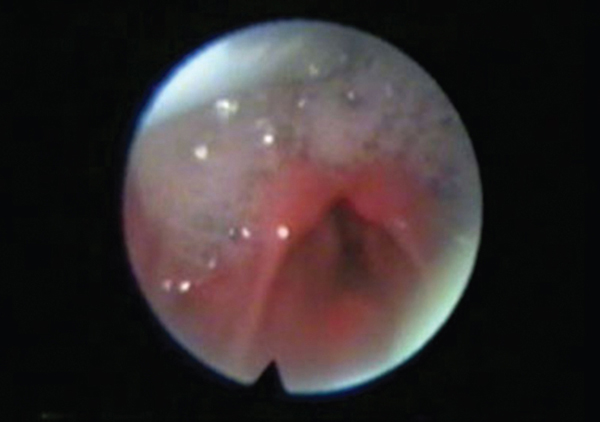
34 Management of Dysphagia Swallowing disorders presenting to an ENT outpatient department are not uncommon. However, many patients do not get the attention they deserve. Inadequate understanding of the pathophysiology may probably lead indifference on the part of the physician toward the swallowing problem. In this chapter, we will look at the common swallowing problems that may be encountered by the ENT surgeon. However, a discussion of infective and neoplastic causes is beyond the scope of this chapter. Muscles of the lips and adjacent facial muscles such as buccinators supplied by the facial nerve play major role in the oral stage of swallowing. Muscles of mastication supplied by the trigeminal nerve are the key to the oral preparatory phase. Tongue muscles with innervation from the hypoglossal nerve are indispensible for both oral and pharyngeal stages. Sensations transmitted through nerves, such as lingual, chorda tympani, and glossopharyngeal, are also very important for the normal swallowing act. Pharynx, with its three constrictor muscles, has to play the most complex of the three stages. Of the three constrictors, inferior constrictor is the most important yet least understood. It has two parts, namely thyropharyngeus and cricopharyngeus. The space between the two is Killain dehiscence—a potential space for herniation. The constrictors are supplied by the pharyngeal plexus, and cricopharyngeus gets innervations from recurrent laryngeal nerve. The interesting part about the cricopharyngeus is the fact that it is in a state of tonic contraction and relaxes only during the act of swallowing. We do not know of a mechanism wherein a muscular relaxation occurring with acetylcholine-mediated nerve stimulation occurs. It is quite possible that some central mechanisms play a role.1 Facial palsy will result in improper closing of the lips and inadequate obliteration of the oral vestibule. As a result, part of the food can spill out of the oral cavity and part can get trapped in the vestibule. Bilateral facial palsy will cause even greater problems. Buccinator weakness will result in stasis of food in the oral vestibule. Trigeminal nerve involvement will affect the chewing mechanism and, consequently, the preparatory phase will be compromised. Bilateral hypoglossal palsy can result in severe swallowing problem both at the oral and at the oropharyngeal levels. However, unilateral hypoglossal nerve palsy, unless accompanied by other neurological deficits, rarely produces major swallowing problems. Surgical resection of lips and or tongue can result in significant morbidity of the swallowing mechanism. If commissure of the lips is resected, then morbidity will be even more. Total glossectomy (Fig. 34.1) makes the act of swallowing extremely difficult, if not impossible. Partial glossectomy generally does not produce as much dysphagia. Reconstruction procedures also affect the swallowing efficiency. While an optimum-sized flap will obliterate the vacuum created by the surgery and improve the swallowing, a poorly designed over-sized flap will hamper the act of bolus transit. Floor of mouth cancers requires removal of varying degrees of muscles of the floor of mouth as well as part of the mandible. If symphysis menti is resected, then hyomandibular complex will be disrupted resulting in severe swallowing difficulty.2 Mandibular arch, mylohyoid muscles and raphe, geniohyoid muscles, and hyoid bone constitute the hyomandibular complex. As in the case of glossectomy, here also the type of reconstruction is important for the swallowing outcome. Hard palate resections are the least problematic of the lot as far as the swallowing is concerned. A suitable prosthesis will effectively eradicate any problem with swallowing in these cases. Apart from history taking, ENT and neurological examination, watching the act of swallowing is very important. Many a time, it gives the physician not only an idea about the pathophysiology, but also about the possible therapeutic strategies. Videofluoroscopic assessment of the swallowing act with radio opaque substances such as barium or Gastrografin is the most important diagnostic tool in oral dysphagia. Both anteroposterior and lateral views are important in this regard. Tongue muscle dysfunction, stasis of bolus in the vestibule, and their potential corrective strategies can be detected from the fluoroscopy. Swallowing therapy techniques are the mainstay of treatment in oral dysphagia in vast majority of the cases. There are direct as well as indirect swallowing therapy techniques. Indirect swallowing therapy aims at improving the swallowing function without attempting to feed the patient. Improving the tongue movements, improving the lip closure by strengthening the lips, and maximizing the power of the masticatory muscles are examples of this.3 Direct swallowing therapy tries to orally feed the patient, with techniques designed to avoid or circumvent the swallowing difficulty experienced by the patient. For example, asking the patient to extend the head and neck while swallowing so that gravity helps to send the bolus down is a direct swallowing therapy technique. Using specially designed spoons or tubes to directly place the food into the pharynx is another direct swallowing therapy technique. Changing the texture of the feeds can solve the problem to a great extent in many cases. Vast majority of the patients having oral dysphagia can be managed satisfactorily with direct or indirect swallowing therapy techniques or both. Some of them however require temporary or permanent nonoral modes of feeding such as nasogastric tube, gastrostomy, or jejunostomy feeding. Bilateral hypoglossal paralysis, as we have already seen, will affect the swallowing considerably, both at the oral and oropharyngeal stages. The propulsion of the bolus by the tongue base will not take place, if the tongue is paralyzed. Parkinsonism is a condition that can adversely affect the oropharyngeal and laryngopharyngeal stages of swallowing.4 Many of these patients show on videofluoroscopy, what is known as the “swing” movement of the tongue. Here, as the bolus reaches the oropharynx, the posterior third of tongue raises and sends the bolus back to the oral cavity. This to and fro movement goes on for a long-time swing—the swing effect during barium swallow videofluoroscopy. Palatal paralysis, especially bilateral cases, causes incomplete velopharyngeal closure and results in nasal regurgitation. Cerebral palsy children may have drooling of saliva, secondary to reduced frequency of swallowing. In these patients, both oral and oropharyngeal stages may be affected. Surgical resection of the tongue base—unilateral or bilateral—will cause significant swallowing problems. Palatal excisions can cause nasal regurgitation and swallowing difficulty. Dysphagia due to tongue base paralysis or total glossectomy is one of the most difficult swallowing disorders to correct. By altering the feeding position and using specially designed feeding spoons, this may be partly corrected. Pumping in semisolid diet into the oropharynx with a 50-cc syringe through a polythene cannula is a simple, inexpensive yet efficient mode of feeding these patients. Swallowing problems in parkinsonism respond well to antiparkinsonism treatment. Masako maneuver is the technique wherein patient is asked to protrude the tongue and bite onto it while swallowing.5 This prevents in coordinate tongue base movements seen in the cases of parkinsonism. Drooling in cerebral palsy children can be corrected by submandibular duct relocation surgery. In this operation, both submandibular salivary ducts are dissected per orally and are relocated into the tonsillar fossae. This causes the saliva to reach the oropharynx, thus initiating the act of swallowing. The result will be even better, if this is combined with swallowing therapy. The two aspects of swallowing therapy in these patients are (1) to improve the lips closure and (2) to stimulate the swallowing act. The first is done by the button and thread exercise wherein the child is asked to keep a button anchored to a thread, inside the lips, but outside the teeth. The child is encouraged to keep the button in its position with the help of the lips against the pull of the thread, exerted by the child himself or herself. Teaching the child to initiate the act of swallowing on hearing an auditory stimulus or on seeing a visual stimulus is also very useful. This is a sort of conditioning reflex. For velopharyngeal incompetence, direct swallowing therapy involves swallowing with chin flexed and touching the chest. Pinching the nose tightly while swallowing also is a very useful method. Indirect swallowing therapy techniques for palatal incompetence include palatestrengthening exercises such as blowing balloon. A sphincter pharyngoplasty with a tight velopharyngeal port might help, though it runs the risk of causing snoring. Upper esophageal sphincter (UES) is a key area in swallowing. This is contributed by the inferior constrictor muscle. The upper part is the thyropharyngeus, and the lower part is the cricopharyngeus. The perfect harmony of their contraction and relaxation is a must for smooth swallowing. In resting state, the cricopharyngeus is in a state of tonic contraction. It will relax only when the bolus has passed beyond the thyropharyngeus. During this particular phase, the larynx will close itself, thus avoiding any possibility of aspiration. Once the bolus has passed beyond the cricopharyngeus, the muscle will contract again, and the larynx will reopen for respiration. For better understanding, laryngopharyngeal pathology may be divided into three groups, though it must be remembered that various permutations and combinations of the three can be present in each patients. They are laryngopharyngeal paralysis, laryngeal incompetence, and cricopharyngeal dysmotility. Motor neuron diseases, Parkinsonism, and stroke are known to produce laryngopharyngeal paralysis, which is the condition characterized by the absence of upward movement of the larynx during deglutition. As a result, the larynx remains unprotected, and cricopharynx fails to open.6 Extensive surgical resection involving the upper neck and the oropharynx also can result in laryngopharyngeal paralysis. Condition is diagnosed by the fact that during the attempted swallow, there is hardly any upward movement of the larynx. Videofluoroscopy confirms the diagnosis. Another useful investigation is flexible endoscopic evaluation of swallowing (FEES). In total laryngopharyngeal paralysis, this will show the entire bolus in the pyriform fossae even after many attempted swallows. This can later enter the laryngeal inlet resulting in coughing and choking episodes. In less severe forms, the amount of food bolus will be reduced after multiple swallow attempts. This is a difficult condition to treat. Two useful direct techniques in swallowing therapy are (1) Mendelssohn maneuver and (2) chin tuck. Mendelssohn maneuver involves in manually elevating the larynx, while patient attempts to swallow. This procedure results in, at least partially, closing the larynx and opening up the cricopharynx.7 The chin tuck technique uses extreme flexion of the head, resulting in opening up of the epiglottic angle. The pressure exerted on the trachea and larynx will also partly prevent aspiration. Permanently elevating the larynx by doing a mandibulohyoid suspension also is useful in this condition. Indirect swallowing therapy for this condition is suprahyoid muscle strengthening. Shaker exercise is aimed at this.8 Patient is asked to lie supine and lift the head offthe bed and keep it in that position for as long as he or she can. This is to be performed many times a day. Hemilaryngeal or total laryngeal paralysis can result in significant aspiration, especially the latter. It is important to note that bilateral recurrent laryngeal nerve palsy alone will not cause significant aspiration. Only when the superior laryngeal nerve or nerves are also involved, aspiration becomes a major problem. Cerebrovascular accidents (CVAs), head injury, and neurosurgical procedures can cause this problem. Laryngeal incompetence will cause the larynx to remain incompletely closed during the pharyngeal stage of swallowing, thus resulting in aspiration. Hemilaryngeal paralysis causing aspiration is easier to handle. Most of the young patients should be okay with swallowing therapy. For this, supraglottic swallowing technique is very useful. Here, the patient is instructed to swallow after holding the breath.9 It is important to note that patient should not be asked to take a too deep an inspiration before holding the breath. By doing so, the larynx will descend in the neck, thus keeping the glottis slightly open. Moreover, elevation of the larynx is an important stimulus to open up the cricopharyngeal sphincter. If the incompetence is severe, then super-supraglottic technique may be tried. The difference here is that patient is asked to bear down once breath is being held. It has been found that in super-supraglottic swallow, swallowing time is shorter. Occasionally, especially in older patients, swallowing therapy alone may not be sufficient. Then, a medialization thyroplasty can help by improving the efficiency of the glottic closure. If there is a big posterior glottis chink or a vertical-level asymmetry of the vocal cords, then an arytenoid rotation also will have to be performed along with the medialization thyroplasty. Total laryngeal paralysis is a formidable problem. Here, the swallowing takes a back seat, as prevention of fatal aspiration is the more pressing need. Luckily, a cuffed tracheostomy will most often solve the problem. However, occasionally one can come across a patient, who still drowns in his or her own secretions. There are a few surgical options for these patients. Laryngeal diversion is the procedure, wherein larynx and trachea are disconnected from each other. The lower end of the larynx is closed, and the upper end of trachea is brought out as the tracheostomy. Another operation is epiglottic over sew, in which the epiglottis is sutured over the laryngeal inlet as a lid. A third option is the procedure known as glottic closure. Here, the medial edges of the vocal cords are made raw and then sutured to each other. The most definite surgical procedure to prevent aspiration is total laryngectomy, though seldom resorted to. Apart from their efficacy, reversibility of the procedure also has to be taken into consideration, while choosing the procedure. While total laryngectomy is the most efficient in preventing the aspiration, it is also an irreversible procedure. Reversibility is best for epiglottic over sew followed by laryngotracheal diversion and glottis closure. By this terminology, it is meant that the cricopharynx does not open up in time, when the bolus reaches it. Even if the larynx is competent, then this condition can result in aspiration. This happens because, the bolus which is still at the level of cricopharynx, finds its way into the larynx, when the glottis open for inspiration. Cricopharyngeal dysmotility is not an uncommon problem in many a patients who suffered CVAs.10 It is especially common in Wallenberg syndrome (Fig. 34.2). Neurosurgeries of the brain stem also can cause this. Surgeries of the hypopharynx and upper esophagus can also result in this condition.
Anatomy and Physiology of Swallowing
Disorders of the Oral Stage
Neurological Causes
Iatrogenic Causes
Diagnosis
Management
Disorders of the Pharyngeal Stage—Oropharyngeal Phase
Neurological Causes
Iatrogenic Causes
Management
Disorders of the Laryngopharyngeal Phase
Laryngopharyngeal Paralysis
Management
Laryngeal Incompetence
Management
Cricopharyngeal Dysmotility
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree