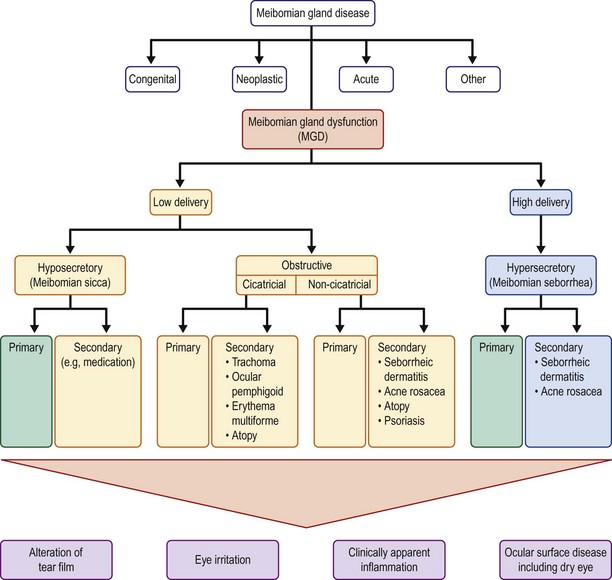
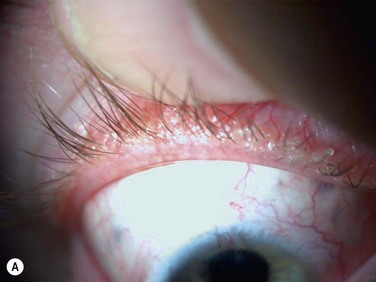
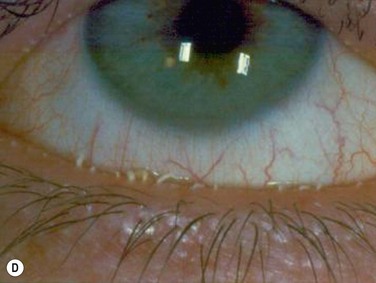
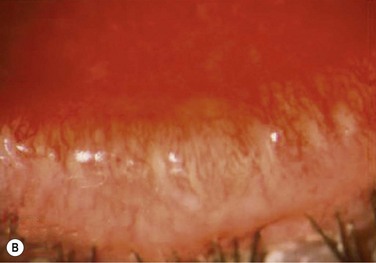
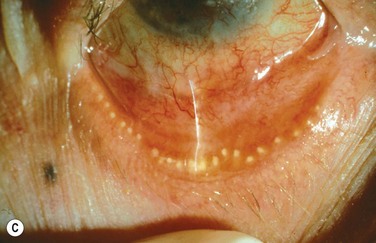
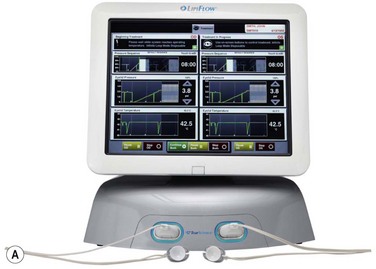
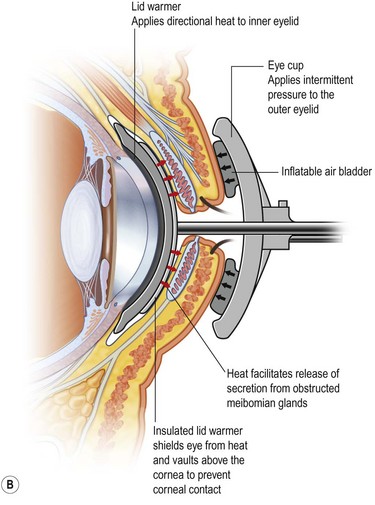
10 Meibomian gland disease is one of the most commonly encountered clinical problems and can occur as focal or diffuse involvement of the meibomian glands. Meibomian glands are anatomically located in the tarsal plate of both upper and lower eyelids, as holocrine sebaceous glands that open directly on the eyelid margin and discharge their entire contents onto the lid margin. A full description of the anatomy and physiology of the glands is provided in the Report of the Meibomian Gland Workshop published in 2011.1 The meibomian gland is a type of sebaceous gland and it is susceptible to disease entities that affect all sebaceous glands, such as seborrhea and rosacea.1 Since obstruction of the gland orifice and alteration of the meibomian secretion are the predominant pathophysiological causes of disease, management of the clinical problem centers around relief of obstruction and modification of the abnormal secretion, as well as control of inflammation when it occurs as part of the disease process. The etiology of meibomian gland disease can be congenital or acquired. A classification system proposed by the International Workshop on Meibomian Gland Dysfunction is depicted in Figure 10.1.2 Congenital absence of the meibomian gland occurs and is particularly severe in association with anhidrotic ectodermal dysplasia.3 Acquired disease occurs as both focal (internal hordeolum or chalazion) or diffuse (meibomian gland dysfunction: MGD) involvement. Although obstruction of the glandular orifice is the likely first event, the clinical appearance is very different, as the internal hordeolum (Fig. 10.2) is the result of an acute bacterial infectious inflammation, while chalazion (Fig. 10.3) is the result of a chronic localized lipogranulomatous inflammation, and meibomian gland dysfunction (MGD) (Figs 10.4 and 10.5) is primarily obstructive with variable inflammatory reaction and typically no active infectious component, although lid margin flora may influence metabolism of the meibum secretion.4 Thus, the management of the various clinical manifestations of meibomian gland disease differs in both the pathophysiological target and recommended therapy. Figure 10.4 (A) MGD with epithelial obstruction of meibomian gland orifice. (B) MGD with meibomian gland secretion turbidity. (Reproduced with permission of Elsevier. From Foulks GN, Bron AJ. Meibomian Gland Dysfunction. A Clinical Scheme for Description, Diagnosis, Classification, and Grading. The Ocular Surface 2003;1:107–26.) (C) MGD with meibomian gland secretion that is turbid with clumps. (D) MGD with meibomian gland secretion that is paste consistency. Figure 10.5 (A) Chronic MGD change of telangiectasia of eyelid margin. (B) Chronic MGD with cicatricial obstruction of meibomian gland orifice. (Reproduced with permission of Elsevier. From Foulks GN, Bron AJ. Meibomian Gland Dysfunction. A Clinical Scheme for Description, Diagnosis, Classification, and Grading. The Ocular Surface 2003;1:107–26.) (C) Chronic MGD with posterior traction of meibomian gland orifice due to cicatricial change. (Reproduced with permission of Elsevier. From Foulks GN, Bron AJ. Meibomian Gland Dysfunction. A Clinical Scheme for Description, Diagnosis, Classification and Grading. The Ocular Surface 2003;1:107–26.) Since internal hordeolum is acute suppurative inflammation of the meibomian gland, antibiotic therapy of the infectious component and anti-inflammatory therapy to control the acute inflammation are both appropriate treatments. Relief of obstruction of the gland is also important. The infecting organism is most often Staphylococcus but other bacteria can be present.5 No good comparative clinical trials have been published to compare effectiveness of treatment options for internal hordeolum,6 but the use of topical antibiotic drops or ointments includes topical erythromycin, bacitracin, tobramycin, or fluoroquinolones. In adults with severe or recurrent disease, oral doxycycline can be prescribed as systemic therapy. Application of warm compresses periodically during the day helps to reduce inflammation and encourages the infection to localize to a point which may spontaneously erupt to relieve the obstruction. Occasionally, surgical lancing of the pointing hordeolum speeds resolution. Anti-inflammatory therapy with topical corticosteroid can be helpful when inflammation is severe. Since chalazion is a chronic focal reaction of the tissue to altered lipid components of meibum occurring in an obstructed gland, the primary therapy is first anti-inflammatory. Warm compresses and massage of the eyelid are a usual first step but this alone is often not curative.7 Antiinflammatory therapy with topical corticosteroid drops can reduce inflammation but the chronic granulomatous nature of the inflammatory response may not completely resolve with topical therapy. Intralesional steroid injection has been advocated to reduce inflammation.7–9 In recalcitrant cases, evacuation of the chalazion by surgical incision and curettage is necessary.10 Randomized controlled clinical trials have been published that compare efficacy and safety of treatment options and show that treatment with intralesional steroid is as effective as incision and curettage (84 % versus 87%, respectively) in contrast to the conservative management with hot compresses, that resulted in only a 46% resolution.8,9 Repeatedly recurrent or unusually irregular lid lesions mimicking chalazion can be more difficult to diagnose and can certainly be more dangerous, as they are neoplasms of the meibomian gland. It is, therefore, wise to submit curettage specimens for histopathological evaluation in recurrent or unusual circumstances. Sebaceous cell carcinoma is the most worrisome lesion to be identified, but intratarsal keratinous cysts are also an uncommon etiology of a lesion mimicking chalazion.11,12 Meibomian gland dysfunction is probably the most common affliction of the meibomian glands and the pathophysiology is amply described in the MGD Report of 2011.1 Obstruction of the meibomian gland orifice by keratinized epithelium or thickened abnormal secretion is the primary initiating pathological event.1,13 Therefore, relief of obstruction is a central goal of therapy. The obstruction of the meibomian gland orifice can be visualized in many cases of MGD but as Blackie, Korb and others have emphasized, nonobvious obstruction is frequent and expression of the eyelid glands as part of the physical examination is essential to diagnosis (Fig. 10.6).14 Including expression of the meibomian glands as part of the routine evaluation of the eyelids during an eye examination, is a pivotal recommendation of the MGD Report. Mechanical options for treatment typically begin with application of warm compresses, two or more times daily, followed by firm massage of the eyelids.15 A variety of techniques have been advocated but one effective, simple approach is well described.15 Other techniques are described in the MGD Report.16 Warming of the eyelid has been accomplished by application of a washcloth soaked in hot water, but more elaborate methods have also been described. Heating a washcloth or a potato in a microwave oven has been advocated to provide a lasting heat, but overheating can occur and lead to burns of the facial skin.17 Reports from the Japanese literature describe heating of the eyelids with an infrared lamp, applied as a controlled mask.18 The application of warm, moist air or steam has also been evaluated.19 A novel approach to application of controlled temperature concurrent with mechanical expression of the eyelids is the Lipiflow™ system, which utilizes pulsed compression of the eyelids during continuous monitored thermal control (Fig. 10.7).20 Figure 10.7 (A) Illustration of the Lipiflow™ System that provides monitored temperature warming and intermittent pulsation of the eyelids. (Courtesy of Tear Sciences, Inc; Morrisville, North Carolina.) (B) Cross-sectional view of Lipiflow™ System when applied to eyelid. (www.tearscience.com/physician/in-officeprocedure/lipid-science (accessed Jan., 2013) ) Meibum is a complex mixture of various polar and nonpolar lipids containing cholesteryl esters (CEs), triacylglycerol, free cholesterol, free fatty acids (FFAs), phospholipids, wax esters (WEs), and diesters.21–24 Reported alterations of the behavior and composition of meibum in MGD are summarized in Table 10.1. Changes in the composition and behavior of the meibomian gland secretion (meibum), occurring both with age and due to meibomian gland dysfunction, have been documented by a variety of spectroscopic techniques.38,39 These studies reveal that abnormal behavior of the secretion is due to increased viscosity, resulting from an elevated phase transition temperature that correlates with a higher degree of ordering of the lipid molecules (Fig. 10.8).40 These abnormal properties of the altered meibum can be reversed with several pharmacological therapies (Fig. 10.9).4,41–43 Tetracycline-class drugs (tetracycline, doxycycline, and minocycline) have been shown to alter the abnormal meibum, presumably by interfering with lipase enzymes that degrade the normal lipids into smaller diglycerides.4 Doxycycline has been shown to produce a number of other changes in lipid composition and the presence of caratenoids in the meibum.39 Azithromycin applied topically to the eye and eyelid over a month of therapy is a very effective agent to restore lipid behavior towards normal (Fig. 10.9).41–43 The effect is probably due to a combination of antilipase activity and anti-inflammatory activity as well.45 Table 10.1 Behavior and Composition Changes in Meibum with MGD
Meibomian Gland Disease
Treatment
Introduction
Classification of Meibomian Gland Disease



Pathophysiological Targets and Goals of Therapy
Behavior
Increased phase transition temperature
Borchman, et al. (FTIR)25
Increased ordering of lipid
Foulks, et al. (FTIR)26
Increased viscosity
Borchman, et al. (FTIR)25
Composition
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access