinitis have been shown to have cat-scratch disease caused by Bartonella henselae or B quintana organisms.
64. c. The parotid gland can become infiltrated with granulomas, and the facial nerve is involved at this site. Facial nerve involvement in sarcoidosis is frequently bilateral, but asymmetric. The second most commonly involved cranial nerve is the optic nerve.
65. b. Hemifacial spasm is characterized by unilateral episodic spasm that involves the facial musculature and lasts from seconds to minutes. Essential blepharospasm is believed to be related to basal ganglia dysfunction, not hemifacial spasm. Compression of the facial nerve in the cerebellopontine angle by anomalous vessels has been demonstrated in 90% of cases of hemifacial spasm. Tumors in the cerebellopontine angle also can cause hemifacial spasm. Therefore, an MRI of the brain is typically performed to exclude a compressive lesion.
66. d. Facial myokymia is characterized by continuous unilateral undulating contraction of the facial muscle bundles. Facial myokymia is caused by disease in the pons involving the facial nucleus or fascicle. The most common causes include multiple sclerosis in adults and pontine glioma in children.
67. a. Essential blepharospasm is a bilateral condition consisting of episodic contraction of the orbicularis oculi. Onset usually occurs between ages 40 and 60. The treatment of choice is injection of botulinum toxin into the orbicularis oculi muscle.
68. d. The afferent pupillomotor fibers exit the optic tracts just before the lateral geniculate body (LGB); they do not pass through the LGB. Although postganglionic pupillomotor fibers in the sympathetic pathway do arise from the superior cervical ganglion, the sympathetic pathway leading to these fibers is thought to originate in the posterior hypothalamus. In addition, postganglionic sympathetic fibers enter the orbit with the ophthalmic division of the trigeminal nerve through the superior orbital fissure. The consensual pupillary response is seen because of decussation at the pretectal nuclei. Were the chiasm split in half, consensual responses would be preserved.
69. c. Argyll Robertson pupils are miotic, irregular, do not react to light, but have a normal near response. This is a rare finding in some patients with tertiary syphilis. In the light-near dissociation of Parinaud’s dorsal midbrain syndrome, the pupils are larger. In young children, the most common cause of this syndrome is a tumor in the region of the pineal gland. In young adults, head trauma and multiple sclerosis are frequently seen. In patients over 60, stroke is most commonly to blame.
70. c. Patients with normal pupils will respond to pilocarpine 1%. Thus, a weaker preparation (0.10%) is recommended that can demonstrate denervation supersensitivity. Features of an Adie tonic pupil include sluggish, segmental vermiform response to light with better response to the near reaction. The majority of patients (80%) will have unilateral pupillary involvement. After many months or years, an Adie’s pupil will become miotic.
71. c. Horner’s syndrome includes ipsilateral ptosis, miosis, and anhidrosis. Ptosis is secondary to lack of Müller’s muscle function. The distribution of anhidrosis depends on the location of the lesion. Interruption of the central or preganglionic neuron causes anhidrosis of the ipsilateral face. Lesions that are postganglionic, distal to the superior cervical ganglion, result in anhidrosis limited to the ipsilateral forehead. 4% cocaine is used to diagnose Horner’s syndrome. A normal pupil will dilate, but a Horner’s pupil will dilate poorly. Hydroxyamphetamine is used to localize the lesion. In postganglionic Horner’s syndrome, the eye will dilate poorly if at all in response to hydroxyam-phetamine, whereas a preganglionic and normal pupil will dilate. Painful Horner’s syndrome may be caused by many disorders (neck trauma, migraine, cluster headaches), but spontaneous dissection of the common carotid artery must be ruled out with angiography or MRI/MRA.
72. a. The fundus photograph demonstrates a retinal racemose angioma. Wyburn-Mason syndrome is a sporadic condition, characterized by a retinal racemose angioma with ipsilateral intracranial arteriovenous malformation (AVM). Patients with Wyburn-Mason syndrome can have orbital AVMs as well (and consequent ocular bruits). PDT is not used to treat Wyburn-Mason syndrome. However, it has been used to treat another vascular lesion of the retina, the retinal capillary hemangioma. PDT can be used for a retinal capillary hemangioma often when the patient is symptomatic from an exudative retinal detachment caused by this lesion.
73. c. The fundus photograph demonstrates a morning glory disc anomaly, a unilateral condition usually accompanied with severe visual loss. It can also cause RAPD. The other answers are correct.
74. d. Optic nerve head melanocytomas are dark brown lesions on the optic nerve head, which are typically benign, but can rarely undergo malignant transformation. They can produce relative APDs and visual field defects and should be followed to document growth.
75. c. Pheochromocytomas produce, secrete, and store catecholamines. They are most often derived from the adrenal medulla but may arise in any of the sympathetic ganglia. Two phakomatoses, neu-rofibromatosis, and von Hippel-Lindau disease, are associated with the tumor.
76. c. A retinal capillary hemangioma is a spherical orange-red tumor fed by a dilated, tortuous retinal artery and drained by an engorged vein. Racemose angiomas are retinal arteriovenous communications without intervening capillary bed and are associated with Wyburn-Mason syndrome. Retinal cavernous hemangioma is characterized by the formation of grapelike clusters of thin-walled saccular angiomatous lesions.
77. b. Retinal capillary hemangioma is associated with von Hippel-Lindau disease.
78. c. Cerebellar, brainstem, or spinal cord hemangioblastomas can occur in these patients. These patients may also have pheochromocytomas or renal cell carcinoma.
79. d. Astrocytic hamartomas can appear as a whitish-yellow mass (“mulberry lesion”).
80. c. Astrocytic hamartomas can be seen in tuberous sclerosis and neurofibromatosis, but is more commonly seen in tuberous sclerosis.
81. a. The vast majority of patients with astrocytic hamartomas are asymptomatic and do not require treatment.
82. c. Unilateral congenital glaucoma is seen in 30% to 70% of patients with Sturge-Weber syndrome and is usually associated with angioma of the upper lid.
83. d. Patients with ataxia–telangiectasia may have associated thymic hypoplasia, defective T-cell function, and IgA (secretory immunoglobulin) deficiency, with severe respiratory infections.
84. c. Many systemic syndromes such as myotonic dystrophy, oculopharyngeal dystrophy, and Kearns-Sayre syndrome include CPEO, which is a nondescriptive term for chronically progressive loss of eye movements. Oculopharyngeal dystrophy is classically seen in patients of French-Canadian ancestry. They typically present with progressive dysphagia followed by proximal muscle weakness and ptosis. Patients with myotonic dystrophy may have ptosis, pigmentary retinopathy, polychromatic (“Christmas tree”) cataracts, and thinning of the temporalis and masseter muscles (“hatchet face”). Patients with thyroid eye disease may have a restrictive ophthalmoplegia.
85. c. Four signs constitute complete Kearns-Sayre syndrome: (a) progressive external ophthalmoplegia; (b) mild pigmentary retinal degeneration; (c) onset before age 20; and (d) heart block, potentially lethal and among the last signs to develop. Some studies indicate that elevated CSF protein correlates with the presence of heart block.
86. a. There are several genetic syndromes associated with monocular diplopia due to lens subluxation. These include Marfan’s syndrome, Ehlers-Danlos syndrome and Weill-Marchesani syndrome. All of the other answers are potential causes for monocular diplopia.
87. a. Conjunctival injection, strabismus, and proptosis are seen in thyroid eye disease. Lid retraction s the most common sign.
88. a. The most frequently involved muscle in dysthyroid orbitopathy is the inferior rectus. The medial rectus is the second most frequently affected muscle and may simulate a sixth nerve palsy. One mnemonic for this is “I M Stuart Little” (inferior, medial, superior, lateral) in order of their involvement.
89. a. This is a classic description of Anton’s syndrome.
90. c. Although 75% of all myasthenics will have eye findings at presentation, only 33% to 50% will have ocular myasthenia only. A higher percentage (90%) of patients with MG will develop ocular symptoms during the course of the disease. Ptosis is the most common.
91. a. A tiny fraction of patients with MG will develop Graves’ disease as well.
92. b. Radiologic investigation is mandatory for all myasthenics in order to discover thymic enlargement. Thymectomy may be curative in this setting.
93. c. If ocular signs remain isolated for more than 2 years, the disease is likely to remain clinically ocular; though, late conversion to generalize MG is possible.
94. b. Studies of central retinal artery ligation in rhesus monkeys established this value (Hayreh).
95. d. Transient monocular blindness is the hallmark of carotid (anterior) disease. Vertebrobasilar insufficiency typically causes binocular visual blurring or oculomotor symptoms. Other symptoms of vertebrobasilar insufficiency include transient dysarthria, drop attacks, photopsias, and hemi-sensory defects.
96. c. The patient’s ocular signs and symptoms clinically suggest the diagnosis of demyelinative optic neuritis. With a history of paresthesias in her right leg, the diagnosis of multiple sclerosis should be entertained. An afferent pupillary defect almost invariably occurs in the acute phase. This patient most likely had a subclinical contralateral episode of optic neuritis in the past and therefore no detectable APD. APDs are always relative, that is, comparing one optic nerve to the contralateral nerve. In the Optic Neuritis Treatment Trial, oral steroid therapy showed to offer no improvement in long-term prognosis and had a higher rate of subsequent optic neuritis recurrence.
97. a. The etiology of Coats’ disease is unknown, and there does not appear to be any genetic, familiar, racial, or ethnic predisposition. However, Coats’-type retinal vascular changes have been noted in patients with facioscapulohumeral muscular dystrophy, Turner’s syndrome, Senior-Loken syndrome, and one variant of the epidermal nevus syndrome. In addition, Coats’-like retinopathy has been noted in up to 3.6% of patients with retinitis pigmentosa.
98. b. Downbeat nystagmus in primary position is localized to the craniocervical junction (or certain intoxications). This patient’s clinical symptoms of intermittent occipital headaches with sudden head movements or anger suggest the diagnosis of Arnold-Chiari malformation. Arnold-Chiari malformation is one of the most common causes of downbeat nystagmus.
99. a. Clonazepam, baclofen, gabapentin, base-out prisms, memantine, and 3,4-diaminopyridine have been used in the treatment of downbeat nystagmus.
100. a. This patient appears to have Parinaud’s dorsal midbrain syndrome, which may include the following findings: pupillary light-near dissociation, lid retraction (Collier’s sign), upgaze paresis, convergence–retraction nystagmus, fixation instability, small-amplitude skew deviation, and papilledema (if ventricular outflow has been compromised). The most common cause in this age group would be a pinealoma. Other causes include stroke, hydrocephalus, and multiple sclerosis.
101. d. After neuroimaging has been obtained, a lumbar puncture would be an important step in the diagnostic evaluation of this patient because pinealoma classically sheds cells into the CSF.
102. a. Optic neuritis in childhood is more commonly bilateral. Visual loss can be severe, although intravenous corticosteroids can improve visual function. Diffuse enlargement of the optic nerve on CT scan may be seen in this condition, mimicking a neoplasm of the optic nerve sheath. The demyelination typically follows a viral illness or vaccination by ten to 14 days.
103. b. Posterior ischemic optic neuropathy (PION) occurs in three distinct settings: perioperative, arteric, or nonarteric. There has been increasing reports associated with spinal surgery. Risk factors for this condition include being in the prone position during surgery, significant blood loss, and long anesthesia time. Vision loss in perioperative PION is often bilateral and severe.
104. d. Bilateral disc edema and headache may be caused by several things, but hypertension should be first on the list to be excluded because it is easy to do so and important to identify. After checking blood pressure, neuroimaging should be obtained.
105. d. Optic disc drusen may be associated with retinitis pigmentosa and with pseudoxanthoma elasticum.
106. b. Meningothelial (syncytial) meningioma is the most common histopathologic type of meningioma seen within the orbit. “Pilocytic” describes the cell type of gliomas of the visual pathways.
107. a. Optociliary shunt vessels are vessels that shunt retinal venous outflow to the choroidal circulation. They occur in approximately 30% of patients with optic nerve sheath meningiomas but are nonspecific. They can also occur in patients with sphenoid wing meningioma, optic glioma, CRVO, and chronic papilledema.
108. d. The most common etiologies of bilateral central or cecocentral scotomas include hereditary optic neuropathy and nutritional optic neuropathy (vitamin B12 and folate deficiency), drug toxicity, tobacco-alcohol amblyopia, and infiltrative disorders such as syphilis and tuberculosis. Cyanide levels are not helpful in suspected tobacco-alcohol amblyopia.
109. c. Optic neuropathy from toxic exposure or nutritional deficiency is characterized by gradual, progressive, bilaterally symmetric, painless visual loss affecting central vision and causing central or cecocentral scotomata. Ethanol abuse probably is associated with optic neuropathy in that it may contribute to malnutrition. Medications can also cause a toxic optic neuropathy. Most commonly implicated medications include ethambutol, isoniazid, chloramphenicol, hydroxyquinolones, penicillamine, cisplatin, and vincristine.
110. d. Although disc edema, disc hemorrhages, and choroidal rupture may be seen in acute traumatic optic neuropathy, the most common finding is a normal fundus. Disc pallor would be unusual in the acute setting, but present in all cases after several weeks (4–8 weeks.)
111. b. The development of diabetic papillopathy appears to be independent of serum glucose levels. Diabetic papillopathy is classically seen in young adults with type 1 diabetes with moderate to severe retinopathy (although it can be seen in type 2 patients as well). It is painless, and associated visual loss is generally mild. The distinction of diabetic papillopathy as an entity unique from AION remains controversial. The disorder generally resolves spontaneously.
112. a. Thyroid optic neuropathy is considered to be a compressive optic neuropathy due to enlargement of extraocular muscles at the orbital apex. Treatment of thyroid optic neuropathy may include orbital radiation (usually 1,500–2,500 rad over a 10-day period) and orbital decompression, which provides the most potential for decompression of the optic nerve. Systemic corticosteroids are thought to be effective only in the acute congestive phase and not in the fibrotic period. Thus, if no response is noted within 3 weeks, systemic steroids should be tapered and another modality should be considered. Although a subtotal thyroidectomy may provide primary treatment of dysthyroid state, it will have no effect on the eye findings (except, perhaps, lid retraction).
113. a. Bromocriptine has been shown to be effective primarily in the management of prolactin-secreting pituitary tumors and is less effective or ineffective with other types of pituitary tumors.
114. c. The symptoms presented in this question are indicative of pituitary apoplexy (Sheehan’s syndrome), in which there is a hemorrhage into a pituitary tumor. A sudden severe headache is a common presenting symptom; other manifestations depend on the direction of the expansion of pituitary gland. Acute painful visual loss is uncommon with the other disorders.
115. c. The nasociliary nerve is a division of CN V1 and supplies the cornea.
116. c. A skew deviation is a motility disturbance with a vertical component that does not have a pattern consistent with a discrete muscle underaction or nerve palsy. They are generally due to supranuclear or vestibuloocular dysfunction and generally reflect brainstem disease. They are typically comitant, but not always.
117. b. Although transient changes in vertical eye movements and slowing of vertical saccades can result from lesions of the paramedian pontine reticular formation, nuclei critical for the initiation of vertical eye movements are the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) and the interstitial nucleus of Cajal (INC).
118. c. Medial rectus contracture is distinctly uncommon in Duane’s syndrome. In congenital sixth nerve palsy, it is quite common and results in esotropia in primary position. Although the left eye is more commonly involved in Duane’s syndrome, this does not help in distinguishing from congenital sixth nerve palsy.
119. a. Disruption of the medial longitudinal fasciculus (MLF), which carries projections of interneurons from the contralateral sixth nerve nucleus to the ipsilateral medial rectus subnucleus, results in ipsilateral absence or slowing of adduction and contralateral abduction nystagmus. This combination of findings is termed internuclear ophthalmoplegia. Vertical nystagmus and skew deviations are frequently found in association with internuclear ophthalmoplegia but are not universal.
120. b. A bilateral INO produces bilateral adduction lag, bilateral abducting nystagmus, and vertical, gaze-evoked nystagmus that is best appreciated in upgaze. The two most common causes of INO are demyelination and stroke. In adolescents and younger adults, INO is typically caused by demyelination. In older adults, microvascular disease is the most common cause.
121. d. A lesion that disrupts both the abducens nucleus or pontine paramedian reticular formation and the ipsilateral MLF will result in the combination of an ipsilateral gaze palsy and internuclear ophthalmoplegia. This combination has been termed the “one-and-a-half” syndrome. The only horizontal eye movement that remains is contralateral abduction.
122. b. A large-angle exodeviation can occasionally occur in association with a bilateral INO, resulting in a syndrome called “wall-eyed” bilateral INO.
123. d. Miller-Fisher syndrome is generally considered a variant of Guillain-Barré syndrome that results in ophthalmoplegia, ataxia, and areflexia. Serum IgG autoantibodies and elevated CSF protein may be present. Complete recovery is common.
124. a. The presence of optic nerve dysfunction, manifested by decreased vision, an afferent pupillary defect, and/or dyschromatopsia, distinguishes an orbital apex syndrome from a cavernous sinus syndrome because the optic nerve passes through the optic canal and does not enter the cavernous sinus.
125. b. Iris and posterior segment neovascularization and rapidly progressive cataract may all be seen as complications of the ischemic oculopathy that these fistulae generate. These fistulae often produce elevated intraocular pressure and proptosis. Corneal exposure due to proptosis is another potential complication of carotid–cavernous fistula.
126. d. Acute thiamine deficiency (Wernicke’s encephalopathy) can result in central scotomas as well as ophthalmoplegia, primarily affecting cranial nerves III and VI. It can be precipitated in nutritionally depleted alcoholics given intravenous glucose alone, due to sudden consumption of systemic thiamine stores.
127. d. Autofluorescence is produced when certain tissues/material are stimulated with monochromatic blue light and emit in the yellow-green range, as fluorescein does. The two optic nerve lesions that may autofluoresce are astrocytic hamartomas and drusen. Large accumulations of lipofuscin also may autofluoresce. To demonstrate this, fundus photographs should be obtained through the standard fluorescein setup, but without fluorescein injection. Lesions will appear bright, as if they had absorbed fluorescein, even though none was injected. Note that this is not the same as a “red-free” photographs (which are produced with a green filter that does not provide sufficient blue light to stimulate autofluorescence).
128. b. Based on autopsy studies, the prevalence of GCA has been estimated to be 1.1% of the Scandinavian population. People born in Northern European countries appear to have higher rates of giant cell arteritis. People of Scandinavian origin are particularly at risk.
129. b. PMR is a surprisingly common disorder. Patients with PMR are at higher risk for developing GCA.
130. a. The classic field abnormality associated with optic chiasmal disorders is a bitemporal hemi-anopia, not a homonymous hemianopia, which is seen with retrochiasmal lesions. Postfixation blindness is a necessary concomitant of bitemporal hemianopia. Objects behind the point of fixation are in the temporal hemifield of each eye. With loss of these fields, nothing beyond the point of fixation is visible. Reds and greens often appear “washed out” in the temporal hemifield of affected patients. “Hemifield slip” refers to the diplopia these patients may also notice. By mechanisms that are not entirely understood, binocular input at the vertical midline seems necessary for motor fusion. When a substantial portion of the vertical midline is not overlapped by both visual fields, there may be loss of motor fusion with resultant diplopia.
131. b. Pupillary fibers from the optic tract exit before reaching the lateral geniculate body and exit into the pretectal olivary nuclei.
132. c. The Pulfrich phenomenon probably reflects delayed conduction in the demyelinated nerve. Oscillating objects perceived by the affected eye appear to be behind the image seen with the healthy eye, simulating three-dimensional movement where there is only movement within one plane.
133. b. The delayed implicit time is the electrophysiologic correlate of the bizarre perception known as the Pulfrich phenomenon.
134. d. The examination reveals pseudo-disc edema: the disc appears elevated with blurred, indistinct disc margins with dilated, telangiectatic peripapillary capillaries but no dye leakage on angiography This constellation is pathognomonic for Leber’s hereditary optic neuropathy (LHON). The disease is typically asynchronous and bilateral. Many patients have asymptomatic, but important electrocardiographic abnormalities, most commonly a preexcitation syndrome. It is theorized that the added metabolic burden of tobacco and alcohol use may exacerbate the defect in oxidative metabolism caused by the defects in mitochondrial and nuclear DNA. A small percentage of patients can have partial recovery of vision.
135. d. As is now well understood, the primary genetic defect underlying LHON resides in the mitochondrial DNA of every somatic cell. This defect is inherited strictly from the cytoplasm of the maternal egg. As paternal sperm carry no mitochondria, the disease is maternally inherited. There is clearly a gender predilection, with 80% to 90% of affected individuals being men. Fifty percent of affected individuals will have a point mutation at position 11778 of the mitochondrial DNA, resulting in impaired ATP production. No treatment has been proven effective
136. b. The right eye’s adduction is clearly slowed, indicating a right internuclear ophthalmoplegia (INO). The lesion is always on the same side of the brainstem as the eye with impaired adduction. Thus, her lesion is on the right side of her brainstem. Some patients with myasthenia gravis (MG) will present with a pseudo-INO virtually indistinguishable from a true INO. Any other associated motility disorders, particularly ptosis or fatigability of adduction, should prompt a Tensilon test. Traumatic INO has a good prognosis for recovery. If convergent adduction is preserved, the term “posterior” INO has been used, historically. Anterior INO implies a more rostral lesion, more likely to impair convergent as well as saccadic adduction.
137. c. Patients with INO typically show “abduction nystagmus” of the contralateral eye. Thus, a patient with a right INO may have nystagmus when looking to the left.
138. d. Anisocoria aggravated by cocaine implies Horner’s syndrome. Cocaine blocks reuptake of catecholamines at the synapse. In Horner’s syndrome, the catecholamine level at sympathetic synapses (iris dilator) is lower, so the mydriasis normally caused by cocaine is lessened. Hydroxyamphetamine stimulates release of catecholamines from the presynaptic neuron at the effector junction. If hydroxyamphetamine fails to dilate the abnormal, miotic pupil (in this case, the right pupil), the lesion must be postganglionic. In Horner’s syndrome, the miotic pupil is the abnormal one, due to relative lack of sympathetic stimulation. In the acute phase, the affected eye may be injected (lack of sympathetic vasodilation), hypotonous (reduced aqueous secretion), and mildly inflamed (breakdown of the blood–ocular barrier). So-called Pancoast’s tumor, a primary pulmonary carcinoma of either upper lobe, may compress the second order sympathetic neurons, causing preganglionic Horner’s syndrome.
139. b. Painful Horner’s is an acute dissection of the internal carotid artery until proven otherwise. The diagnosis of exclusion then becomes migraine if the angiogram is normal.
140. b. Bilaterally elevated discs with indistinct margins raise the possibility of papilledema, particularly in an obese young woman (pseudotumor cerebri). The photo demonstrates two findings arguing against this diagnosis. First, the vessels are clearly visible, with no obscuration of their borders. This is a sensitive finding in true pap-illedema. Second, two or three tiny excrescences with a crystalline appearance within the neural rim are visible. The figure reveals either auto- or pseudofluorescence (hyperfluorescence despite no injection of fluorescein). The clinical findings are consistent with a lesion known to be associated with autofluorescence, optic nerve drusen. Typically, visual acuity is normal, although there may be associated field defects. Axoplasmic stasis is a feature of true papilledema, rather than pseudopapilledema, which is present here. Autofluorescence is well described for both optic nerve drusen and astrocytic hamartomas of the optic nerve head. Both lesions may appear quite similar clinically. A distinguishing feature is the hypervascularity of astrocytomas, best revealed with fluorescein angiography.
141. d. The visual fields reflect a bitemporal hemianopia. This indicates chiasmal compression. Although this may occur with severe hydrocephalus of any cause, the primary lesion is usually parasellar. In this case, there is a huge pituitary tumor, probably nonsecreting; the chiasm can be seen riding on top of this impressive mass. Option (a) is a large occipital infarct, (b) is a parietal lobe metastasis, and (c) is a meningioma of the falx cerebri.
142. c. The CT scan reveals absence of the septum pellucidum, a thin layer of serous connective tissue separating the two lateral ventricles. This is clearly associated with bilateral optic nerve hypoplasia and hypothalamic–pituitary disturbances, typically underfunctioning. Precocious puberty may be a part of polyostotic fibrous dysplasia (Albright’s syndrome). Ash-leaf macules and pheochromocytoma may be seen in various phakomatoses (tuberous sclerosis, neurofibromatosis, and von Hippel-Lindau syndromes).
143. b. This MRI image demonstrates central nervous system anatomy at the level of the midbrain. A unilateral brainstem lesion here could result in numerous defects. Weber’s syndrome refers to an intramedullary CN III lesion within the substance of the cerebral peduncle where descending fibers of the corticospinal tract run. This results in third nerve palsy and contralateral hemiplegia (the motor fibers within the corticospinal tract decussate at the caudal medulla, distal to the lesion of Weber’s syndrome).
144. a. Sumatriptan is a serotonin antagonist available orally, via injection, or as a nasal spray. The “-triptan” antimigraine drugs are used for symptomatic relief of migraines, but are contraindicated in patients with basilar artery migraine. They can produce MI and should be used with caution in patients with severe hypertension or coronary artery disease.
145. d. Methysergide is an ergot alkaloid with numerous potential side effects. Prophylaxis can be achieved with the use of beta-blockers, calcium channel blockers, tricyclic antidepressants, selective serotonin reuptake inhibitors, sodium valproate, topiramate.
146. c. Patients in the surgical group were significantly more likely to lose at least three lines of acuity. There is no proven therapy for NAION.
147. d. Pseudotumor cerebri typically (not universally) presents with visual loss and headaches. Neurologic abnormalities are usually absent, except for occasional abducens paralysis. Although the opening pressure is elevated, CSF protein levels are either normal or low.
148. a. Binding antibodies to acetylcholine receptors are found in 90% of patients with generalized MG.
149. d. Ocular myasthenia has only ocular involvement without any systemic manifestations.
150. b. The disease is indistinguishable from MG, with an onset averaging 6 months after initiation of therapy. Approximately 80% of patients will remit completely within 6 to 8 months of cessation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Answers
Answers