Neck Neoplasms
- Primary neoplasms of the soft tissue in the head and neck are rare.
- The most common benign tumors are paragangliomas and nerve cell tumors.
- The most common malignant neoplasm is metastatic squamous cell carcinoma from the upper aerodigestive tract.
- The evaluation of a metastatic squamous cell carcinoma without an easily identifiable primary site is extensive and treatment is controversial.
- Neck dissections are performed to treat metastatic neoplasms and to determine the presence of occult metastasis.
Neck neoplasms include not only metastatic squamous cell carcinoma but also a number of other primary neck tumors. Metastatic squamous cell carcinoma arises from the upper aerodigestive tract and is present in the lymph nodes and in the neck; other primary tumors arise from the soft tissue in the neck, such as fat, fibrous tissue, muscle, blood vessels, lymphatic vessels, nerves, and paraganglia (Table 28–1). These primary tumors are fairly uncommon, often making a pathologic diagnosis difficult. The evaluation of all neck masses consists of obtaining a complete history and conducting a physical exam.
| Benign | Malignant |
|---|---|
| Vascular—hemangioma, lymphangioma | Lymphoma |
| Paraganglioma—glomus vagale, carotid body tumor | Synovial sarcomas |
| Neural—Schwannoma, neurofibroma | Malignant peripheral nerve sheath tumor |
| Fibromatosis | Fibrosarcoma |
| Lipoma | Liposarcoma |
| Rhabdomyoma | Rhabdomyosarcoma |
The presenting symptom of a neck neoplasm is a painless enlarging neck mass that may grow extremely slowly or very rapidly. On physical examination, there is often a well-circumscribed mass in the neck. The location of the mass sometimes suggests its cause.
Imaging with computed tomography (CT) or magnetic resonance imaging (MRI) is critical for these lesions, especially if these studies are performed before a biopsy is obtained. A preoperative study can better assess both the size and the extent of the lesion without confounding factors such as bleeding and edema. An MRI is often the study of choice because it allows a greater differentiation of soft tissue. A positron emission tomography (PET) scan in evaluating patients with metastatic disease can identify additional tumor masses. Additional studies such as angiography and, recently, magnetic resonance angiography (MRA) add valuable information to the diagnosis of vascular lesions (eg, carotid body tumors and vascular malformations).
A tissue specimen is vital for the diagnosis of neck neoplasms and can be obtained via a fine-needle aspiration biopsy (FNAB). Metastatic squamous cell carcinoma has an excellent specificity and sensitivity for FNAB. Additional studies such as flow studies, immunohistochemistry techniques, or electron microscopy may be required for an accurate diagnosis of these specimens.
Open biopsies consist of incisional and excisional biopsies. A small superficial lesion or any lesion smaller than 3 cm should undergo an excisional biopsy with sufficient normal surrounding tissue for adequate, clear margins. An incisional biopsy should only be entertained if the mass is larger than 3 cm. If metastatic squamous cell carcinoma is suspected, an open biopsy should not be considered unless all other avenues have been exhausted and at least two inconclusive FNAB.
After either an FNAB or open biopsy is performed, the specimen then undergoes evaluation with light microscopy. Immunohistochemistry techniques can stain for cytokeratin, leukocyte common antigen, S-100, and myoglobin to differentiate sarcomas, melanomas, and epithelial carcinomas. Electron microscopy is used to aid in the diagnosis in patients where light microscopy and immunohistochemistry techniques prove ineffective.
The most common benign masses in the neck are inflammatory lymph nodes and masses of salivary and thyroid gland origins. True soft-tissue benign tumors in the neck are relatively uncommon.
Paragangliomas arise from paraganglia, islands of cells derived from neural crest cells, associated with arteries and cranial nerves located at the carotid body, vagal body, along laryngeal nerves, and in the jugulotympanic region. The tumors derived from these regions are carotid body tumors, intravagal paragangliomas, and glomus tympanicum and glomus jugulare. While paraganglia cells are capable of producing catecholamines, the incidence of catecholamine-producing head and neck paragangliomas is exceedingly rare.
Carotid body tumors are the most common head and neck paragangliomas. The carotid body is found at the bifurcation of the common carotid artery and responds to changes in arterial pH, oxygen, and carbon dioxide.
Symptoms are present only with large tumors and include pressure, dysphagia, cough, and hoarseness. On examination, the mass is palpated at the anterior border of the sternocleidomastoid muscle. It is typically mobile laterally but not vertically.
The diagnosis requires a high index of suspicion as the location is similar to that of many other masses (eg, branchial cleft cysts and enlarged lymph nodes). Fine-needle aspiration of these lesions often yields only blood; however, if cells are obtained, FNA can offer a definitive diagnosis.
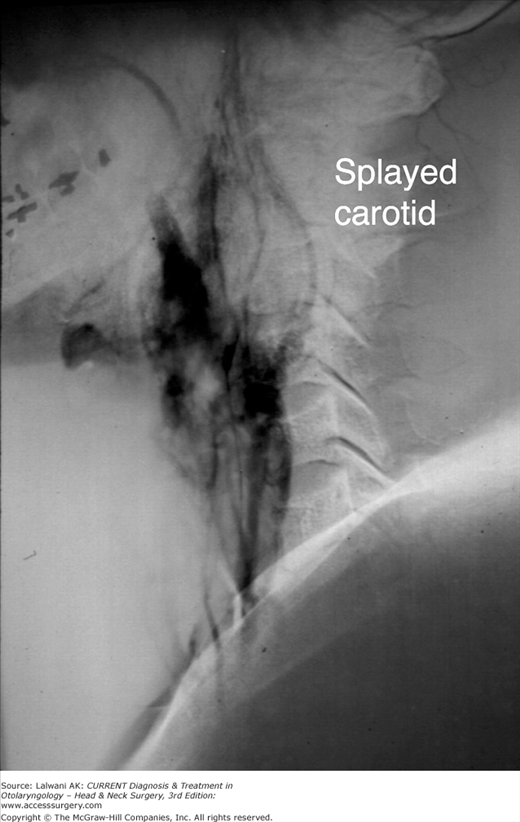
The angiogram in Figure 28–1 shows the typical findings of a splayed bifurcation of the carotid artery with a vascular blush. An MRI often proves useful in identifying other paragangliomas as synchronous and metachronous lesions occur in 25–48% of cases. Familial paragangliomas occur in 7–9% of cases.
The treatment of these lesions is predominantly surgical. Preoperative embolization is useful to minimize blood loss in order to allow for a cleaner dissection. Surgical excision requires the following measures: (1) identification of the proximal and distal carotid artery and (2) identification and preservation of the vagus, hypoglossal, and spinal accessory nerves. Patients with large or recurrent tumors often require vascular reconstruction, which should be planned preoperatively.
Radiation therapy is not the primary mode of therapy but has been used as the sole method of treatment in some cases such as elderly patients who are poor surgical candidates. In patients with carotid body and vagale tumors, radiation therapy alone has been shown to provide a local control rate of as much as 96%. Control rates with surgery alone range from 88% to 100%. Treatment decisions are based on surgical risks and complications; therefore, small tumors should usually be treated surgically, with radiation therapy reserved for large tumors.
Intravagal paragangliomas typically occur in association with one of the vagal ganglia, most commonly the ganglion nodosum. Intravagal paragangliomas account for approximately 3% of all head and neck paragangliomas. Symptoms can include hoarseness, dysphagia, aspiration, tongue weakness, and Horner syndrome. Angiographic imaging shows a mass located above the carotid bifurcation, with lateral and medial displacement of the external and internal carotid arteries. FNA has been useful in the diagnosis of these tumors.
The treatment involves surgical resection, with radiation therapy reserved for patients with high surgical risk, incomplete resection, recurrent disease, and bilateral tumors. Most intravagal paragangliomas can be resected via a cervical approach. If there is intracranial extension, a middle or posterior fossa approach may be needed.
Tumors arising from peripheral nerves typically arise from the Schwann cells in the nerve sheath. Of the many names used to describe these tumors, two in particular—schwannomas and neurofibromas—have significant clinical differences that warrant discussion. As a group, neurogenous tumors occur most commonly in the head and neck regions. They are often asymptomatic and present as lateral neck masses.
Peripheral nerve schwannomas, more appropriately termed neurilemomas, are solitary, well-encapsulated tumors. Histologically, these tumors have characteristic Antoni A and Antoni B tissues. Antoni A tissue consists of palisading nuclei around central cytoplasm and Antoni B tissue is comprised of a loose edematous matrix. These tumors can arise from cranial nerves, peripheral motor and sensory nerves, and the sympathetic chain. They can sometimes present with a displaced tonsil or a lateral pharyngeal wall when the mass is located in the parapharyngeal space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree