Thyroid cancer represents the most common endocrine cancer, and rates have been increasing over the last 3 decades. The treatment of cervical metastases in well differentiated thyroid cancer remains in evolution. Many questions require further resolution. Unlike many other malignancies, most large studies have found that overall survival is not significantly affected by regional metastases. On the other hand, several studies have noted that regional disease may decrease survival in selected patient groups. The greatest effect of lymph node metastases seems to be an increase in recurrence rates. Except for the compartment-oriented removal of clinically positive nodes, few strong recommendations may be made.
Thyroid cancer represents the most common endocrine cancer, and rates have been increasing over the last 3 decades . Questions remain as to whether this increased incidence represents a true change in disease patterns or rather an improvement in detection of previously subclinical disease. Regional lymph node metastasis rates are high, ranging from 30% to 80% . Despite this, papillary thyroid cancer is associated with a 93% to 98% 10-year survival rate .
Authors disagree on the effect of nodal metastasis on survival. Numerous studies have found no statistically significant decrease in long-term survival in the presence of regional disease . Conversely, a recent large case-control study of 5123 patients in Sweden reveled a 2.5-times risk for disease-related death in the setting of regional metastases . Several reports have shown a decrease in survival associated with regional metastases when select patient groups are examined. Hughes and colleagues found, in a case matching study of 100 patients, that although overall there was no significant difference in survival between patients who had N1 disease versus those who had N0 disease, in patients older than age 45 years, a trend toward decreased 20-year survival was found. Scheumann and colleagues , in a series of 324 patients, found regional metastasis had a significant effect on survival and recurrence especially in those who had primary tumors staged T1 to T3. Sugitani and colleagues found, in patients who had papillary microcarcinoma (primary tumor size <1.0 cm) with palpable lymphadenopathy of at least 1 cm in size, the disease-specific survival rate was 72%, which compares poorly with the previously noted greater than 90% survival rate. Nodal size greater than 3 cm and extracapsular spread were particularly poor prognostic signs. Kitajiri and colleagues also found nodal metastases greater than 3 cm in size to be associated with significantly worse overall survival.
Thyroid lymphatic drainage
The thyroid gland sits in its position in the central neck, affixed to the anterior and lateral walls of the trachea. Lymphatics, for the most part, follow venous drainage patterns into level VI, or the central lymph node compartment (cervicocentral compartment) . This lymph node level is unpaired and is bound superiorly by the hyoid bone, laterally by the carotid arteries, and inferiorly by the sternal notch. Subdivisions of level VI include the pretracheal, paratracheal, precricoid (delphian), and supramediastinal nodes . These regions are believed to represent the first echelon of nodal drainage and metastasis in well-differentiated thyroid cancer.
The next logical step of metastatic progression from level VI is to the nodal regions of levels II to IV or the deep jugular nodes (lateral cervical compartment). Pathologic studies have not fully borne out findings of consistent progression. Several studies including both central and lateral cervical nodal dissections have found a small but substantial rate (2%–19%) of lateral metastases without intervening ipsilateral central nodal metastases. These “skip metastases” may imply a route of lymphatic spread directly from the thyroid gland to the lateral cervical compartment, thus bypassing the central compartment . Conversely this apparent phenomenon may represent a failure of current means to detect micrometastases in the central compartment.
Characteristics of lymph node metastasis in papillary thyroid cancer
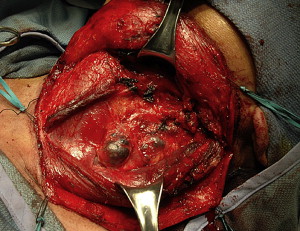
Cervical lymph node ultrasound findings have been well correlated with the likelihood of metastases in thyroid carcinoma. Approximately 40% (reported range, 21%–50%) of all lymph node metastases from papillary thyroid carcinomas may completely cavitate by cystic degeneration. As a result, these nodes may mimic apparently benign cervical cysts (branchial cleft cysts, and so forth). Wunderbaldinger and colleagues aspirated fluid from 78 cystic lymph nodes, and 80% were found to contain either dark and viscous or bloody fluid with elevated thyroglobulin levels. This fluid discoloration may explain the finding of grossly dark blue-black or purple lymph node metastases from papillary thyroid carcinomas ( Fig. 1 ). Other radiographic findings in lymph node metastases from papillary thyroid carcinomas include irregular borders, internal heterogeneity, calcifications, lack of an echogenic hilum, and hypervascularity .
Characteristics of lymph node metastasis in papillary thyroid cancer
Cervical lymph node ultrasound findings have been well correlated with the likelihood of metastases in thyroid carcinoma. Approximately 40% (reported range, 21%–50%) of all lymph node metastases from papillary thyroid carcinomas may completely cavitate by cystic degeneration. As a result, these nodes may mimic apparently benign cervical cysts (branchial cleft cysts, and so forth). Wunderbaldinger and colleagues aspirated fluid from 78 cystic lymph nodes, and 80% were found to contain either dark and viscous or bloody fluid with elevated thyroglobulin levels. This fluid discoloration may explain the finding of grossly dark blue-black or purple lymph node metastases from papillary thyroid carcinomas ( Fig. 1 ). Other radiographic findings in lymph node metastases from papillary thyroid carcinomas include irregular borders, internal heterogeneity, calcifications, lack of an echogenic hilum, and hypervascularity .
Rates of and distribution of cervical metastasis
Wada studied the metastasis patterns associated with the papillary microcarcinomas (primary tumors <10 mm in size). The rates of pathologic metastasis to the central and lateral compartments were 64% and 45%, respectively. A 5% skip metastasis rate was noted. Central neck nodes were more commonly found in the pretracheal (43%) and ipsilateral paratracheal (36%) compartments than in contralateral sites (19%). In the lateral neck, mid-lower levels nodes or level III to IV (38%) were more commonly involved than upper nodes (22%). The posterior triangle, level V, was rarely involved (3%) . In a later study, Wada and colleagues found that for primary tumors greater than 10 mm in size, central nodal metastases were found in 76%. Lateral nodal metastases were found in 65%, with 7% of patients exhibiting skip metastases.
Shaha reported on a series of 1038 patients who had well-differentiated thyroid cancer over 55 years at Sloan-Kettering Cancer Center. Overall, 56% of patients had clinically evident regional metastases at the initial evaluation. These were further broken down by primary tumor pathology. Reported nodal metastasis rates were 61% for papillary carcinoma, 30% for follicular carcinoma, and 21% for Hürthle cell tumors respectively.
Roh and colleagues reported the distribution of lateral neck metastases in 22 patients; 91% of patients had metastases in the mid-lower jugular nodes, 45% in the upper jugular nodes (level II), and 18% in posterior triangle nodes. In a separate group of 155 patients, Roh performed a total thyroidectomy, central neck dissection, and in cases with clinical evidence, a lateral neck dissection. The rate of positive nodes for the central and lateral neck was 62% and 25.6%, respectively. Lateral skip metastases were noted in 2.4% of patients .
Lee and colleagues reported on 167 patients who had clinically positive lateral necks. The metastasis rate was level II (62%), level III (81%), and level IV (75%), respectively. The level IIb rate specifically was noted to be 7%. Machens found a lateral neck skip lesion rate of 20% in patients who had papillary carcinoma. Skip lesions were not found associated with follicular carcinoma.
Gimm and colleagues found a 68% central compartment metastasis rate in 35 patients. All positive nodes were found on the side ipsilateral to the primary tumor. Ito and colleagues reported a similar central compartment metastasis rate of 63%. Shindo and colleagues studied 100 patients who had undergone total thyroidectomy with central neck dissection. Pathologically confirmed metastasis rates differed with respect to age less than or greater than 45 years, at 29% and 39%, respectively.
Qubain and colleagues examined neck dissection specimens in 80 patients who were clinically negative for nodal metastases using immunohistochemical stains for cytokeratins (AE1/AE3). Micrometastases were found in 53% of patients. The rate was influenced by primary tumor size, with micrometastasis being observed in 26% of patients who had primary tumors 1.0 cm or smaller and in 66% who had tumors greater than 1.0 cm. Attie and colleagues found a similar rate (69%) of micrometastases in patients otherwise noted to be clinically negative.
In a cohort of 31 patients, Machens and colleagues found ipsilateral central and lateral metastasis rates were 29% and 29%, respectively. Contralateral metastasis rates for central (13%) and lateral (3%) were uncommon, and were found to increase with increasing primary tumor size. Mirallié and colleagues found a high rate of cervical metastasis at 61%, with 40% of patients demonstrating bilateral involvement. The ipsilateral paratracheal nodes were the most common site involved (50%).
Retropharyngeal nodes represent a rare site of nodal metastasis in thyroid cancer. Approximately 23 cases have been reported in the literature. In most cases, the retropharyngeal metastasis was associated with other cervical metastases, likely representing alteration of normal pattern of lymph flow secondary to these other metastases .
Central neck dissection
Central neck dissection (CND), as is implied by the name, involves removal of nodal tissue from the central neck compartment, or level VI ( Figs. 2 and 3 ). This level is considered a midline unpaired nodal basin, and remains the most common site of metastasis in well-differentiated thyroid cancer. Compared with total thyroidectomy alone, CND imparts greater risks to the parathyroid glands and recurrent laryngeal nerve.
In a case-control study 195 patients underwent central neck dissection. Ten-year survival rates were significantly improved in the study group (98.4%) compared with the control group (88.9%–91.6%) . A recent review by White and colleagues recommended central lymph node dissection in well-differentiated thyroid cancer, finding a trend of decreased recurrence and increased survival.
The American Thyroid Association released guidelines in 2006 consideration of a routine central neck dissection for papillary thyroid carcinoma and suspected Hürthle cell carcinoma. Other authors argue that postoperative radioactive iodine therapy instead of CND may provide an alternative approach for papillary thyroid carcinoma and Hürthle cell carcinoma .
If a central neck dissection is to be performed, must both sides of the central compartment be addressed? Lee and colleagues studied a group of 103 patients who had primary papillary thyroid tumors less than 2 cm in size. Patients underwent either unilateral or bilateral CND. Therapeutic effect, noted in this case by posttreatment thyroglobulin levels, was not significantly different between the treatment groups. Patients undergoing bilateral dissection had a significantly higher rate of hypocalcemia, which would seem to argue for elective unilateral CND in the setting of smaller (<2 cm) primary tumors.
Lateral neck dissection
Current American Thyroid Association recommendations advocate lateral neck compartment node dissection for patients who have evident cervical metastases, whether detected clinically, pathologically, or by imaging. Additionally, lateral neck dissection is recommended for patients deemed likely to fail radioactive iodine therapy, based on lymph node size, number, and other factors, such as an aggressive primary tumor . Scheumann and colleagues found that compartment-oriented neck dissection was associated with improved survival and decreased recurrence rates.
What extent of dissection should be performed in the treatment of lateral neck metastases? Pingpank and colleagues studied 55 patients undergoing neck dissection for well-differentiated thyroid cancer. Nodal metastases were found to be confined to a single level in only 20% of neck dissection specimens. Some 14% of specimens demonstrated metastases in four or more nodal levels. These findings are consistent with recommendations against “berry-picking,” or superselective neck dissection, secondary to concerns that this may lead to a higher rate of missed disease and recurrence.
Conversely, Battacharyya argues for a more selective approach, removing only clinically apparent nodes. Surveillance, Epidemiology, and End Results (SEER) data were used to compare 880 patients who had undergone “limited lymphadenectomy” versus 1217 who had undergone compartment-based neck dissection. All patients underwent postoperative radioactive iodine therapy. No significant difference was noted in 5-year survival rates, which were 94.4% and 95.9%, respectively. Recurrence rates were not reported .
Turanli compared the results of 61 patients who had lateral neck metastases undergoing selective lateral neck dissection (levels II–IV) versus modified radical neck dissection. No significant differences were found between the groups with respect to disease-free survival, overall survival, or local recurrence at an average of 80 months of follow-up. Lee and colleagues advocates inclusion of level IIb in the presence of clinically apparent level IIa nodes.
Treatment of the clinically N0 neck remains a topic of debate. Studies of clinically negative necks have found high rates of occult metastases. Wada and colleagues reported occult metastasis rates of 61% for the central compartment and 40% for the lateral compartment. Regional differences in treatment patterns are seen, particularly when comparing centers in the United States with Japan. In the latter, elective neck dissection is much more commonly applied in the setting of well-differentiated thyroid cancer. This difference may be a function of less frequent use of radioactive iodine therapy in Japanese centers . Both Wada and Ito reported on large groups of patients, 235 and 523, respectively, undergoing thyroidectomy with or without elective lateral neck dissection. Neither study found a significant difference in recurrence rates between the two groups. In a study of 464 patients who did not have preoperative evidence of cervical metastases, Wang and colleagues found only a 3% cervical recurrence rate. These results suggest that occult metastases may not necessarily represent clinically concerning -lesions, particularly in the setting of routine radioactive iodine therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


