 Miscellaneous Lesions tha Simulate Conjunctival Neoplasms
Miscellaneous Lesions tha Simulate Conjunctival NeoplasmsConjunctival Epithelial Inclusion
General Considerations
Several primary cystic lesions can occur in the conjunctiva (1,2,3,4,5,6,7,8,9,10,11,12,13). Although conjunctival epithelial inclusion cyst is a very common lesion, surprisingly little has been written on this subject and it is only mentioned briefly in textbooks (1,2,3,4). It is usually stationary and recognized readily on slit-lamp examination as a benign cyst. Surgical excision is not recommended. Occasionally a conjunctival inclusion cyst becomes large and symptomatic and extends into the orbit; in these cases, surgical excision is necessary (11,12). In other instances, a conjunctival inclusion cyst can be larger or atypical and the possibility of a neoplasm prompts surgical excision.
Clinical Features
Clinically, a conjunctival inclusion cyst is a smooth, thin-walled lesion. It may contain clear or slightly turbid fluid. In some instances, epithelial debris secreted into the lumen of the cyst can deposit inferiorly and assume a “pseudohypopyon” appearance. Particularly in dark-skinned patients, a cyst can be lined with pigment, leading to clinical suspicion of malignant melanoma (5). Conjunctival-orbital cyst has been observed in patients with mucous membrane disorders, like Steven-Johnson syndrome (6).
Although most conjunctival cysts are simple inclusion cysts, there are many causes of a cystic lesion of the conjunctiva, including epithelial implantation cysts from surgical or nonsurgical trauma and parasitic cysts. Some tumors, like lymphangioma and diffuse conjunctival nevus, can be highly cystic. These are discussed elsewhere.
Pathology
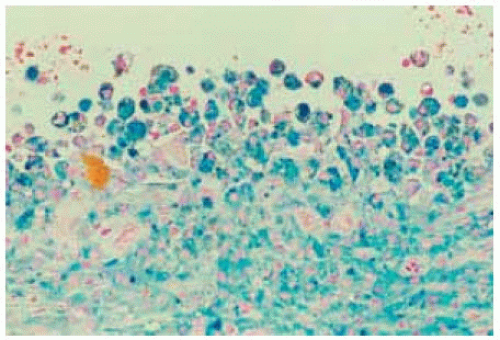
Histopathologically, an epithelial inclusion cyst is usually lined by conjunctival epithelium. The lumen can be clear or it can contain mucinous material, epithelial debris, and occasionally keratin. In some instances, the keratin or sebaceous debris can gravitate inferiorly to form an intracystic “pseudohypopyon.”
Management
In most instances, a conjunctival inclusion cyst can be followed and the lesion may eventually disappear. Larger lesions that produce symptoms or raise suspicion of a neoplasm can be excised locally. Some authors have recommended using indocyanine green solution to facilitate visualization of the cyst during surgery. The prognosis is generally excellent. Sometimes, a cyst may show progressive enlargement and become so extensive that excision may be necessary
Selected References
1. Shields CL, Shields JA. Overview of tumors of the conjunctiva and cornea. In: Foster CS, Azar DT, Dohlman CL, eds. Smolin and Thoft’s The Cornea. 4th ed. Philadelphia: Lippincott, Williams & Wilkins; 2005:735-755.
2. Shields JA, Shields CL. Tumors of the conjunctiva. In: Stephenson CM, ed. Ophthalmic Plastic, Reconstructive and Orbital Surgery. Stoneham, MA: Butterworth-Heinemann; 1997:260-261.
3. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
4. Shields CL, Demirci H, Karatza E, et al. Clinical survey of 1643 melanocytic and nonmelanocytic tumors of the conjunctiva. Ophthalmology 2004;111:1747-1754.
5. Jahnle R, Shields JA, Bernardino V, et al. Pigmented conjunctival inclusion cyst simulating a malignant melanoma. Am J Ophthalmol 1985;100:483-484.
6. Desai V, Shields CL, Shields JA. Orbital cyst in a patient with Stevens Johnson syndrome. Cornea 1992;11:592-594.
7. Bouncier T, Monin C, Baudrimont M, et al. Conjunctival inclusion cyst following pars plana vitrectomy. Arch Ophthalmol 2003;121:1067.
8. Raina UK, Jain S, Arora R, et al. Photographic documentation of spontaneous extrusion of a subconjunctival cysticercus cyst. Clin Exp Ophthalmol 2002;30:361-362.
9. Kobayashi A, Saeki A, Nishimura A, et al. Visualization of conjunctival cyst by indocyanine green. Am J Ophthalmol 2002;133:827-828.
10. Agarwal M, Amitava AK. Spontaneous expulsion of a subconjunctival cysticercus cyst. J Pediatr Ophthalmol Strabismus 2000;37:371-372.
11. Basar E, Pazarli H, Ozdemir H, et al. Subconjunctival cyst extending into the orbit. Int Ophthalmol 1998;22:341-343.
12. Shields JA, Shields CL. Orbital cysts of childhood—classification, clinical features and management. The 2002 Angeline Parks lecture. Surv Ophthalmol 2004;49:281-299.
13. Desai V, Shields CL, Shields JA. Orbital cyst in a patient with Stevens Johnson syndrome. Cornea 1992;11:592-594.
Conjunctival Epithelial Inclusion Cyst
Jahnle R, Shields JA, Bernardino V, et al. Pigm ented conjunctival inclusion cyst sim ulating a m alignant melanoma.Am J Ophthalmol 1985;100:483-484.
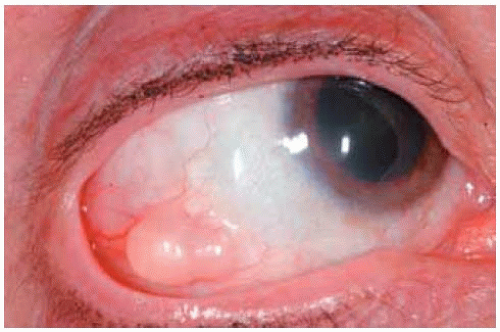
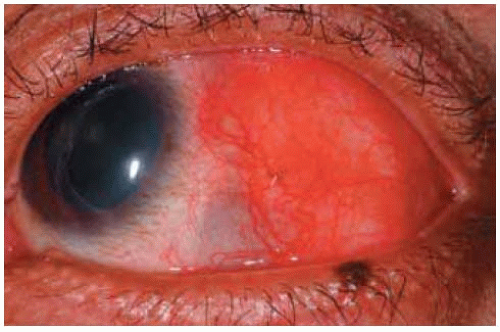
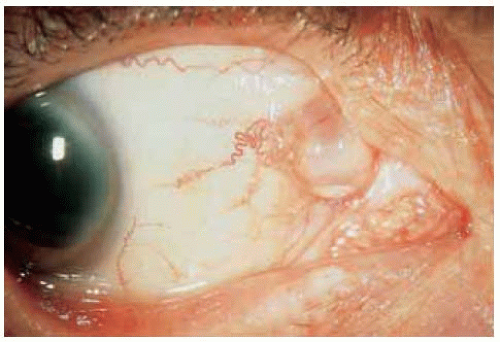 Figure 24.2. Nasal conjunctival inclusion cyst w ith layered epithelial debris in the lumen, forming a “pseudohypopyon” in a 61-year-old man. |
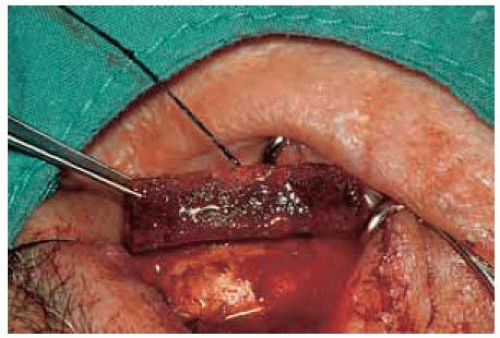
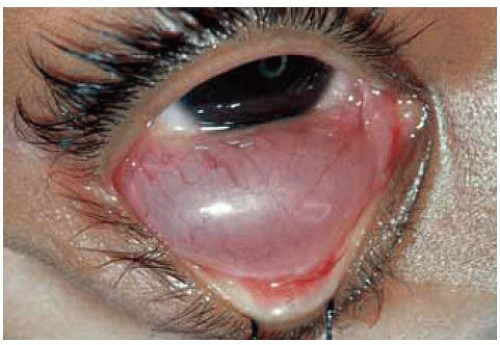 Figure 24.3. Giant epithelial inclusion involving the inferior conjunctiva in a 5-year-old girl. W ith m eticulous dissection, the cyst was rem oved, leaving intact the overlying surface epithelium. |
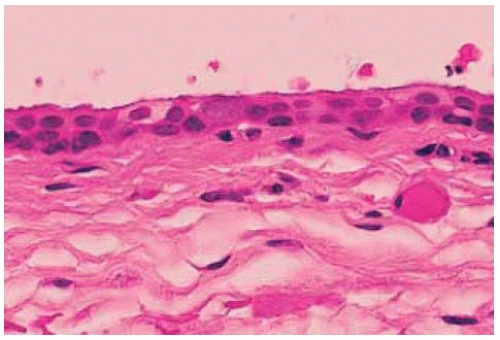 Figure 24.4. Histopathology of lesion in Figure 24.3 showing the nonkeratinizing epithelium lining the cyst. (Hematoxylin-eosin 10.) |
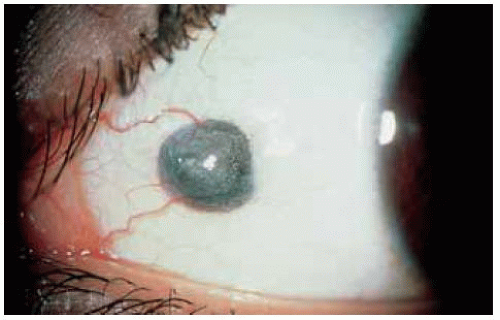
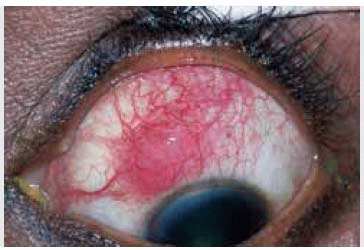
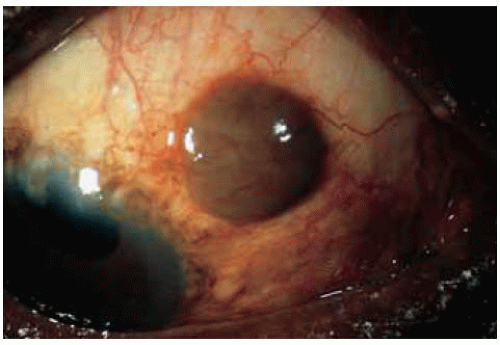 Figure 24.5. Pigmented epithelial inclusion cyst simulating a conjunctival melanoma in a 62-year-old African American patient. |
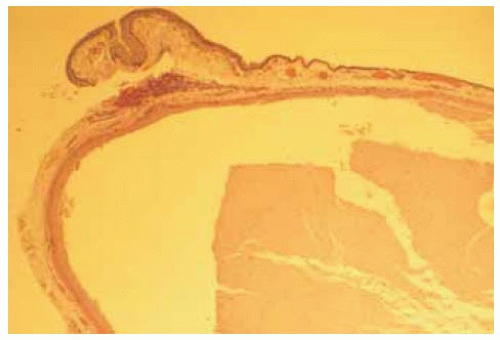 Figure 24.6. Histopathology of lesion shown in Figure 24.5. Much of the m elanotic appearance w as due to pigm ent in the surface epithelium over the cyst, rather than pigment in the wall of the cyst. (Hematoxylin-eosin 10.) |
Conjunctival Organizing Hematoma (“Hematic Cyst”; “Hematocele”)
General Considerations
Organizing hematoma is a circumscribed blood clot that can simulate a pigmented tumor. In the ocular area, the lesion is best known to occur under the periosteum of the orbit, often after overt or occult trauma (1,2,3,4). Although the terms “hematic cyst” or” were previously used by most authors (1,3), it has recently been stressed that, because it lacks a true epithelial lining, the term “cyst” is inappropriate and “organizing hematoma” is the preferred terminology (2). In the conjunctiva, an organizing hematoma can occur spontaneously, after surgical or nonsurgical trauma. Bleeding around an implant for retinal detachment repair can occasionally be confused with conjunctival melanoma (4). Orbital and conjunctival cysts occur occasionally in the anophthalmic orbit following enucleation (5).
Clinical Features
Organizing hematoma is often dark in color, suggesting a malignant melanoma. However, it generally lacks feeder vessels or episcleral sentinel vessels.
Pathology
Management
Organizing hematoma can be observed if blood is expected. However, if the lesion does not resolve and produces a foreign body sensation or other symptoms, then surgical excision is justified.
Selected References
1. Shields JA. Cystic lesions of the orbit. In: Shields JA, ed. Diagnosis and Management of Orbital Tumors. Philadelphia: WB Saunders; 1989:89-120.
2. Henderson JW. Cysts. In: Henderson JW, ed. Orbital Tumors. 3rd ed. New York: Raven; 1994:73-78.
3. Shapiro A, Tso MOM, Putterman AM, et al. A clinicopathologic study of hematic cysts of the orbit. Am J Ophthalmol 1986;102:237-241.
4. Lieb WE, Shields JA, Shields CL, et al. Postsurgical hematic cyst simulating a conjunctival malignant melanoma. Retina 1990;10:63-67.
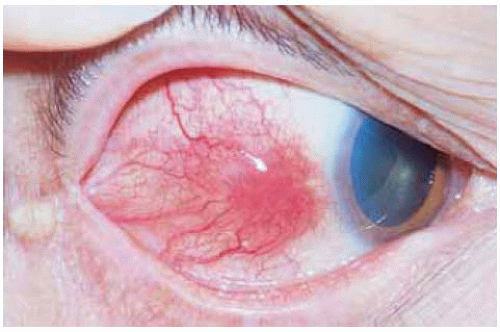
Conjunctival Organizing Hematoma Secondary to Silicone Sponge for Retinal Detachment Repair
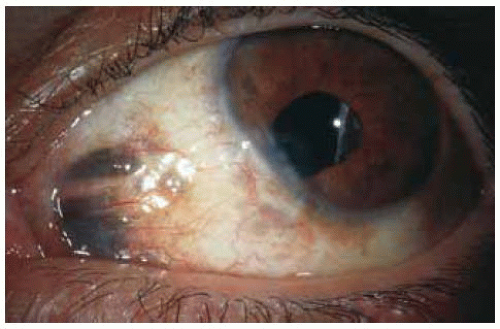
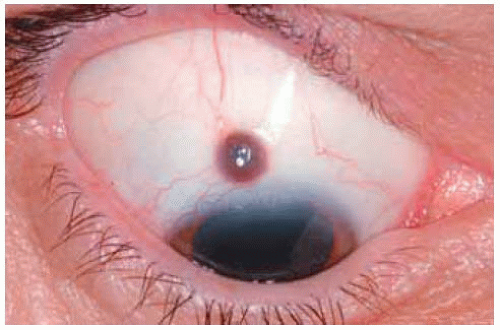
Chronic bleeding around a sponge used for retinal detachment repair can simulate a conjunctiva melanoma, as occurred in this 75-year-old man 15 years after retinal detachment surgery.
Lieb W E, Shields JA, Shields CL, et al. Postsurgical hem atic cyst sim ulating a conjunctival m alignant melanoma. Retina 1990;10:63-67.
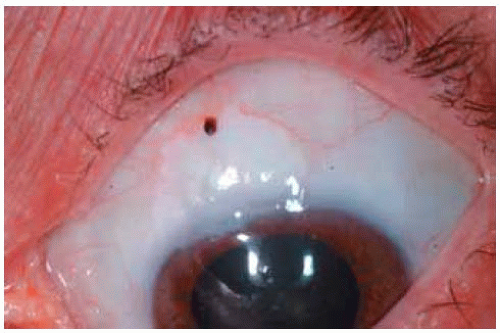
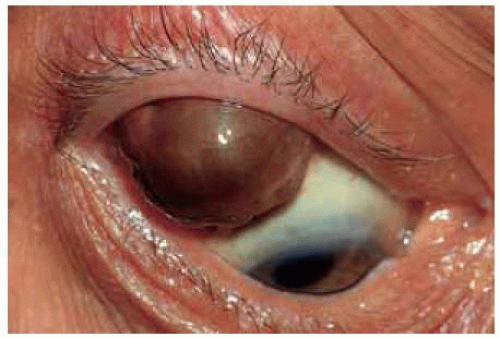 Figure 24.7. Dome-shaped pigmented mass in conjunctiva superotemporally. Note the lack of large feeding and draining blood vessels that would generally be evident in a true melanoma. |
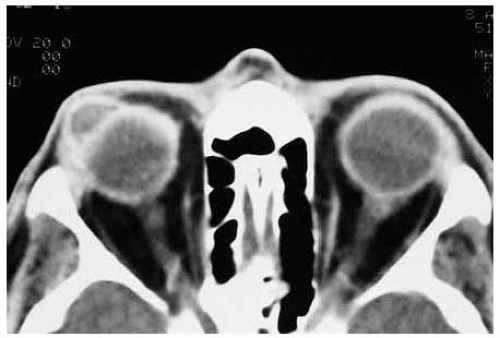 Figure 24.8. Axial computed tomograph showing that the lesion in Figure 24.7 has a cystic, rather than a solid, appearance. |
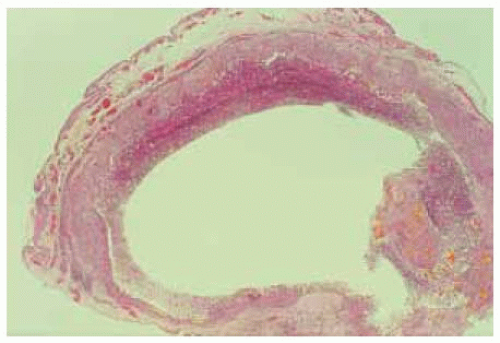 Figure 24.10. Photom icrograph show ing clear space that w as filled with blood products before their liberation at surgery and during histopathologic processing. (Hematoxylin-eosin 5.) |
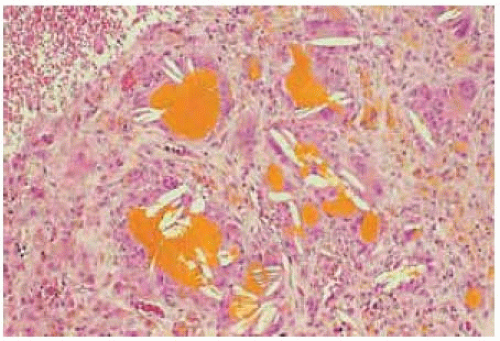 Figure 24.11. Histopathology from wall of cystoid lesion showing foreign body giant cells surrounded by cholesterol clefts and golden yellow hematoidin pigment. (Hematoxylin-eosin 100.) |
Conjunctival Foreign Bodies
General Considerations
Several types of foreign body can lodge in the conjunctiva and simulate a neoplasm (1,2,3,4,5). It can result from overt trauma or it can be present without an antecedent history of injury. It is most frequent in carpenters, construction workers, and others with occupations that might subject them to foreign objects. It is important to take a careful history when a foreign body is suspected because the lesion may be noticed many years after the trauma, which may have been forgotten by the patient. Metallic foreign bodies are often dark in color and can be clinically confused with primary acquired melanosis or circumscribed melanoma (1).
A peculiar form of foreign body is the synthetic fiber granuloma (2,3). It results from the implantation of filamentous synthetic fibers in the conjunctival fornix. It is most often seen in infants and young children who sleep in close contact with toys, such as teddy bears, that have synthetic fibers containing titanium, barium, or zinc.
Clinical Features
The clinical appearance of a conjunctival foreign body varies with the type of foreign object. Clinically, a metallic foreign body can be black, brown, or gray, suggesting a primary melanoma or extraocular extension of a uveal melanoma. Mascara pigment used to accentuate the eyelashes can rarely imbed in the conjunctiva and simulate a melanoma (4). It is an irregular mass that appears to contain hairs, sometimes suggesting a dermoid, dermolipoma, or caterpillar hairs. However, the hairlike structures are actually synthetic fibers from the toy.
Pathology
The pathology of a conjunctival foreign body necessarily varies with the type of object. Most foreign bodies are birefringent with polarized light. With regard to the synthetic fiber granuloma, the hairlike fibers induce an intense granulomatous inflammatory reaction with foreign body giant cells surrounding the foreign material.
Management
Treatment is generally surgical removal. A small, asymptomatic foreign body can be observed without surgical excision.
Selected References
1. Guy JR, Rao NA. Graphite foreign body of the conjunctiva simulating melanoma. Cornea 1986;4:263-265
2. Marr BP, Shields CL, Federici TJ, et al. Conjunctival foreign body simulating malignant melanoma. Am J Ophthalmol. In press.
3. Weinberg JC, Eagle RC, Font RL, et al. Conjunctival synthetic fiber granuloma. A lesion that resembles conjunctivitis nodosa. Ophthalmology 1984;91:867.
4. Shields JA, Augsburger JJ, Stechschulte J, et al. Synthetic fiber granuloma of the conjunctiva. Am J Ophthalmol 1985;99:598-600.
5. Shields JA, Marr BP, Shields CL, et al. Conjunctival mascaroma masquerading as melanoma. Cornea 2005;24:496-497.
6. Shields CL, Demirci H, Marr BP, et al. Expanding MIRAgel(tm) scleral buckle simulating an orbital tumor in 4 cases. Ophthal Plast Reconstr Surg 2005;21:32-38.
Conjunctival Foreign Body
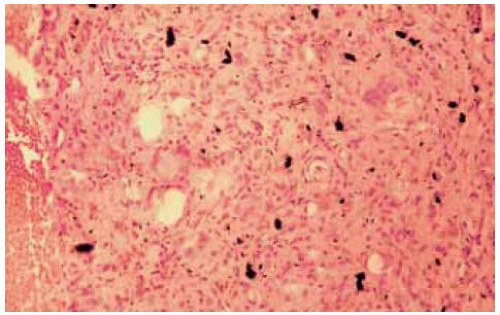 Figure 24.14. Histopathology of the lesion in Figure 24.14 show ing tissue containing m etallic fragm ents that stained positive for iron. (Hem atoxylin-eosin 100.) |
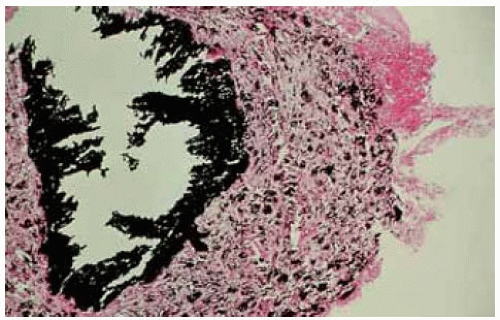 Figure 24.16. Histopathology of the lesion seen in Figure 24.15 showing inflam m atory reaction around lead foreign body. (Hem atoxylin-eosin 15.) |
Conjunctival Foreign Body
M iscellaneous foreign m aterials can occur in the conjunctiva and sim ulate a neoplasm . Unusual exam ples are show n of synthetic fiber granulom a, M IRAgel retinal detachm ent im plant, and m ascara sim ulating m elanom a.
1. Shields JA, Augsburger JJ, Stechschulte J, et al. Synthetic fiber granuloma of the conjunctiva. Am J Ophthalmol 1985;99:598-600.
2. Shields CL, Demirci H, Marr BP, et al. Expanding MIRAgelT scleral buckle simulating an orbital tumor in 4 cases. Ophthal Plast Reconstr Surg 2005;21:32-38.
3. Shields JA, Marr BP, Shields CL, et al. Conjunctival mascaroma masquerading as melanoma. Cornea 2005;24:496-497.
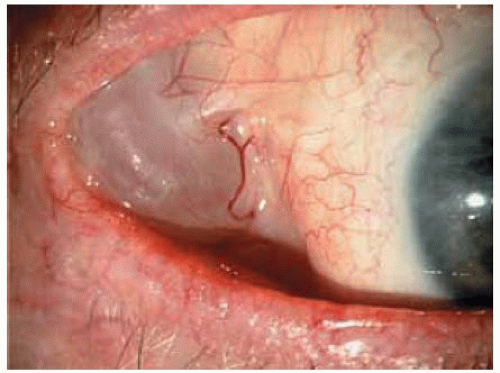
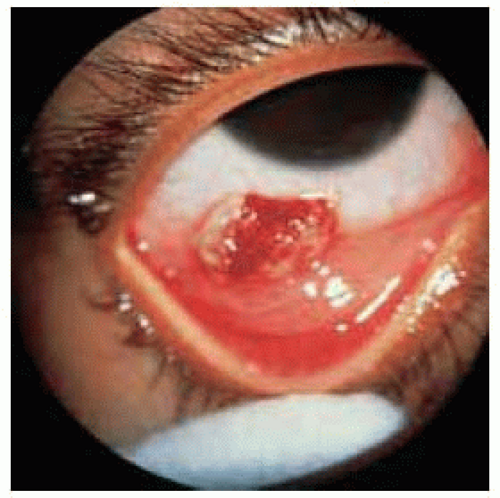 Figure 24.19. Synthetic fiber granuloma in the inferior conjunctiva in a 26-month-old child. The child had slept with a toy teddy bear. |
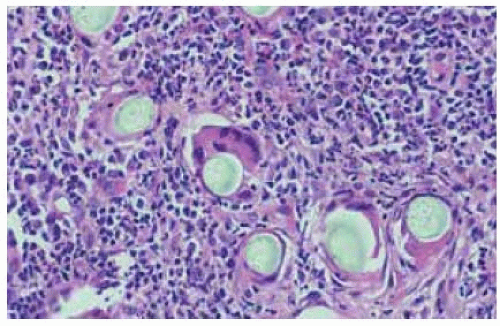 Figure 24.20. Histopathology of lesion shown in Figure 24.19. Note the hairlike structures that are inducing a foreign body inflam m atory response with giant cells. (Hematoxylin-eosin 40.) |
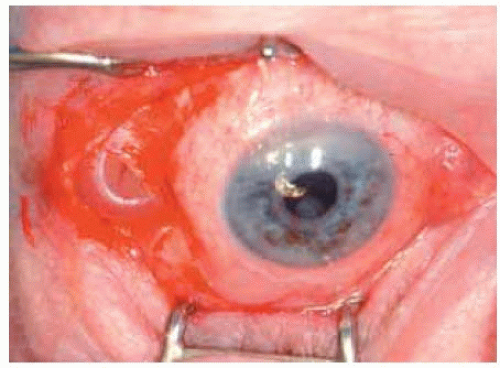 Figure 24.22. M IRAgelTM im plant show n in Figure 24.21 exposed at time of surgical removal. |
 Figure 24.23. M ascara deposit (m ascarom a) near lim bus sim ulating conjunctiva melanoma in a patient who used excessive mascara. |
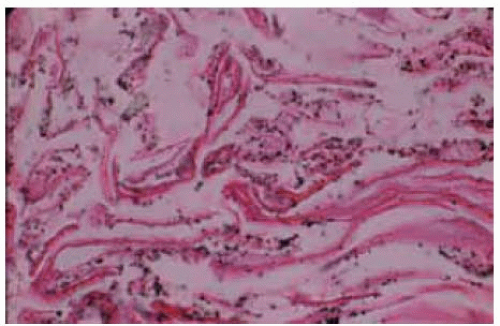 Figure 24.24. Histopathology of mascara deposit showing deposition of m ascara in superficial layer of keratin corresponding to the black lesion seen clinically in Figure 24.23. (Hem atoxylin-eosin 50.) |
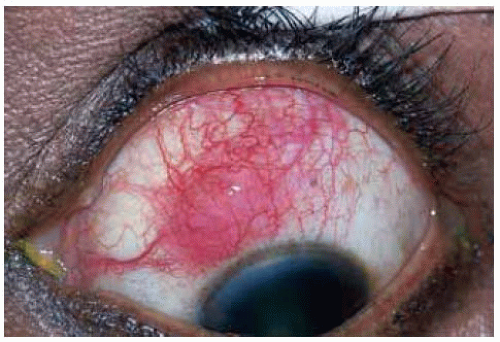
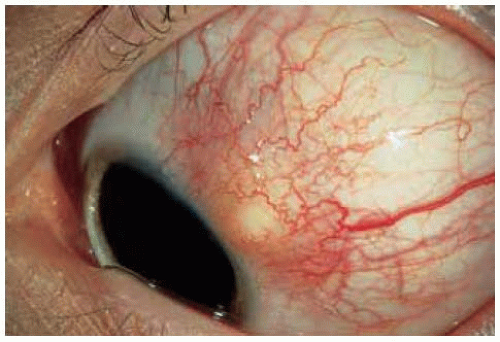
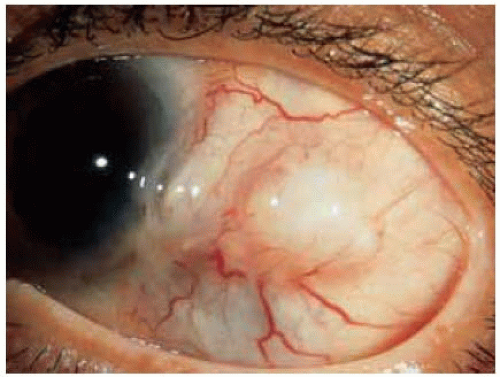
Episcleritis and Scleritis Simulating Neoplasms
General Considerations
Episcleritis and scleritis can be elevated and vascular, and simulate an amelanotic conjunctival neoplasm, particularly conjunctival squamous cell carcinoma. Nodular episcleritis is a benign, often painful inflammatory condition. It is idiopathic in most instances, but can be related to several inflammatory conditions, including rheumatoid arthritis. It lasts about 2 to 3 weeks, after which it spontaneously resolves. It has a tendency to recur.
Clinical Features
The acute onset and progression and the associated pain are usually sufficient to differentiate episcleritis from a primary neoplasm, which is usually nonpainful and more slowly progressive. One tumor that can have a similarly rapid onset and pain is metastatic carcinoma to the conjunctiva, which is a rare condition. Episcleritis can be localized (nodular) or diffuse (1).
Scleritis is often a deeper inflammation that may be granulomatous or nongranulomatous in nature. Almost half of affected patients will be found to have other systemic disease, particularly connective tissue disease such as rheumatoid arthritis. Other cases remain idiopathic despite systemic evaluation (2). Scleritis can lead to scleral necrosis and secondary uveal staphyloma. The typical appearance and associated systemic findings should help to differentiate scleritis from neoplasm. In some instances, however, a necrotic intraocular melanoma can produce secondary inflammation of the sclera and adjacent tissues. Hence, a patient with scleritis should undergo a fundus examination to exclude the possibility of an intraocular neoplasm.
Pathology
Depending on the state of the disease, episcleritis or scleritis can have acute or chronic inflammatory cells and may have signs of granulomatous inflammation with epithelioid and giant cells.
Management
The patient with suspected episcleritis should be evaluated for the known causes of inflammation, such as rheumatoid arthritis and other known granulomatous inflammations. If the lesion does not resolve on systemic or topical corticosteroids, then excisional biopsy may be warranted.
Selected References
1. Watson PG. The diagnosis and management of scleritis. Ophthalmology 1980;87:716-720.
2. Rao NA, Marak GE, Hidayat AA. Necrotizing scleritis. A clinicopathologic study of 41 cases. Ophthalmology 1985;92;1542-1549.
Episcleritis and Scleritis
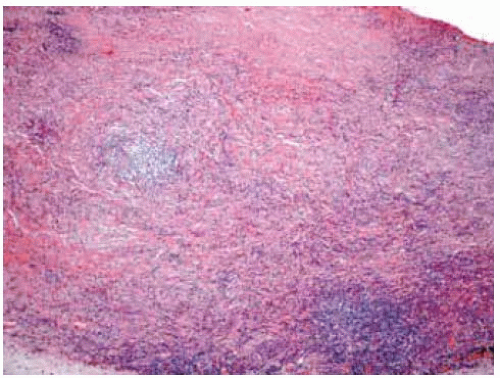 Figure 24.30. Histopathology of lesion shown in Figure 24.29 revealing diffuse infiltration of chronic inflammatory cells in the sclera. The patient had no systemic diseases that could be related to the ocular process. (Hematoxylin-eosin 50). |
Conjunctival Churg-Strauss Allergic Granulomatosis Simulating Conjunctival Neoplasm
General Considerations
Churg-Strauss syndrome is an uncommon systemic disease characterized by asthma, eosinophilia, and vasculitis (1,2,3,4,5,6). Systemic involvement can lead to renal and cardiac failure as well as peripheral neuropathy, and often has a fatal outcome. The differentiation of Churg-Strauss syndrome from vasculitides like Wegener’s granulomatosis and periarteritis nodosa have been described (2). Conjunctival involvement is now known to be a feature of Churg-Strauss syndrome, in which case it can simulate a neoplasm (2,3,4,5,6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree