20 Artemios S. Kandarakis The management of a patient with visually significant cataract and glaucoma poses a clinical challenge for an ophthalmologist. The variables to consider are the patient’s age, stage of glaucomatous damage, status of the control of glaucoma, the patient’s general health, ability to pay for treatments, noncompliance, and family or social support. Although there are no large studies on the rate of incidence of age-related cataract and glaucoma, it is reasonable to assume that with the increase in the world’s older population, there would be an increase in the number of cataract and glaucoma patients as well. Kahn et al,1 studying the Framingham population, found that among 2,477 subjects aged 52 to 85, the prevalence of senile cataract was 15.5% and that of open-angle glaucoma was 3.3%. More recently, Rahmani et al,2 studying the Baltimore Eye Survey population of 40 years of age or older, found that the prevalence of cataract was 35.3% and that of glaucoma 4.7%. Similarly, Singh et al,3 in a total of 903 persons above 50 years of age from Maharashtra, India, found the prevalence of cataract to be 40.4% and that of glaucoma to be 3.1%. The 5-year incidence of age-related cataract from the Framingham Eye Study ranged from 1% at the age of 55 to 15% at the age of 75.4 Klein et al5 estimated the incidence of cataract in the Beaver Dam Eye Study population by taking into account the prevalence of cataract at a baseline examination conducted between 1988 and 1990 and again at the follow-up examination held between 1993 and 1995. They found that incipient nuclear cataract occurred in 13.1%, cortical cataract in 8.0%, and posterior subcapsular cataract in 3.4%. The cumulative incidence of nuclear cataract increased from 2.9% in persons aged 43 to 54 years at baseline to 40.0% in those aged 75 years or older. For cortical cataract, the corresponding values were 1.9% and 21.8% and for posterior subcapsular cataract, 1.4% and 7.3%, respectively. In Europe, Dielemans et al6 in the Rotterdam Study concluded that the overall prevalence of primary open-angle glaucoma (POAG) in 3,062 participants over 55 years of age was 1.1%. It has been confirmed that the older the individual, the greater the prevalence of cataract and glaucoma.7,8 Hiller et al,7 in the National Health and Nutrition Examination Survey (NHANES), found that the risk of cataract at age 70 is 13-fold higher than that at age 50. Klein et al8 noted in the Beaver Dam Eye Study that the prevalence of glaucoma increased from 0.9% at ages 43 to 54 to 4.7% at age 75 or more. In England, Das et al9 found that, under the age of 60, Asians had a 30% prevalence of age-related cataract compared to 3% in Europeans, and 78% compared to 54% at age 60 and over. In another detailed study, Mitchell et al10 examined the prevalence and demographics of age-related cataract in an urban population of Australia. They reported that nuclear cataract involved 51.7% of the population (53.5% of women and 49.7% of men) and was found in 17.6% of persons less than 55 years of age, 34.2% of persons aged 55 to 64 years, 61.8% of persons aged 65 to 74 years, 87.3% of persons aged 75 to 84 years, and 89.6% of persons aged 85 years or older. They also reported that cortical opacities were found in 23.8% of the population (25.9% of women and 21.1% of men) and specifically in 4.4% of individuals less than 55 years of age, 13.1% of those aged 55 to 64 years, 28.4% of those aged 65 to 74 years, 46.7% of those aged 75 to 84 years, and 55.8% of those aged 85 years or older. Finally posterior subcapsular cataracts were seen in 6.3% of the population (6.2% of women and 6.5% of men) and were found in 2.7% of persons less than 55 years of age, 3.8% of those aged 55 to 64 years of age, 6.5% of those aged 65 to 74 years, 11.7% of those aged 75 to 84 years, and 19.8% of people aged 85 year or older. Women are affected slightly more than men are, and this excess in prevalence is mainly due to a higher risk of cortical cataracts.7,10,11 Mitchell et al10 also found that the rates of cortical cataracts were higher in women than men in each age group and the age-adjusted prevalence of advanced cortical cataract was significantly higher in women compared with men—relative prevalence 1.21 [95% confidence interval (CI) 1.08 to 1.36]. In the Beaver Dam Eye Study, Klein et al11 found that women had more cortical opacities than men (p <.002). Dielemans et al6 reported that age-specific prevalence figures of POAG in the Netherlands increased from 0.2% (95% CI: 0.16, 0.24) in the age group of 55 to 59 years to 3.3% (95% CI: 2.57,4.04) in the age group of 85 to 89 years. Men had a more than three times higher risk of having primary open-angle glaucoma than women (odds ratio, 3.6). Tuck and Crick,12 studying the age distribution of POAG in England, found that the prevalence for age 40 to 89 years was 1.2%, rising from 0.2% for those in their 40s to 4.3% for those in their 80s. Using data from the NHANES, Hiller et al13 found that cortical and nuclear cataracts were more commonly associated with blacks than whites (relative risk of cortical cataracts 3.5 and of nuclear cataracts 1.8 for blacks versus whites). Blacks have a prevalence of POAG three or four times higher than that of whites.14,15 There is probably a wide variation of geographic distribution of age-related cataract. In Punjab, India, the prevalence of senile cataract was found to be 15.3% among 1,269 persons aged 30 years and older with a prevalence of 1% for ages 30 to 49 and 67% for ages 70 and older.16 In the Tibet Eye Study (2,665 participants) the prevalence of senile cataract among persons aged 20 to 32 years was 0.2% and among persons aged 40 or more was 11.8%. The authors attributed these findings to the high altitude (4,000 meters) because this prevalence was 60% higher than the prevalence of a similar, previously conducted study in Shunyi County, China, with an altitude of only 50 meters.17 However, Brilliant et al18 also found that cataract prevalence was negatively correlated with altitude in 873 residents of Nepal, reporting a 2.7 times lower prevalence at sites over 1,000 meters than at sites of 185 meters or less (r = -.0533, p <.0001). Klein et al19 found that less education was significantly associated with nuclear and cortical cataract, whereas lower income was significantly associated with cortical and posterior subcapsular cataract (p <.05). Hiller et al13 found in the NHANES study that less education was associated only with cortical cataract [realtive risk (RR) = 1.8 for less than 9 years of schooling vs. college], whereas posterior subcapsular cataracts were associated with diabetes (RR = 6.6 for diabetes present vs. diabetes absent) and high systolic blood pressure (RR = 2.2 for 160 mm Hg vs. 120 mm Hg). Positive correlation between cataract prevalence and sunlight (p <.0001) was observed by Brilliant et al.18 Taylor et al20 examined 838 fishermen at Chesapeake Bay and found that high cumulative levels of ultraviolet B (UVB) exposure significantly increased the risk of cortical cataract (regression coefficient, 0.70; p = .04) and that fishermen with cortical lens opacities had a 21% higher average annual exposure to UVB (t-test, 2.23, p = .03). In a series of 351 cataract patients operated in Oulu, Finland, Lumme and Laatikainen21 found that 30% of them lived alone at home, 62% lived with some other person, and 8% were in institutions. Another study has found that anterior subcapsular cataract was significantly (p = .001) more prevalent (26%) in participants with schizophrenia than controls (0.2%). 22 Evaluation of 4,926 participants in the Beaver Dam Eye Study revealed a relationship between cigarette smoking and lens opacities.23 Specifically, it was found that the frequency of nuclear sclerosis increased with cigarette smoking in both sexes. For men the odds ratio (OR) was 1.09 (CI = 1.05,1.14) and for women, the OR was 1.09 (CI = 1.04,1.16). It was also found that the frequencies of posterior subcapsular cataract (PSC) also increased in both sexes with smoking. The OR was 1.06 (CI = 0.98,1.14) for women and 1.05 (CI = 1.00,1.11) for men. Recently there have been suggestions that good nutrition with antioxidant supplements may have protective association against cataract. Jacques et al24 investigated the antioxidant status of 112 individuals aged 40 to 70 years, and found that subjects with high levels of at least two of the three vitamins (vitamin E, vitamin C, and carotenoids), are at reduced risk of cataract (OR, 0.2). Similar findings of dietary intake of riboflavin, vitamins C and E, and carotene as well as intake of niacin, thiamin, and iron support a protective effect against cortical, nuclear, and mixed cataract (OR 0.40, 0.48, 0.56, respectively).25 Drug intake may also play a role in cataract formation. The association of steroid intake with the PSC is well established. In the Lens Opacities Case-Control Study of 1,380 participants, it was found that oral steroid therapy increased the risk of PSC (OR, 5.83).25 In the Blue Mountains Eye Study26 the hypothesis that aspirin protects against cataract formation was not supported because aspirin users for more than 10 years had higher prevalence of PSC than did 40 nonusers (p = .02). In the same study, antihypertensive medications, cholesterol-lowering drugs, and allopurinol were not associated with any type of cataract, whereas the use of antimalarial drug meracrine was associated with PSC (OR, 3.56; 95% CI = 1.56, 8.13) and the use of phenothiazines with nuclear cataract (OR, 2.18; CI = 1.01,4.74). In a recent study, McCarty et al22 found that the distribution of the age-related cataract was similar across all users of psychotropic medications (diazepams, butyrophenols, tricyclic antidepressants, and monoamine oxidase inhibitors), with the exception of users of phenothiazines in whom cortical cataract was statistically lower (p = .047). Cataract is a major health problem; it is the leading cause of blindness worldwide.27 It is estimated that more than 1 million cataract surgeries are performed annually in the United States.28 Steinberg et al29 analyzed a 5% sample of Medicare beneficiaries who underwent extracapsular cataract extraction (ECCE) between 1982 to 1987. The authors modified the costs by using the 1991 charges allowed by Medicare. It was found that the median charge allowed by Medicare for an uncomplicated routine cataract surgery was approximately $2,500 and that Medicare spent $3.4 billion on cataract-related surgery. In addition, Medicare also spent more than $39 million for preoperative evaluation of nonophthalmologic tests such as cardiac angiograms, and more than $18 million for perioperative medical services. Kobelt et al30 estimated the direct cost of glaucoma management in a study dealing with 200 glaucoma patients in Germany. They found that during the 2 years of follow-up, 54% of patients had their therapy changed at least once. Mean total charge and cost per patient were 815 and 1,274 deutsche marks, respectively. Mean intraocular pressure (IOP) at baseline was 31.2 mm Hg and after 2 years 18.8 mm Hg. IOP at baseline was positively correlated with costs (p <.01), whereas IOP reduction after treatment initiation was negatively correlated with costs (p <.01). The authors concluded that because frequent treatment change was associated with higher costs, new treatments that control the IOP effectively over time may reduce the cost of patient management. There are quite a few options by which the problem can be solved. These options are based on general principles, surgical experience, and individualization of each case. Cataract and glaucoma are, in the majority of cases, diseases of aging. And as population life span increases, the frequency of both conditions in the same age group may increase as well. Also, the chronic use of glaucoma medications that cause miosis, apart from other side effects, may have a catarac-togenic effect. Cataract formation is associated with the use of both directly acting miotics (pilocarpine) and indirectly acting anticholinesterase drugs (phospholine iodide).31 Therefore, glaucoma and cataract not only commonly coexist, but one can influence the management of the other. On the other hand, the evolution of both cataract and glaucoma surgery of the past 5 to 10 years has been enormous. Modern cataract surgery is now characterized by the reduced incision size of phacoemulsification, the use of foldable intraocular lenses (IOLs),32 and improved techniques of management of the miotic pupil.33 Concerning glaucoma surgery, refinement of trabeculectomy by microsurgery, the possibility of less invasion of the conjunctiva, and the adjunctive use of antimetabolites,34 releasable sutures,35 and laser suture lysis36 have all improved the risk/benefit ratio for the glaucoma and cataract patient. Therefore, ophthalmologists must be prepared to simultaneously manage cataract and glaucoma, taking advantage of all the latest advances for effectively solving this situation. To evaluate a cataract, pupillary dilation is necessary. One can then identify the types of cataracts (nuclear, cortical, subcapsular), the integrity of the zonules, the existence of pseudoexfoliation or posterior synechiae, the degree of pupillary dilation, and the health of macular area. In a case of axial (nuclear) cataract and miosis (either from miotics or from age), pupil dilation may improve a patient’s visual acuity to such a degree that a filtering operation may be sufficient. This approach may work better because the patient, after a successful filtering procedure, might be taken off miotics and not subjected to further miosis. In the case of a low-density cortical cataract, a patient may have 20/40 vision and yet experience severe disability and glare in driving under bright sunlight or facing oncoming vehicle headlights. In the case of a posterior subcapsular cataract, one needs to be extra vigilant because vigorous scraping or vacuuming of the calcified opacity may lead to rupture of the posterior capsule. Zonules become fragile with advanced aging and in the presence of pseudoexfoliation. It is important to identify zonular integrity preoperatively so that an appropriate surgical technique may be planned. The existence of pseudoexfoliation predisposes to inadequate pupillary dilation, fragile zonules, increased postoperative inflammation, and increased risk of capsular tear during anterior capsulotomy.37,38 Posterior synechiae prevent complete dilation and their lysis may cause postoperative inflammation as well. Finally, an inadequate pupillary dilation may require additional surgical manipulations for adequate visualization (see below, How Is the Miotic Pupil Managed?). Examination of the macular area is important to determine whether the decrease in visual acuity is due to lens opacification or retinal disease. The macular function can be determined either by laser interferometer or by the potential acuity meter (PAM). Laser interferometry measures potential visual acuity by using either red helium-neon laser light or simple white light and checks a field size of 1.5 to 8 degrees. PAM projects a Snellen chart through a 0.1-mm diameter aperture and checks a field of vision of 6 degrees.39 The PAM can be used reliably in cases where visual acuity is better than 20/60 and there is mild to moderate glaucomatous damage, whereas it is unreliable if visual acuity is worse than 20/60 and the damage is severe.40 The prediction of visual outcome is better if PAM can be used in combination with automated perimetry,41 which estimates not only foveal area (as PAM does) but perifoveal thresholds as well. Both laser interferometry and PAM perform poorly in mature and hypermature cataracts because the patient may not perceive the test objects. The factors to consider for cataract evaluation in patients are outlined in Table 20–1. Among the important factors for the evaluation of glaucoma are the type of glaucoma, the degree of glaucomatous damage, its progression or stability, the quality of control of IOP, and the number as well as tolerance of antiglaucoma medications. It is important to identify the type of glaucoma as POAG or secondary glaucoma. The latter category may present unique challenges, such as inadequate pupillary dilation and zonule fragility in pseudoexfoliation glaucoma, lens intumescence, and dislocation in traumatic glaucoma, and intraocular inflammation in uveitic glaucomas. There are also some types of glaucoma that might be associated with cataracts, namely pseudoexfoliative glaucoma,42–44 Fuchs’ heterochromic cyclitis,45 and uveitic glaucoma. Hiller et al,42 in a population-based survey with an age-adjusted analysis, found positive but no statistically significant association between pseudoexfoliation and senile lens changes (the odds ratios were greater than 1.0, but did not achieve statistical significance). However, Roth and Epstein43 found that 40% of the patients with unilateral exfoliation had cataracts in that eye, as compared to 5% in the other eye. Lumme and Laatikainen44 found a 31% prevalence rate of exfoliation syndrome in 351 patients undergoing cataract surgery by ECCE. Patients with exfoliation syndrome also experienced a fourfold occurrence of vitreous loss during surgery. Cataract surgery in patients with chronic uveitis is a major surgical challenge. The level of inflammation of the eye has to be estimated preoperatively because postoperatively there may be a greater tendency for increased inflammation, fibrin, and synechiae formation, which may lead to an occluded pupil. Also, cystoid macular edema presents a major obstacle to visual rehabilitation after cataract surgery in patients with uveitis, and if a lens implant is to be considered, it must be placed in the capsular bag.46 The pertinent factors for glaucoma evaluation are outlined in Table 20–2.
Management of Cataract and Glaucoma
Definition
What Variables Need to be Considered in Management of Cataract and Glaucoma?
Epidemiology and Importance
Has There Been an Increase or Decrease of Cataract and Glaucoma Over the Years?
What Are the Demographic Characteristics of Patients with Cataract and Glaucoma?
Are There Any Social and Economic Factors Associated with Cataracts and Glaucoma?
Are There Any Personal Habits That Predispose Patients to Cataract and Glaucoma?
What Is the Magnitude of the Economic Cost of Cataract and Glaucoma?
What Is the Importance of the Management of Cataract and Glaucoma?
Diagnosis and Differential Diagnosis
What Factors Need to be Evaluated in a Patient Suffering from Cataract and Glaucoma?
Type of cataract |
Integrity of zonules |
Presence of pseudoexfoliation |
Existence of posterior synechiae |
Degree of pupillary dilation |
Potential visual acuity |
Health of macular area |
There are difficulties in evaluating the severity of glaucomatous optic nerve damage based on fundus examination or by visual fields in patients with lens opacities. Any opacity of the ocular media can cause localized defects or generalized depression of sensitivity.47 As the lens becomes denser, less light reaches the retina, and therefore, preexisting field defects may appear denser and larger. Although there are programs that compensate for this influence by subtracting the generalized depression to expose localized defects, if any, still the evaluation is not completely precise.48 When evaluating visual field defects, attention must be paid to the density of the lens, the visual acuity, and the comparison with previous visual fields. Although the Glaucoma Laser Trial49 has used its own strict criteria, in general, few (two to three) localized defects at the Bjerrum area and/or mild generalized reduction of sensitivity might be considered minimal optic nerve damage. More and denser localized defects might imply moderate damage. Finally, dense paracentral scotomas or those close to fixation are considered severe damage. A miotic pupil can also cause a significant decrease of sensitivity and constriction of the visual field, and it is desirable for the pupils to be at least 2.5 mm before testing.50
When visual fields are confusing, the severity of glaucomatous optic nerve damage may be based on the evaluation of the optic nerve head. Important parameters include cup-to-disc ratio, neuroretinal rim pallor, optic disc blood vessels, and evidence of peripapillary atrophy. Although these are arbitrary categories, damage is minimal if the stereoscopic view of the cup-to-disc ratio is less than or equal to 0.6, moderate if the ratio is between 0.7 and 0.8, and severe if it is equal to or more than 0.9. Also, the presence of an acquired pit of the optic nerve51 or a disc hemorrhage is a finding of rather severe optic nerve damage and sometimes an indication of progress of the disease.52 Criteria to evaluate the degree of optic nerve damage in a glaucomatous patient with cataract are listed in Table 20–3.
Type of glaucoma |
Degree of optic nerve damage |
Control of intraocular pressure (IOP) |
Progression of disease process |
Number and tolerance of antiglaucoma agents |
Compliance by the patient |
Minimal optic nerve damage
|
Moderate optic nerve damage
|
Severe optic nerve damage
|
*Note: Optic disc hemorrhage at any stage of optic nerve damage indicates progression of glaucoma. |
What Are the Major Concerns About Cataract Surgery on Glaucomatous versus Nonglaucomatous Eyes?
The chronic use of pilocarpine and other parasympathomimetic drugs causes a miotic pupil mostly resistant to dilation. Inadequate pupillary dilation makes phacoemulsification dangerous because of poor red reflex and uncontrolled capsulorhexis. There is a high incidence of posterior capsule rupture.38 Indeed, in a patient with a small pupil, the edge of the continuous curvilinear capsulorhexis can be lost under the pupillary margin and a tear of radial fashion can reach the lens equator and sometimes can even extend to the posterior capsule.
Also, the chronic use of miotic agents causes a breakdown of the blood–aqueous barrier, resulting in excessive postoperative inflammation.53 Chen et al53 compared 20 eyes in which pilocarpine was not administered prior to performing trabeculectomy combined with ECCE and posterior chamber (PC) IOL implantation, with 40 eyes in which pilocarpine was administered prior to undertaking the same procedures. The authors found that the incidence of complications such as pigment deposits, posterior synechiae, IOL displacement, and capture by the iris was significantly higher in the pilocarpine group (p <.05).
Finally, the most important immediate concern is that IOP might rise acutely, usually 3 to 24 hours after cataract extraction. This pressure spike can occur not only after ECCE but also following a phacoemulsification.54–57 Ruiz et al54 found an average increase in IOP of 12.9 ± 2.7 mm Hg 24 hours after ECCE in normal eyes, with 55% of eyes exceeding 25 mm Hg. Gross et al56 reported an IOP equal to or greater than 30 mm Hg in 43% of normal eyes following ECCE and in 27% following phacoemulsification, 2 to 3 hours postoperatively. McGuigan et al55 reported that four (10%) of 40 normal eyes experienced an increase of 7 mm Hg or more in IOP 24 hours following ECCE. Kooner et al58 reported that 29% of patients had an IOP greater than 23 mm Hg at 24 hours postoperatively. Hopkins et al57 reported 52.2% of normal eyes having IOP greater than 20 mm Hg and 22.7% showed IOP greater than 30 mm Hg 4 hours after phacoemulsification.
Such an increase can occur more frequently and to higher levels in glaucomatous eyes.55,59 McGuigan et al55 found an IOP elevation of 7 mm Hg or more in 23 (62%) of 37 glaucomatous eyes 24 hours following ECCE. Krupin et al59 reported that 69% of preoperatively medically controlled glaucomatous eyes that underwent ECCE with PC-IOL alone experienced an increase in IOP of 10 mm Hg or more (range 28–60 mm Hg); 77% of these patients had an IOP greater than 25 mm Hg. Also, Vu and Shields60 reported IOPs greater than 21 mm Hg 24 hours after cataract surgery in 52% of eyes with glaucoma.
This ocular hypertension may be related to trabecular collapse, retained cortical material, pigment release, inflammation, or the use of viscoelastic substances,61 although it may occur even when this material is adequately removed at the end of surgery.62 In patients undergoing ECCE, Naeser et al61 found IOP higher than 26 mm Hg in 43% of normal eyes when using sodium hyaluronate 1% and in only 19% of eyes when balanced salt solution or air was used (p <.05). Berson et al62 found a 65% decrease in outflow facility after instillation of sodium hyaluronate into the anterior chambers of enucleated human eyes. This decrease was sustained even after vigorous irrigation of the anterior chamber was performed either immediately or 3 hours later.
The pressure spike can occur not only after ECCE with manual nucleus expression but also following phacoemulsification.56,57 Hopkins et al57 reported 52.2% of normal eyes having IOP greater than 20 mm Hg and 22.7% with IOP greater than 30 mm Hg 4 hours after phacoemulsification.
Healthy optic nerves may tolerate these transient IOP elevations, but in the presence of glaucomatous damage there may be a permanent worsening of damage.63 Savage et al63 reported that 9.7% of glaucomatous eyes had deterioration of visual fields after ECCE and PC-IOL implantation.
Treatment and Management
How Is Coexisting Cataract and Glaucoma Managed?
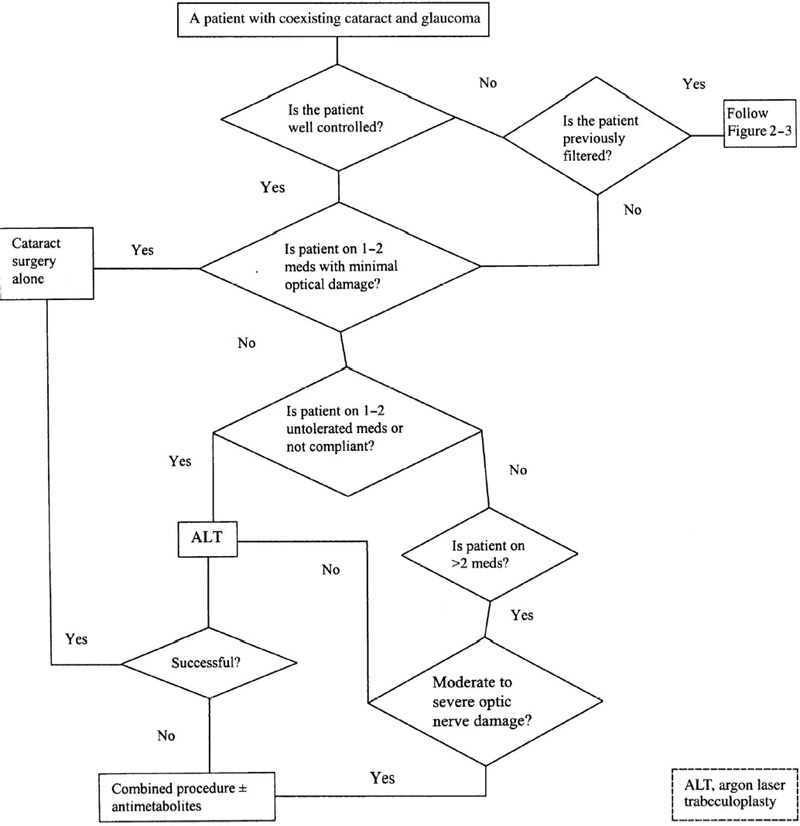
There are three basic surgical alternatives: (1) cataract surgery alone, (2) combined cataract and glaucoma surgery, and (3) glaucoma surgery alone and cataract surgery later (Fig. 20–1).
There is a long-standing debate on the choice of appropriate surgical approaches in these patients. The final decision may be based on some established general rules, the surgeon’s experience, and the complexity of the case itself.
There are three major groups in which the above surgical management alternatives may be applied: (1) medically well-controlled glaucomas, (2) uncontrolled glaucomas, and (3) postfiltering cases.
How Is Medically Well-Controlled Glaucoma Managed with or without Argon Laser Trabeculoplasty (ALT)?
This group includes patients who have one common denominator (well-controlled glaucoma) but differ in the magnitude of glaucomatous damage, the type of glaucoma, and the number of medications required. Specifically, this group can be divided in the following subgroups: (1) well-controlled glaucoma with one or two well-tolerated medications (with or without ALT) and minimal optic nerve damage; (2) well-controlled glaucoma with one or two untolerated medications with minimal optic nerve damage; and (3) well-controlled glaucoma with more than two well-tolerated medications with moderate to severe optic nerve damage.
Figure 20–1. Management of the patient with coexisting cataract and glaucoma.
How Is Well-Controlled Glaucoma Managed If One or Two Well-Tolerated Medications Are Used (with or without ALT) and There Is Minimal Optic Nerve Damage?
The simplest and safest approach to these patients is to perform cataract surgery alone. This decision is based on the fact that a minimally damaged optic nerve is resistant to the possible postoperative IOP rise.64 If the glaucoma of these patients is controlled with one or two medications without ALT, then this procedure may be considered preoperatively, especially if a miotic is being used. ALT may help the surgeon in withdrawing the miotic and prevent miotic-induced intraoperative and postoperative complications.
IOP reduction achieved by ALT can be maintained after cataract surgery.65 Brown et al65 performed ALT in 25 eyes with a mean prelaser IOP of 23 mm Hg and achieved a mean postlaser IOP of 15.8 mm Hg. After approximately 10 to 11 weeks, all eyes had extracapsular cataract extraction. The mean IOP after an average follow-up of 16 months was 15.1 mm Hg. It is better to perform ALT at least 1 month before the cataract surgery. Four studies have reported an increased rate of encapsulated blebs in eyes with previous ALT,66–69 although the rate was statistically significant in only two.
ECCE with PC-IOL implantation may sometimes cause a long-term decrease of IOP.55,70 Steuhl et al70 attribute this pressure drop to the deepening of the anterior chamber angle after ECCE and PC-IOL implantation. The mean preoperative chamber-angle width in 50 eyes was 28.0 ± 5.6 degrees, whereas the mean postoperative value was 37.4 ± 2.4 degrees, yielding a mean postoperative deepening of the chamber angle of 9.3 ± 4.5 degrees. The chamber-angle quotient was 1.38 ± 0.27.
This IOP reduction may be associated with phacoemulsification as well.71,72 Kim et al71 reported 31 medically controlled glaucoma patients who underwent phacoemulsification and PC-IOL implantation with a mean follow-up of 16.4 months. The mean IOP dropped from 18.1 ± 3.1 mm Hg preoperatively to 15.2 ± 2.9 mm Hg postoperatively, and the mean number of antiglaucoma medications dropped from 1.7 preoperatively to 0.7 postoperatively. Similarly, Storr-Paulsen et al72 reported mean preoperative IOP of 23 mm Hg (range 21–30) and mean postoperative IOP of 16.5 (range 12–18) 12 months after phacoemulsification in medically uncontrolled glaucomatous eyes. This decrease was statistically significant (p = .005). The number of medications was decreased from a mean of 2 (range 1–3) preoperatively to 1 (range 0–4) postoperatively, though this decrease was not statistically significant. Small-incision cataract surgery by phacoemulsification also has the added advantage that a filtering procedure may be done at a later date in undisturbed conjunctiva.
How Is Well-Controlled Glaucoma Managed If One or Two Untolerated Medications Are Used with Minimal Optic Nerve Damage?
In this subgroup, although glaucoma may be well-controlled, patients either cannot tolerate the medication or cannot follow the administration schedule (noncompliance). A good option for the management of this situation is to perform an ALT first, to eliminate the need for medications. Later, one may proceed with cataract surgery alone. In case of ALT failure, the surgeon may consider a combined procedure.
Combined cataract extraction and filtration surgery is an effective procedure for patients with visually significant cataract and glaucoma. Small-incision phacoemulsification is preferred over a large-incision ECCE. There are several advantages of a combined procedure. A combined procedure decreases the magnitude of the early postoperative IOP spike, decreases the number of glaucoma medications, avoids the inconvenience and the cost of a second operation, and provides a rapid visual rehabilitation. Table 20–4 lists the advantages of combined cataract and glaucoma surgery. For more details of combined procedure, see below (How Is Uncontrolled Glaucoma and Cataract Managed?).
How Is Well-Controlled Glaucoma Managed If More Than Two Well-Tolerated Medications Are Used or If There Is Moderate to Severe Optic Nerve Damage?
An optic nerve with this degree of damage might not be able to tolerate postoperative pressure elevations. Elevated IOP may compromise optic nerve head blood flow and result in further permanent and irreversible damage.59,64 For this subgroup of patients there are several rational alternatives. The surgeon might take advantage of the necessity of cataract surgery and perform a filtering procedure at the same time. This may eliminate or decrease the necessity for antiglaucoma medications, which, although well tolerated, alter the patient’s quality of life. In these patients, filtering surgery alone might not be recommended otherwise. However, if the patient has well-controlled glaucoma with good compliance, good tolerance to medical treatment, and minimal optic nerve damage, an equally correct alternative is to perform either cataract surgery alone or an ALT followed by cataract surgery. Those patients with borderline IOP control may also be candidates for combined surgery so as to avoid postoperative spikes.
Whenever in doubt about performing a cataract surgery alone or a combined procedure, the patient’s age plays an important role in the final decision. Generally, cataract surgery alone is more appropriate for older patients, whereas combined surgery is better suited for younger ones. Phacoemulsification is preferable, leaving conjunctiva intact for a future filter, if necessary. Optic discs are at greater risk for further damage if the exposure to elevated IOP is of longer duration.
How Is Uncontrolled Glaucoma and Cataract Managed?
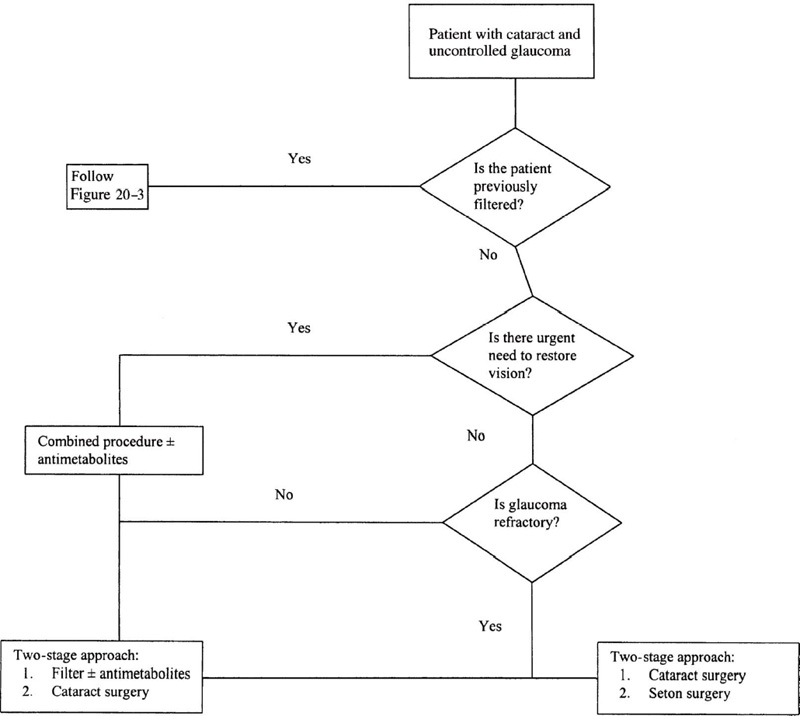
In cases of poorly controlled glaucoma and cataract, the goals are the visual rehabilitation of the patient, the avoidance of immediate postoperative IOP rise, and long-term IOP control. This can be achieved theoretically by a combined procedure (see Fig. 20–2).
Until the beginning of the 1990s, ophthalmologists performed a combined procedure by doing an ECCE with PC-IOL implantation and a trabeculectomy.
Single procedure |
Low incidence of early postoperative IOP spikes |
Reduced number of antiglaucoma drugs postoperation |
Rapid restoration of vision |
Less cost |
Figure 20–2. Management of patient with cataract and uncontrolled glaucoma.
This combination does not completely eliminate transient increases of IOP, but reduces the frequency and magnitude of this complication. Krupin et al59 reported an IOP rise of 10 mm Hg or more in 14% of patients and an IOP over 25 mm Hg in 21% on postoperative day 1, following incision ECCE and trabeculectomy. This pressure rise can be related to obstruction of the filtering site by a blood clot, iris, fibrous material, or viscoelastic agent.73
Combined surgery also has many complications. Simmons et al74 reported 27 (36%) of 75 eyes with IOP greater than 30 mmHg and 30 (40%) having a pressure of 7 mm Hg or more above their preoperative level during the first 6 months after large-incision ECCE with IOL implantation combined with trabeculectomy. They also reported detectable filtering blebs in 41% of patients at 2 months and in only 12% at 12 months. Also, hyphema was present in 45% of the cases in the early postoperative period.
Because of the increased rate of complications following a combined ECCE with nuclear expression and filtering procedure, surgeons saved this operation for cases where the glaucoma was poorly controlled. Nowadays, small-incision cataract surgery by phacoemulsification and foldable IOL has replaced the ECCE. Also, adjunct antimetabolites have an increased success rate and increased safety of combined procedures.75,76
Small-incision surgery has the advantages of both reduced conjunctival dissection and decreased postoperative inflammation. Therefore, the excessive wound healing and the risk for subsequent bleb failure in combined procedures are reduced.77,78 The complications of such a modern combined procedure are less and the indications have changed.77–81 Wishart and Austin77 compared combined cataract extraction using the extracapsular technique with phacoemulsification, and found that the latter procedure resulted in earlier visual rehabilitation, improved long-term IOP control, and less postoperative astigmatism, as well as less hyphema, fibrous iritis, choroidal detachment, and hypotony. A postoperative pressure rise occurred in 32% of the ECCE-trabeculectomy group and in 23.5% of the phacoemulsification-trabeculectomy group. Shingleton et al78 reported results from 35 eyes that underwent ECCE, PC-IOL, and trabeculectomy, and 37 eyes that underwent phacoemulsification, PC-IOL, and trabeculectomy. The follow-up was 16 months and the average IOP reduction of the phacoemulsification group was significantly lower (5.0 ± 4.3 mm Hg) than the average IOP reduction of ECCE group (2.9 ± 4.1 mm Hg) (p < .03). The authors did not find significant differences between the groups in postoperative visual acuity and reduction of antiglaucoma drugs.
Wedrich et al81 compared the efficacy and complication rate between an ECCE-trabeculectomy (ECCE-trab) group and a phacoemulsification-trabeculectomy (Phaco-trab) group. In the latter, the final mean IOP (14.2 ± 3.0 mm Hg vs. 15.5 ± 2.7 mm Hg) was statistically lower (p = .02). Also, in the phaco-trab group, there was a higher percent of patients without medications (82% vs. 65%, p = .07), a lower early postoperative IOP rise greater than 25 mm Hg (2% vs. 18%, p = .009), a lower filtering bleb scarring (8% vs. 63%, p <.0001), and lower total number of complications (63% vs. 87%, p = .006).
Although there is better protection from the early IOP increase, some patients still show IOP spikes after small-incision surgery and trabeculectomy.57,77,81,82 Hopkins et al57 reported 13.9% of patients with an IOP between 20 and 30 mm Hg and 5.5% with IOP more than 30 mm Hg, 4 hours after phacoemulsification combined with trabeculectomy, and 20.5% with an IOP between 20 and 30 mm Hg and 4.6% with IOP more than 30 mm Hg on postoperative day 1. These eyes required digital massage alone to lower the pressure without medical therapy.
Similarly, Lyle and Jin82 found IOP greater than 30 mm Hg in 9.6% of patients having 3-mm incisions and in 6.3% of patients with 6-mm incisions on postoperative day 1 following combined small-incision surgery. The authors do not give any explanation for the percentage disparity of results.
There has been concern about the long-term efficacy of combined procedures. However, as the procedures have evolved with the use of small incisions, long-term success in controlling IOP is improving.72,83–87 Anders et al83 compared the results of a no-stitch scleral tunnel phacoemulsification with standard no-stitch phacoemulsification. They found that 1 year after surgery, the combined procedure group had a decrease of IOP of 7.6 ± 5.5 mm Hg, whereas the standard phacoemulsification group had a decrease of 3.7 ± 4.2 mm Hg. The difference was statistically significant (p <.001). Dittmer and Quentin86 reported a significant decrease in IOP from 21.8 to 14.8 mm Hg following combined phaco-trab with silicone PC-IOL 21.6 weeks postoperatively (p <.001). Mamalis et al87 performed phacoemulsification with PC-IOL and trabeculectomy in 212 eyes, with a follow-up of 26 months. They reported a decrease of IOP from 23.1 mm Hg preoperatively to 15.9 mm Hg postoperatively and of glaucoma medications from 1.85 preoperatively to 0.41 postoperatively. Only 10% had a postoperative IOP greater than 21 mm Hg.
Results of combined phacoemulsification and trabeculectomy with PC-IOL are even better with the use of adjunctive mitomycin C or 5-fluorouracil (5-FU) in selective cases.75,88 (See below, What Is the Influence of Antimetabolites in a Combined Procedure?)
Another alternative management for uncontrolled glaucoma and cataract is the two-stage approach—filter first and cataract surgery at a later date. Before the evolution of the present combined surgery, the two-stage approach was the procedure of choice in uncontrolled glaucomas, with severely damaged optic nerves, and in cases where there was an immediate threat to vision. Naveh et al89 reported 40 patients who underwent combined surgery and 38 patients who underwent trabeculectomy alone and followed them for 18 months postoperatively. Pressure levels were significantly lower in the trabeculectomy group (12.8 ± 4.2 mm Hg) than in the combined group (16.5 ± 5.6 mm Hg). However, the technique used was the large-incision ECCE.
Although the evolution of combined surgery with phacoemulsification and the adjunctive use of antimetabolites continues, the success rate is still far lower than trabeculectomy alone.90 Park et al90 found a mean IOP reduction of 6.8 ± 5.5 mm Hg in a group of clear-cornea phacoemulsification combined with separate trabeculectomy plus 5-FU, and 10.3 ± 7.6 mm Hg in a group of trabeculectomy alone plus 5-FU. Therefore, trabeculectomy alone is probably still the procedure of choice when there is glaucoma with an immediate threat of vision loss or an inflammatory glaucoma such as Fuchs’ heterochromic cyclitis. This approach, however, delays visual rehabilitation for the patient, and both bleb survival and IOP control may be compromised by the subsequent cataract surgery.91 Cataract surgery should be delayed at least 3 months and ideally for 6 months after a filtering procedure.
What Is the Influence of Antimetabolites in a Combined Procedure?
Antimetabolites may improve the success rate of filtering surgery in glaucoma patients with a poor prognosis.92,93 However, their efficacy in combined procedures is still controversial.94,95 Shin et al94 found a mean IOP of 14.6 ± 4.3 mm Hg in patients with phacoemulsification–PC-IOL–trabeculectomy and mean IOP of 14.7 ± 4.3 mm Hg (p = .94) in patients with adjunctive mitomycin C at the last follow-up visit (mean follow-up time 21.0 ± 7.7 months). O’Grady et al95 reported no effect of 5-FU and found mean IOP 15.0 ± 5.0 mm Hg in patients with phacoemulsification–PC-IOL–trabeculectomy and 15.4 ± 3.7 mm Hg in patients with adjunctive 5-FU at the last follow-up visit (p = .45).
On the other hand, Gandolfi and Vecchi75 treated one group of uncontrolled glaucoma patients with combined clear cornea phacoemulsification–PC-IOL and separate incision trabeculectomy with 5-FU, and another group without 5-FU as a control. The difference became significant 3 months after surgery and remained so thereafter. At 1 year postsurgery they found that 10 of 12 eyes of the 5-FU group had an IOP less than or equal to 15 mm Hg, whereas in the control group only one of 12 eyes had an IOP less than or equal to 15 mm Hg (p = .00064). The IOP range was 10 to 17 mm Hg in the 5-FU group and 14 to 22 mm Hg in the control group.
Derick et al88 reviewed 42 eyes that underwent phacoemulsification and trabeculectomy with mitomycin C and 42 eyes that had trabeculectomy alone with mitomycin C. At final follow-up at 21.8 ± 6.0 months, the IOP averaged 13.9 ± 5.1 mm Hg in the first group and 12.3 ± 4.7 mm Hg in the second. Shin et al76 found no statistically significant difference between two groups of nonselected patients with POAG who underwent primary trabeculectomy combined with phacoemulsification and posterior chamber IOL, with or without the adjunctive use of mitomycin C. However, they found that black race, diabetes mellitus, preoperative IOP greater or equal to 20 mm Hg, and more than one preoperative medication were all significant prognostic factors for filtration failure without mitomycin C. They concluded that the intraoperative use of mitomycin C should be selective, limited to patients with one or more of these factors.
Shin et al96 also reported for the first time that the intraoperative use of 0.5 mg/mL mitomycin C for 3 minutes had an inhibiting effect on posterior capsule opacification after combined surgery.
Although the results with antimetabolites in combined procedures are encouraging, further long-term prospective studies are necessary. In the meantime, adjunctive therapy preferably with mitomycin C seems to be helpful in combined procedures for selective patients with uncontrolled or advanced glaucoma. However, attention should be given to the potential side effects of these agents. For more details of antimetabolites see Chapter 19.
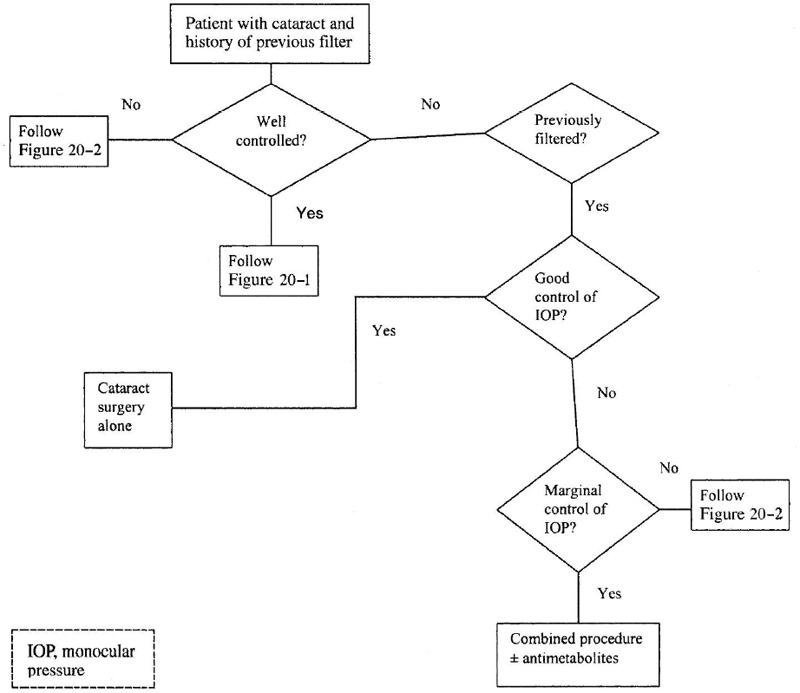
How Is a Cataract Managed Following Filtering Surgery?
The management of a patient with a cataract following filtering surgery depends on the condition of the filter itself. If a patient has a well-functioning filtration procedure and is on no antiglaucoma medications, then the indicated approach is cataract surgery alone (Fig. 20–3).
It is important, if the surgeon’s experience allows it, that a phacoemulsification be done. Because postoperative inflammation with this procedure is less, the possibilities for bleb survival are more. Also, small-incision surgery has the advantage of leaving enough space for future filtration if the existing one stops functioning. It is conceivable that clear cornea phacoemulsification is superior, because it leaves even more conjunctiva intact. If phacoemulsification cannot be done, then the approach will be a large-incision ECCE, either limbal (temporal or inferior) or clear corneal with a possibility of large amount of induced astigmatism.
Figure 20–3. Management of the patient with cataract and glaucoma and previous filtering surgery.
Burratto and Ferrari97 reported 104 eyes with filtering blebs that underwent ECCE and PC-IOL implantation, with good functional results and stable IOP after a follow-up of 8 months. In 33 eyes (32%) they performed ECCE inferiorly and the remaining 71 (68%) eyes underwent phacoemulsification with limbal incision temporally. However, the authors do not mention postoperative astigmatism.
In cases where the filter has completely failed, the postoperative IOP rise may be dangerously high, so a combined procedure is indicated. If the patient has a marginally functioning bleb requiring glaucoma medical therapy, there is still need for prophylaxis against the pressure spike in the immediate postoperative period. On the other hand, cataract surgery of any kind may influence the long-term function of a previous bleb.98 Possible causes are the postoperative inflammation and the breakdown of the blood–aqueous barrier. In these cases cataract surgery alone will probably cause a complete failure of the marginally functioning bleb.
Shin et al99 investigated whether previously failed glaucoma filtration surgery is a risk factor for failure of subsequent trabeculectomy combined with cataract surgery. They also compared the role of adjunctive mitomycin C in repeat trabeculectomy combined with phacoemulsification and a PC-IOL. They found that without mitomycin C, success was significantly less in repeated trabeculectomy combined with phacoemulsification than in a primary trabeculectomy combined with phacoemulsification (p = .003). However, by use of mitomycin C intraoperatively, the success rate increased significantly (p = .02). The decreased success rate in subsequent trabeculectomy is attributed, according to them and other investigators,100,101 to the possible change in the composition of the aqueous humor after an intraocular surgery, to breakdown of the blood-aqueous barrier, and possibly to some other unknown reasons. Indeed, it has been shown that aqueous humor from a failed trabeculectomy had a greater chemoattractive activity for ocular fibroblasts than in control subjects.100 Also, ascorbic acid, which is cytotoxic to Tenon fibroblasts, was in lower concentration in the aqueous humor of eyes that underwent intra-ocular surgery.101
So in cases of a marginally functioning or nonfunctioning bleb, a combined cataract extraction preferably by phacoemulsification and probably with the adjunctive use of antimetabolites is indicated.
How Is Refractory Glaucoma and Cataract Managed?
When glaucoma becomes resistant to medical therapy and when filtration surgery, even with the adjunctive use of antimetabolites, fails to control IOP, then the alternatives are either cyclodestructive procedures or tube shunts. These eyes are usually associated with poor prognostic features such as uveitis, aphakia, pseudophakia, neovascularization of the angle, and young age. The cyclodestructive procedures, such as cyclocryotherapy or cyclophotocoagulation, have relatively high rates of phthisis and visual loss.102 Therefore, in an eye with refractory glaucoma and useful vision, their use is unpredictable and may be sight-threatening. On the other hand, tube shunts are useful alternatives. There is a better success rate and a lower complication rate, but these rates may vary depending on the type of the implant and the type of glaucoma.
Generally, success rates in tube shunts, with respect to control of IOP, range from 58% to 95%, with the lowest success rate in neovascular glaucoma.103–107 Melamed et al103 implanted Molteno implants in 41 eyes, and found IOP less than or equal to 18 mm Hg in 32 eyes (78%) after an average of 16 months. Major complications they reported were shallow anterior chamber and hypotony in six eyes (14.6%), vitreous hemorrhage and malignant glaucoma in two eyes (4.9%), and retinal detachment in one eye (2.4%). Fellenbaum et al104 reported that after implantation of a Krupin valve, IOP was less than 22 mm Hg in 66% 1 year postoperatively. The complications were fibrinous uveitis 24%, shallow or flat anterior chamber 20%, serous choroidal effusion and choroidal hemorrhage 16%, strabismus 12%, obstruction of the slit valve with fibrin 12%, and obstruction of the tube by fibrin or vitreous 8%. Siegner et al,105 using the Baerveldt implant, reported IOP less than 22 and more than 5 mm Hg in 60.3% 1 year postoperatively. The most common complications were shallow anterior chamber or hypotony 32%, choroidal effusion or hemorrhage 20.4%, corneal decompensation or edema 17.5%, hyphema 14.1%, and tube obstruction 12.6%. Huang et al,106 in a large series of 159 eyes following Ahmed glaucoma valve implantation, found at 1 year postsurgery IOP between 6 and 21 mm Hg in 87% of eyes and complications in 47%. The most common complications were the obstruction of the tube in 11% and hypotony in 8%. Also, 81% of the eyes were either aphakic or pseudophakic. Only one eye had combined cataract extraction with IOL and valve implantation.
These eyes have had a complicated course and in most cases they had previous cataract surgery. If refractory glaucoma coexists with cataract, it is reasonable to avoid a simultaneous seton insertion and a cataract extraction, avoiding any additional intraoperative or postoperative complications. But patients with extensive subconjunctival scarring may have no choice. A valved seton such as a Krupin or Ahmed is preferable to nonvalved implants. There is a greater need to avoid hypotony and thus prevent complications such as suprachoroidal effusion or suprachoroidal hemorrhage. The surgeon is advised to create an entry site for the seton before proceeding with cataract extraction. Pars plana insertion of the tube may be considered in patients who had prior vitrectomy or are aphakic or pseudophakic. In most cases, it is better to implant the tube shunt separately first, to relieve the optic nerve from the elevated IOP. Then, as soon as the eye is quiet, cataract surgery may follow, preferably by phacoemulsification. Cataract extraction usually does not alter the established function of the tube shunt. It is important to retain an intact posterior capsule or to have a posterior chamber IOL inserted, to avoid vitreous incarceration in the tube.108
Finally, in an eye with a cataract and repeatedly failed filters done without the use of antimetabolites, one may consider another filtering procedure with adjunctive use of antimetabolites. Inferior trabeculectomy is also an option, though the patient is at a greater risk for developing bleb infections. Depending on the condition of the patient, the surgeon may proceed to a combined procedure or a cataract surgery alone at a later date.
What Kind of Cataract Surgery Is Preferable for a Glaucoma Patient?
There is no doubt that phacoemulsification is the preferable procedure in most eyes suffering from glaucoma where cataract extraction alone or combined with a filtering procedure is indicated. This is because phacoemulsification provides three important advantages for the glaucomatous eye: smaller incision size, less manipulation of conjunctiva and surrounding tissues, and a reduced amount of postoperative inflammation.
Most glaucomatous eyes are difficult to manage intraoperatively. These patients tend to have hard nuclei, posterior synechiae, small and immobile pupils, and lower endothelial cell counts. Gagnon et al109 compared the corneal endothelial cell density in 102 patients with glaucoma with that of 52 patients without glaucoma. They found that corneal endothelial cell counts were significantly lower in patients with glaucoma than in controls and in patients receiving three to four glaucoma medications than those receiving one to two (p <.0001). It is our impression that in glaucoma patients with long-term use of antiglaucoma medications, a preoperative specular microscopy with endothelial cell count might be helpful and that the surgeon should be aware of possible corneal decompensation.
There is an increased prevalence of cataracts in eyes with pseudoexfoliation.42–44 Therefore, many patients suffering from pseudoexfoliation glaucoma may present with several characteristics of this disease, such as inadequate dilation before surgery, greater incidence of capsular rupture, fragile and weak zonules, probable phacodonesis, and shallow anterior chamber. Rupture of the posterior capsule, with subsequent vitreous loss and the possibility of inserting an anterior-chamber IOL, creates more problems in glaucomatous than in normal eyes. Kooner et al110 found an IOP rise of 8 mm Hg above baseline in 25.8% of eyes on the first postoperative day following anterior-chamber secondary implantation, but 3 years postoperatively medical treatment was required in only 11.3% of eyes. Therefore, although phacoemulsification is preferable, the surgeon has to be extremely skillful and experienced before attempting this procedure on a glaucoma patient. It might be much better to perform an ECCE if there is a greater chance of preserving an intact posterior capsule and inserting a PC-IOL in situ, rather than doing a complicated phacoemulsification with broken capsule, vitreous loss, vitreous in the anterior chamber, and a possibility of an anterior-chamber IOL. Almost all difficulties may be managed effectively by an experienced phaco surgeon. Poor dilation can be dealt with by following advanced small-pupil techniques, extremely hard nuclei can be dealt with by chopping techniques, and weak zonules can be dealt with by endocapsular rings. (For details of small pupil techniques, see below, How Is the Miotic Pupil Managed?) However, an experienced surgeon always assesses the risk/benefit ratio for each patient. That means that during the preoperative evaluation, he should formulate a plan that can be changed accordingly intra-operatively, adjusting to the needs of a particular patient.
If the surgeon decides to perform a combined phacoemulsification and trabeculectomy, this can be done with either a one-site or two-site approach. The one-site approach refers to the procedure in which the filter and the phaco are done through the same opening (usually at the superior corneoscleral limbus). On the other hand, the two-site operation is the one in which filter and phaco are performed at two different places. More surgeons who prefer the latter approach perform a clear cornea phaco temporally and a trabeculectomy superiorly.
Wyse et al111 used mitomycin C and compared the one-site and the two-site approaches and found that IOP reduction was not significantly different (p = .129). However, in a follow-up more than 3 months postoperatively, the percentage of eyes on glaucoma medication was significantly greater (p = .026) in the one-site group (55%) compared with the two-site group (15%), and the former group required significantly (p = .030) more glaucoma medications (0.8 ± 0.9) than did the latter group (0.2 ± 0.6). The possible explanation is that the two-site approach involves less manipulation of the conjunctiva and sclera in the trabeculectomy area. The surgeon is also able to manipulate each surgical site independent of the other in the postoperative period. On the other hand, digital message would be contraindicated in a two-site patient if the corneal wound were not sutured.
Another dilemma for the surgeon is whether the conjunctival flap should be limbal- or fornix-based in a combined procedure. There are advantages and disadvantages of the two approaches. A fornix-based conjunctival flap is easier to dissect and close, and has better exposure of the wound, and has less chances for buttonholing the conjunctiva, but there may be difficulty in locating the sources of bleeding, there is increased incidence of wound leakage, and the wound is near the trabeculectomy site. A limbal-based flap requires more time, but the wound is away from the trabeculectomy site, is more watertight, and thus is ideal for antimetabolite use. Simmons et al74 found no difference between limbal-based and fornix-based conjunctival flaps in combined trabeculectomy and ECCE, except a statistically significant difference in the frequency of postoperative hyphema (30% in fornix-based vs. 71% in limbal-based).
Murchison and Shields112 also found no differences in the two groups with respect to long-term pressure control, visual acuity, and complications. The only difference was the fact that IOP was greater than 30 mm Hg at postoperative days 1 and 2 in only one patient (4%) in the limbal-based group, compared to three patients (14%) in the fornix-based group. Stewart et al113 studied prospectively the results of limbal- versus fornix-based flaps in patients with combined trabeculectomy and phacoemulsification and found no significant differences at 6 months postoperatively in the level of IOP, number of medication, or complications. Recently Lemon et al114 have also reported no significant differences in postoperative mean IOP, mean number of medications, and visual acuity between limbal-based versus fornix-based conjunctival flaps in 69 patients with POAG who underwent trabeculectomy combined with phacoemulsification and IOL implantation with adjunctive use of mitomycin C. But there was a significantly higher incidence of postoperative hypotony with wound leak, in the limbal-based group (p = .019). Authors believe that this might be related to the excessive conjunctival manipulation that was necessary during cataract surgery because they had not found such a difference in a previous study on primary trabeculectomy and adjunctive mitomycin C with the same closure technique.115 The excessive conjunctival manipulation was responsible for inadvertent conjunctival wound defects that were not evident intraoperatively, but were leaking postoperatively leading to hypotony. In summary, it seems that there are no significant differences between limbal- and fornix-based conjunctival flap approaches.
How Is the Miotic Pupil Managed?
The miotic pupil is a common finding in glaucomatous eyes. There are several reasons for this troublesome situation. First, although there are many new antiglaucoma medications available, many patients still are under long-term miotic treatment. Second, elderly patients may have age-related miosis. Although in young people dilation is full, quick, and brisk, in the elderly it is usually slow and incomplete. Third, many eyes have developed posterior synechiae because fibrin, which is present in the aqueous due to a disturbed blood-aqueous barrier after miotic use, may produce iris adhesions to the lens. Fourth, pseudoexfoliation is a common finding, according to reports from Europe and Japan.116,117 In pseudoexfoliation, the pupil is atonic and does not dilate well.37 Also, inadequate pupillary dilation may occur during ocular surgery due to iris manipulation.
Adequate dilation is a prerequisite for a safe procedure whether planning an ECCE or phacoemulsification. A miotic pupil that does not respond to mydriatics can make cataract surgery extremely difficult and unsafe.38 Guzek et al,38 evaluating 1,000 ECCEs, found that decreased pupil size was the only statistically significant risk factor for vitreous loss (p = .0002). Also, even a well-dilated pupil may become constricted during surgery due to iris manipulations. For this reason, surgeons use 0.5 mL of epinephrine 1:1,000 in the infusion bottle to maintain adequate dilation or to achieve further dilation in eyes with borderline mydriasis.
Pupil enlargement can be achieved in different ways. The simplest way to open a fixed pupil is to break any posterior synechiae by first injecting viscoelastic agent in the anterior chamber and then breaking the adhesions with an iris spatula. Miller and Keener118 developed a procedure of stretching the iris by using a Graether collar button (Storz, St. Louis, MO) or any kind of a “push-pull” iris manipulator and lens positioning hook. The Graether collar button engages the pupil at the 6 o’clock position and pushes it down toward the limbus, while the lens hook engages the pupil at the 12 o’clock position and pulls it up to the limbus. Then the lens hook is inserted through a limbal stab incision at 3 o’clock position and it pulls the iris toward the limbus, while the Graether collar button manipulator stretches toward the 9 o’clock position. By using this stretch pupilloplasty technique, an additional 2 to 3 mm of dilation is achieved. Some pupils become atonic after this procedure.
Another way to manage a small pupil is to create a sector iridectomy through a prior peripheral iridectomy. This opens the pupil superiorly but multiple small sphincterotomies inferiorly may be necessary. Sector iridectomy can be repaired at the end of the procedure with 10-0 polypropylene (Prolene) sutures.119 This method, although good in ECCE, has been abandoned by phaco surgeons. Large-sector iridectomy usually creates excessive postoperative inflammation and posterior synechiae on the IOL. Also, during phacoemulsification the cut edges of the iris tend to be aspirated in the tip of the phacoemulsification handpiece or the irrigation-aspiration probe. If the patient is elderly or has posterior segment problems, it is acceptable to keep iridectomy unsutured and open for better view of the fundus. However, it may be cosmetically unacceptable. Fine and Masket33 have devised a system with a preplaced inferior iris suture and an inferior sphincterotomy to facilitate phacoemulsification. After breaking the synechiae, they use a 10-0 polypropylene suture on a straight needle that penetrates the inferotemporal limbus, proceeds through the inferior iris sphincter, and exits from the inferonasal limbus. Then they perform an inferior sphincterotomy followed by a limbal puncture at 6 o’clock, by which they remove both suture ends from the anterior chamber with a microhook. After completing phacoemulsification and implantation of a PC-IOL, the suture will be tied to close the sphincterotomy. If the surgeon decides to suture the iris, 10-0 or 11-0 polypropylene is the most appropriate suture material to use for iris repairing because it provides more permanent support than nylon.
Fine and Masket33 have also described another method that consists of multiple partial sphincterotomies after lysing any synechiae with a cyclodialysis spatula. The snips are about 0.50 to 0.75 mm long. These sphincterotomies can be done by using the Rappasso scissors. After their completion, the anterior chamber is further deepened with a viscoelastic material, resulting in pupil dilation of 6.00 mm in diameter. For more dilation, a Lester hook can be used too slowly stretch the pupil at each sphincterotomy site toward the iris root. The authors claim that postoperatively the pupil has relatively normal diameter, is easily dilated, and has a normal light reaction.
Another alternative is the use of de Juan flexible iris retractors120 made by Grieshaber (Schaffhausen, Switzerland). The retractor consists of a flexible hook made of nylon material and a Silastic slide. A viscoelastic agent should be used to deepen the anterior chamber and any synechiae should be lysed. The manufacturer claims that the retractors are strong enough to break even firmly adherent synechiae, yet flexible enough to prevent damage to the lens capsule. Four retractors are necessary and are easily placed through a self-sealing stab incision at a limbal site. They are adjusted to the appropriate position and tension and fixed with a flexible Silastic slide. At the end of the procedure, they can easily be unhooked from the iris and removed. The end of the hook will bend and slip out of the self-sealing incision. Additional time is required for hook insertion, and sometimes excessive pupillary stretching results in sphincter tears and subsequently atonic pupils. Entry into the anterior chamber should be at an oblique angle for better stretching of the pupil. A vertical entry, for example, will result in tenting of the iris and causing difficulties with phacoemulsification.
There are several pupil dilators also available. They are made of different materials—silicone, hydrogel, or polymethylmethacrylate (PMMA). Morcher (Stuttgart, Germany) type 5 S is a semicircular elastic PMMA ring, with an overall length of 7.5 mm, and with a 0.6-mm groove in which the pupillary edge enters. It provides a dilation of approximately 7.0 mm and it can be used in any type of corneal or limbal incision. It does not need additional incisions and, after removal at the end of surgery, intracameral acetylcholine may provide a fast and relatively normal reaction of the pupil. Pupil dilators should be used only with phacoemulsification and not with ECCE because the nucleus cannot be delivered through a fixed and nonflexible ring opening.
Finally, capsulorhexis and phacoemulsification can be done under a miotic pupil by using a viscoelastic agent and a Kuglen hook to lift and move iris. This procedure does require experience and the surgeon’s ambidexterity. The small-pupil techniques are listed in Table 20–5.
Epinephrine (0.5 mL of 1:1,000 in a 500-cc infusion bottle) |
Viscoelastic agents |
Breaking posterior synechiae |
Stretch pupilloplasty technique |
Iris retractors |
Multiple fine sphincterotomies |
Hook and capsulorhexis technique |
Pupil dilators |
Keyhole iridectomy |
Future Considerations
What Are the Future Considerations in Cataract and Glaucoma Management?
Although there are definite indications for the three options of management of cataract and glaucoma, namely cataract alone, combined surgery, and two-stage procedure, they constantly change due to continuing evolution and refinement of surgical techniques and the great variations in patients. The ideal procedure still does not exist, and the surgeon has to digest and combine the advances in optics, physics, physiology, pathology, and pharmacology.
There is a need for determining the best concentration and exposure time for antimetabolites. Belyea et al121 studied the results of combined phacoemulsification, lens implantation, and mitomycin C trabeculectomy procedure. They found that although there was excellent IOP control, a surprisingly high rate of progressive diffuse visual field loss was found. There were also two late endophthalmitis cases. The possible influence of mitomycin C in the above complications has to be clarified in further studies.
An interesting new alternative to filtering glaucoma surgery was reported by Jacobi et al122 in pseudoexfoliation glaucoma cases. They performed bimanual trabecular aspiration of pseudoexfoliation material in 42 eyes combined with ECCE or phacoemulsification. The aspiration was performed by using an aspirator with a tip of 400 μm in diameter and angled at 45 degrees to comply with the anatomic configuration of the anterior chamber angle. Following the entrance of the irrigation probe into the irrigation chamber, the aspirator was introduced through a limbal paracentesis and was pushed forward carefully in the opposite chamber angle and directed against the trabeculum. Under careful tip-tissue contact, and without visualization, suction pressure between 100 and 200 mm Hg was applied for 2 to 3 minutes. The same was repeated for the contralateral side of the chamber angle. The main advantage of trabecular aspiration over a standard filtering operation is that it increases outflow facility along the normal pathway. The procedure seems to be safe, promising, and efficacious in decreasing IOP, but a prospective, randomized multicenter study is necessary.
Recently, Teekhasaenee and Ritch123 reported results of combined phacoemulsification, PC-IOL implantation, and goniosynechialysis (GSL) in 52 eyes suffering from cataract and chronic angle-closure glaucoma with peripheral anterior synechiae (PAS) of less than 6 months’ duration. After completion of phacoemulsification and insertion of a PC-IOL, GSL was performed by using a blunt Swan knife under Barkan goniolens visualization. The mean extent of PAS was reduced from 310 to 60 degrees, and the IOP was reduced to less than 20 mm Hg in 47 eyes (90.4%) without medication. This procedure seems promising and the future will show its efficacy.
Foldable IOLs are now widely used in cataract surgery. However, there has been no clear evidence that IOL material has a clinically significant effect on the postoperative course of a combined cataract and glaucoma procedure. Kosmin et al85 compared silicone versus PMMA lenses in phacoemulsification combined with trabeculectomy and found that 1 year after surgery, IOP control was attained without medication in 80.0% in the silicone group and 76.7% in the PMMA group (p = 1.00), with no statistically significant early postoperative complications. Hollick et al124 reported that polyacrylic lenses were associated with a significant difference (p = .0001) of less posterior capsule opacification (10%) than silicone (40%) and PMMA lenses (56%) 3 years after cataract surgery. Again, a prospective randomized multicenter study, comparing all parameters of different foldable IOL materials, is necessary.
New research is targeting the search for materials to fill the capsular bag after cataract surgery, which would undergo hardening by polymerization from light exposure. Hettlich et al125 performed in vitro experiments on enucleated pig eyes and in vivo on rabbit eyes. However, they recorded temperatures as high as 45.1°C during the polymerization process. Therefore, refilling materials with better physical properties need to be developed.
References
22. McCarty CA, Wood CA, Fu CL, et al: Schizophrenia, psychotropic medication, and cataract. Ophthalmology 1999;106:683–687.
43. Roth M, Epstein DL: Exfoliation syndrome. Am J Ophthalmol 1980;89:477–481.
48. Anderson DR: Automated static perimetry. St. Louis: CV Mosby, 1992;80–82.
53. Chen HSL, Steinmann WC, Spaeth GL: The effect of chronic miotic therapy on the results of posterior chamber intraocular lens implantation and trabeculectomy in patients with glaucoma. Ophthalmic Surg 1989;20(ll):784–789.
79. Shields MB: Another reevaluation of combined cataract and glaucoma surgery. Am J Ophthalmol 1993;115:806–811.
91. Kass MA: Cataract extraction in an eye with a filtering bleb. Ophthalmology 1982;89:871–874.
93. Palmer SS: Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology 1991;98:317–321.
108. Katz LJ: Tube shunts for refractory glaucomas. In: Tasman W, Jaeger EA (eds). Duane’s Clinical Ophthalmology, Vol. 6, Revised Ed. Philadelphia: JB Lippincott, 1993;1–14.
117. Mizuno K, Muroi S: Cycloscopy of pseudoexfoliation. Am J Ophthalmol 1979;87:513–518.
125. Hettlich HJ, Lucke K, Asiyo-Vogel M, et al: Experimental studies of the risks of endocapsular polymerization of injectable intraocular lenses. Ophthalmology 1995;92:329–334.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree