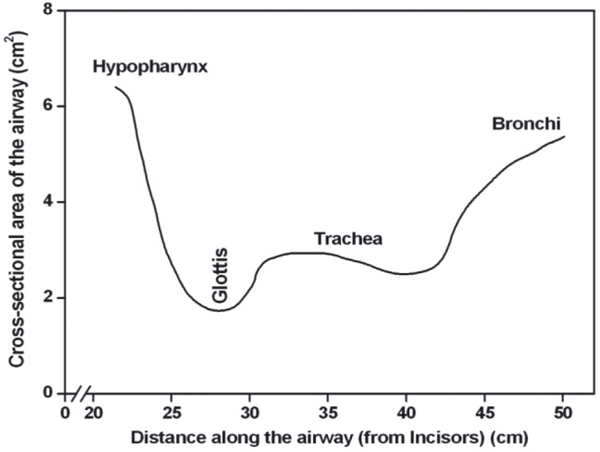
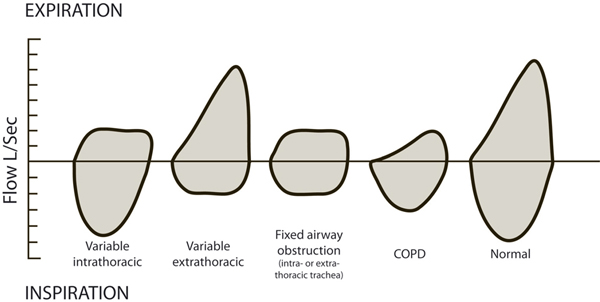
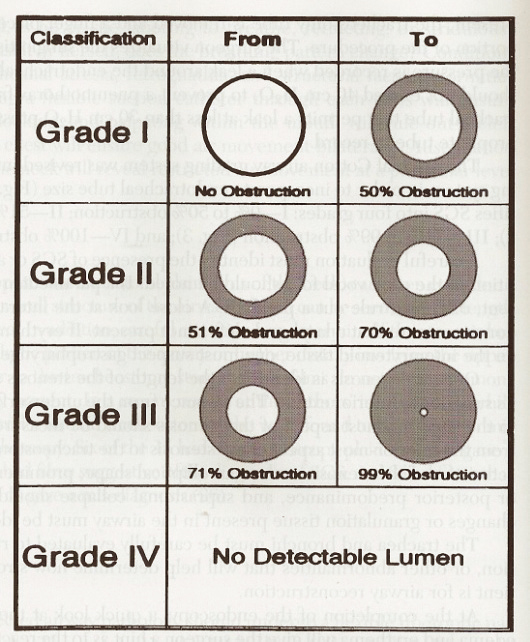
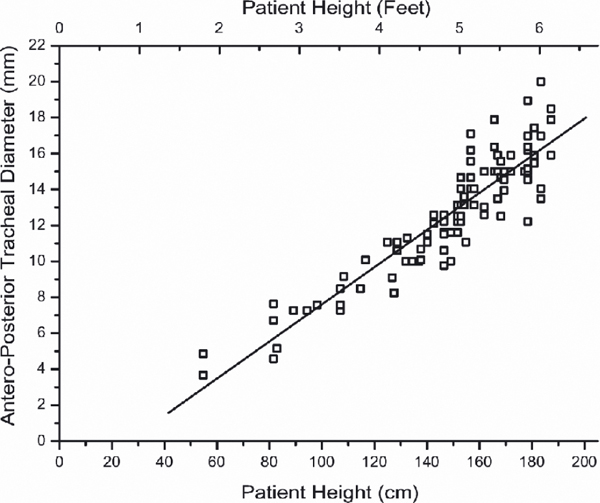
28 Management of Benign Laryngotracheal Stenosis in Adults The larynx, trachea, and bronchi form the conduit between the external environment and the lungs through which respiratory gases are transported and pulmonary secretions are expectorated. The principle function of the larynx is to protect the airway from aspiration during swallowing, but the larynx is also involved with phonation and the Valsalva maneuver. The narrowest sites of the adult airway are the larynx and trachea (Fig. 28.1). Upper airway stenosis can have a significant impact on the quality of life and sometimes on life itself. Abnormal narrowing of the laryngotracheal complex causes breathlessness, especially during physical activity. Retention of pulmonary secretions may lead to lung infection or collapse. Laryngeal stenosis can interfere with phonation and a dysfunctional larynx can affect swallowing safety. Due to medical advances, more patients are surviving periods of ventilation on intensive care units (ICUs).1,2 As a consequence, the incidence of laryngotracheal injury is probably increasing but remains unknown. Poiseuille law •R = resistance •n = viscosity •l = length •r = radius In laminar airflow, airway resistance is dictated by the diameter of the airway and by the density of the inspired gas (Poiseuille law). Because of the fourth power in the denominator, resistance increases rapidly as diameter decreases. However, an area of airway stenosis also produces turbulence, which adds to resistance, but cannot easily be calculated. During inspiration, the intrathoracic airways expand along with the expanding lungs. However, the extrathoracic trachea will have a reduced lumen during inspiration because the intraluminal pressure is lower than atmospheric. The reverse happens during expiration. A variable obstruction of the airway also changes size with breathing. Hence, an extrathoracic variable tracheal stenosis will limit inspiration, whereas an intrathoracic variable lesion will limit expiration. A fixed obstruction, whether intrathoracic or extrathoracic, will limit peak airflow on inspiration and expiration in equal proportions and produce a characteristic flow volume loop (Fig. 28.2).3 The exact physiological causes of dyspnea are not known; however, the extra work of breathing, altered afferent input from the respiratory tract, and the tendency toward carbon dioxide retention must play a role. Pediatric laryngotracheal stenosis is a well-researched area of medicine and treatments include airway augmentation with rib grafts as well as tracheal and cricotracheal resections. Adult laryngotracheal stenosis has been poorly researched and the surgical options include tracheostomy, tracheal resection, or cricotracheal resection.4 Some surgeons continue to use primary cartilage grafts to augment the adult airway. There has been little appreciation of the fact that there is a high incidence of ischemic necrosis of primary rib graft in adult patients.5 Furthermore, the quality and quantity of rib cartilage that can be harvested diminishes with age.5 Pediatric airway stenosis nearly always involves the subglottis6 and most commonly is due to prolonged endotracheal intubation. However, the lesional anatomy, anatomical sites, and pathologies behind adult laryngotracheal stenosis differ greatly from the pediatric group. The most widely used grading system to describe the degree of airway stenosis is the Myer-Cotton grading system,7 which refers to the surface area of the stenosis (Fig. 28.3) as opposed to the size of the patient’s airway. This grading system was developed to help decision making in pediatric airway surgery with respect to conservative or surgical treatments. In pediatrics, a decannulation is deemed a successful outcome and in the adult population, the outcomes are often graded as “excellent,” “good,” “satisfactory,” “failure,” or “death” with little mention of swallowing or voice outcomes. Table 28.1 illustrates the etiologies in 400 consecutive adult patients treated for benign airway stenosis by the National Centre for Airway Reconstruction in the United Kingdom. Of the relative etiological factors, more than half the cases of adult laryngotracheal stenosis were due to a period of ventilation on an ICU. The incidence of stenosis in patients who were ventilated with endotracheal tubes or converted earlier to tracheostomies was very similar, only the site of the injury differed. Early tracheostomy did, however, reduce the incidence of damage to the vocal folds and their mobility. Unlike pediatric laryngotracheal stenosis, which almost always affects the subglottis, in the adult population, one-third of the patients had stenosis of the cervical trachea. Nearly half of the adult patients had airway compromise due to other disease processes such as Wegener granulomatosis, sarcoidosis, and idiopathic subglottic stenosis (ISS). Figure 28.2 Patterns of flow volume loops3—these graphically depict the rate of airflow on the y-axis and the total volume expired (above) inspired (below) on the x-axis. The patient is asked to take the deepest breathe, apply the mouth to the device, and breathe out as hard as possible and for as long as possible. This is followed by a maximum and rapid inspiration. COPD, chronic obstructive pulmonary disease. The male larynx differs little in size from that of the female larynx until puberty. The adult male larynx undergoes significant growth and the adult female larynx undergoes a lesser degree under the influence of the hormones responsible for secondary sexual characteristics. The adult male larynx averages 44 mm in length and the adult female larynx averages 36 mm.8 The anteroposterior length in the adult male averages 41 mm, and 26 mm in the adult female. Contrary to traditional teaching, the diameter of the trachea relates to height regardless of sex (Fig. 28.4), both in children and adults.9 Table 28.1 Four hundred consecutive adult referrals with laryngotracheal stenosis

•48% Acquired laryngotracheal stenosis ○34.75% Subglottic stenosis ○13.25% Tracheal stenosis •14.75% Bilateral vocal cord mobility impairment ○8.75% Nerve injury ○4.75% Scar/fixation ○1.25% Rheumatoid arthritis •11.25% Wegener granulomatosis •9.75% Idiopathic subglottic stenosis •5.5% Supraglottic stenosis (2.5% sarcoid, 3.0% other) •3.25% Previous papillomatosis treatment •3.25% Glottic web •2.0% Tracheomalacia (1.25% relapsing polychondritis) •1.0% Amyloidosis •0.75% Vascular lesion •0.5% Subglottic stenosis congenital |
The trachea is a tube that spans between the lower border of the cricoid cartilage of the larynx, at the level of the sixth cervical vertebra, and the carina at the level of the sternal angle. At the carina, the trachea divides to give rise to the right and left main bronchi. In the adult, the trachea varies between 10 and 13 cm in length and in the adult is composed of approximately 20 C-shaped cartilaginous rings that are connected by fibrous bands and covered by respiratory mucosa. Posteriorly, the tracheal wall is composed of a flat fibromuscular structure that spans between the arms of the C and contains the unpaired trachealis muscle.10 The trachealis constricts the trachea during a cough allowing the high velocity passage of air during a cough.
Surgery and Anesthesia for Patients with Airway Compromise
Endoscopic airway assessment is performed by respiratory physicians, thoracic surgeons, and otolaryngologists. Pulmonologists and thoracic surgeons are trained to use both flexible and rigid bronchoscopes. Flexible bronchoscopy is usually performed in the spontaneous breathing and sedated patient who has had topical anesthetic applied to the upper aerodigestive tract. This technique allows assessment of the dynamic airway, the trachea, and bronchi with the ability to perform the full spectrum of interventions. However, with a flexible bronchoscope placed through a narrow stenosis, the patient’s airway becomes obstructed. Similarly, attempted dilatation of an airway stenosis leads to temporary airway obstruction. The rigid ventilating bronchoscope (Fig. 28.5) requires the patient to be paralyzed and ventilated by a face mask or endotracheal tube until the bronchoscope is inserted. For assessment of the airway beyond an area of stenosis, the bronchoscope has to be forced through the stenosis. This has the effect of dilating the stenosis, but it also causes stripping of the mucosa in a longitudinal fashion.
Neither flexible bronchoscopy nor rigid bronchoscopy allows prolonged access or endoscopic surgery on the larynx or subglottis.
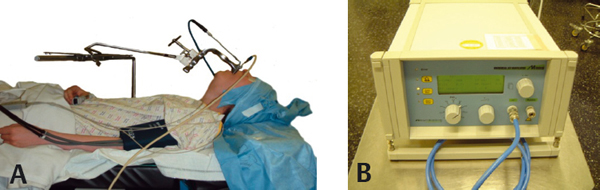
Suspension laryngoscopy is performed routinely by otolaryngologists for access to the supraglottic and glottic larynx. Laryngologists are also comfortable operating on the subglottis via the microscope or rigid endoscopes. The advantages of the microscope are binocular vision, depth of field, and superior axial illumination and it also allows two hands free for instrumentation. Also, the laser can be used with a “line-of-sight” technique through a micromanipulator attached to the microscope. Many otolaryngologists still use the ventilating bronchoscope for tracheal or bronchial assessment and surgery. Suspension laryngoscopy allows the use of both optical rigid endoscopes and flexible bronchoscopes to access the airway. The advantages are that the patient is paralyzed and the full spectrum of rigid instrumentation, dilators, lasers, and stents can be inserted and used with relative ease. As the patient is ventilated using a supraglottic jetting technique, lasers can also be used without the risk of airway fires (Fig. 28.6).
Pediatric airway surgery performed by an otolaryngologist differs in that the child is usually breathing spontaneously and oxygen or a combination of oxygen and an anesthetic gas is delivered by a nasotracheal tube withdrawn into the hypopharynx. Endoscopes and instrumentation can then be passed through the glottis to access the trachea and bronchi. This type of prolonged spontaneous breathing technique is not possible in an adult patient. Adults tend to lighten from anesthesia much quicker with the associated risk of laryngospasm. Also, access to the larynx in an adult is much easier in a paralyzed patient.
The senior author (G.S.S.) prefers a technique of suspension laryngoscopy and supraglottic jet ventilation via a cannula attached to the laryngoscope (Fig. 28.6). Fig. 28.7 demonstrates the differing views of the glottis in the same patient having supraglottic jet ventilation, subglottic jet ventilation, and a microlaryngoscopy endotracheal ventilating tube.
The jetting is delivered at high frequency (up to 100 jets per minute) using an automated device called Mistral (Acutronic, Switzerland). This device has built-in safety that sets an alarm if either the delivery of the jet or the return of gas is obstructed in the airway. No incidence of a pneumothorax has been reported when using this device in adult patients in our department over the past 10 years. This amounts to nearly 10,000 procedures. Pneumothorax has been reported when using jet ventilation delivered by a “manual jet” ‘Sanders type’ device.11 This is probably related to the fact that the delivery of the anesthetic agents is less well controlled and there is no safety cut-out mechanism.
Tracheobronchial Stenting
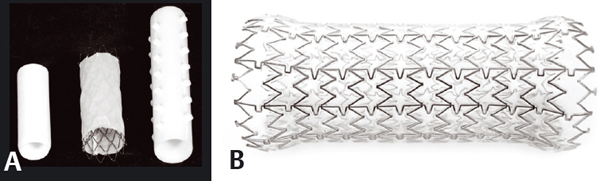
Charles Thomas Stent was a British dentist in the late 19th century. He developed dental impression material that was used as a template to support skin grafts for repair of oral trauma. Initially the term “stent” was used to describe artificial structures for preserving the viability and function of tissue. Today, the term is used to describe devices for maintaining the patency of tubular structures, including the tracheobronchial tree. Early experience of stents was gained through their use in the biliary tree, esophagus, urinary tract, and blood vessels. There has also been a proliferation of devices for airway stenting. There are currently a variety of silicone and expandable metal stents. The metal stents can be uncovered, covered, or partially covered (hybrid). Wire stents tend to be covered with polyurethane, although Teflon sheeting is used in some designs. The next generation of stents will be reabsorbable or bioengineered in other ways, negating the need for subsequent removal.
In benign and malignant disease, stents have been used to palliate the effects of large airway obstruction caused by extrinsic compression, endoluminal disease, or loss of cartilaginous support. Indications in benign disease include long length stenoses, failed previous repair, patient comorbidities that restrict reconstructive surgery, or patient preference. Stents are also used temporarily following airway surgery.
The first airway stent was a metal alloy stent described by William Hankins of St Louis, United States, in 1952.12 However, there were problems related to repeated obstruction and migration of this stent, which led to the development of the silicone T-tube, first used by Montgomery in the 1960s.13 The T limb prevented migration of the endoluminal tube. In 1982, Westaby et al described their modification of this silicone stent, which included a bifurcation at the lower end, allowing stenting of the trachea and both bronchi.14 In the 1990s, Dumon produced the first dedicated endobronchial silicone stent.15 Current metal stents tend to be made from steel or nitinol (a titanium and nickel alloy with a memory) wire mesh. The Gianturco metal stent is an uncovered stainless steel mesh stent and was first described in 1986.16
Although patients with metal stents enjoy immediate palliation of symptomatic tracheal stenosis, metal stents are associated with a high incidence of obstruction with granulation.17 They are also susceptible to metal fatigue and fracture over time. Based on personal experience and a review of the literature,18 the authors recommend that uncovered or hybrid metal stents should only be used in a select group of patients with a short life expectancy. If not removed within the first few weeks of deployment, they become a permanent fixture in the airway (Fig. 28.8).
Silicone stents also have complication rates, ranging from 21.5%19 to 42%.20 There is a high incidence of bacterial colonization of all stents, which can lead to granular tissue formation,21,22 the most common organisms being Staphylococcus aureus and Pseudomonas aeruginosa in most series. The difficulty in culturing the airway and stents by conventional flexible or rigid bronchoscopy is that the passage of these devices introduces contamination from oral and pharyngeal secretions. Our study was unique in that we used suspension laryngoscopy and an apneic technique for “clean” removal of the stent before starting supraglottic jet ventilation21 in a paralyzed patient.
Figure 28.7 Picture demonstrates the improving access to the posterior glottis and subglottis when ventilating with a (A) microlaryngoscopy endotracheal tube, (B) subglottic jetting catheter, and (C) supraglottic jetting.
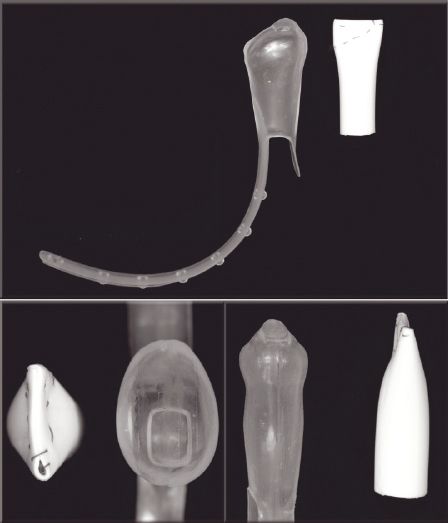
Figure 28.9 Two types of laryngeal stents. These have to be closed superiorly to prevent aspiration. Eliachar (Hood Laboratories, Pembroke, MA, USA) stent and over-sewn silastic T-tube (white).3
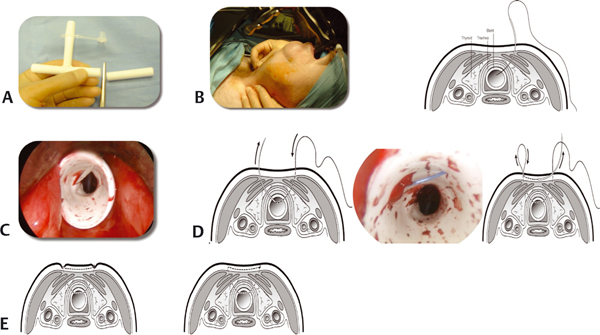
The senior author (G.S.S.) has more than 12 years of experience of using tracheobronchial stents of all designs. It is widely accepted that wire stents have a higher incidence of granulation formation, especially at their ends. Some authors report that silicone stents have a higher incidence of mucus plugging than wire stents (Fig. 28.9).17 However, this experience largely relates to the use of stents in the bronchi. In the upper trachea, bio fouling and mucus plugging are much greater in wire stents than in silicone stents. This may be due to the relative lower humidity in this area. The incidence of stent migration is widely reported as being higher in the subglottis than in the remainder of the tracheobronchial tree. The reason for this appears to be due to the fact that the subglottis is a fixed structure, which is narrower than the trachea, especially with the expansion allowed by trachealis. Hence, there is a natural tendency for stents to be pushed down. Stents placed high into the subglottis also run the risk of damaging the vocal folds and causing granulation in this area. There is very little data on migration rates of different tracheobronchial stents. Our unit has, for over 15 years, been using the vertical limb of a silicone T-tube as a stent (Fig. 28.10, A left). Different diameters of T-tubes are available and can be cut to a suitable length and are placed in the airway under general anesthesia and suspension laryngoscopy. The stent is held in place with a suture through the tissues of the neck (Fig. 28.11), which is buried under the skin.24
Figure 28.10 Various tracheal stents. Cut length of silastic T-tube (A left), partially covered wire stent (A middle), Dumon (Novatech, Cedex, France) silastic stent (A right), Aero expanding wire (Merit, Utah, USA) stent23 covered with polyurethane (B).
In our series, migration of this type of stent, following failure of the suture, occurred in 2:200 cases (1%) without detriment to the patient. This review included patients in whom the stent was left in for more than a year. This is the lowest migration rate of any endoluminal stenting device. The added advantage of using this stenting technique is that it is not reliant for its fixation on firm adherence to the tracheal wall. As a result, ciliary action continues to take place between the stent and the tracheal wall. This limits the degree of mucus plugging.
Insertion of Tracheobronchial Stents
Silicone stents usually have to be placed under general anesthesia, using a ventilating rigid bronchoscope. The team uses a technique of suspension laryngoscopy with supraglottic jet ventilation and placement of a silicone stent with rigid stent forceps. Visualization is assisted by a 0-degree, 30-cm Hopkins optical endoscope, which is 4 mm in diameter or a flexible bronchoscope. Wire stents come preloaded in delivery devices and can be passed parallel to a flexible bronchoscope in a spontaneously breathing, sedated patient, or using fluoroscopic screening techniques. Wire stents can also be inserted under general anesthesia. Stent removal is easiest using a general anesthetic technique. This allows the use of rigid biopsy or grasping forceps to firmly grip the stent even if embedded in granulation. Uncovered wire stents that have been in place more than 3 months will usually require an open surgical approach for removal.17
Figure 28.11 Securing an endoluminal silastic stent.24 The stent is cut from a length of silastic T-tube (A) positioned in the airway using suspension laryngoscopy (B). A monofilament suture with a large needle is used to secure the stent as shown (C, D). The ends bury themselves within a few days (E). For stent removal, the suture is divided endoscopically and removed through a small incision in the neck.
Postoperative Care of Tracheobronchial Stents
All patients with stents are prescribed saline nebulizers daily. Carbocysteine can be added in those patients in whom there is evidence of mucus plugging. There is no research evidence to support the use of any of these measures.
Etiology of Adult Postintubation Laryngotracheal Stenosis
In 1950, anesthesiologist, Peter Safar, established the concept of “advanced support of life,” keeping patients sedated and ventilated in an intensive care environment. During the polio epidemic in Copenhagen, Denmark, in 1952 (where paralyzed patients had to be ventilated for prolonged period), Bjorn Ibsen set up the first Intensive Care Unit (ICU).25 This led to an ever widening use of mechanical ventilation to treat respiratory failure. These iatrogenic lesions provided a whole new field of endeavor for surgeons. In the 1960s, scores of papers appeared in Europe and North America, describing surgical resection of postintubation strictures. Prevention of postintubation injury quickly became a priority once the origin of these lesions was evident. Initially, high-pressure cuffs were used and risked ischemic injury to the mucosa and necrosis of the cartilage of the trachea. Carroll et al in 1969 recommended a cuff with a large volume and low pressure, which only resulted in small increases in tracheal wall pressure with overinflation.26 Although the incidence of postintubation airway stenosis in post-ICU patients is unknown and can only be approximated between 1 and 4%,27–30 a significant early injury is evident in 47% of patients.31 This is despite the use of these high-volume, low-pressure cuffs on endotracheal and tracheostomy tubes (Fig. 28.12). This is the only paper in the literature where the trachea has been examined at the time of endotracheal tube removal. Unfortunately, it does not make the definition of “significant injury” clear.
The anatomical and pathological differences between stomal and cuff stenoses and other postintubation injuries were described at this time by Pearson et al and Grillo. They also stressed the importance of allowing florid inflammation to subside before the surgical correction.32–35 They demonstrated that surgical resection and anastomosis produced better results than repeated dilatation, steroid injection, or cryotherapy. The results of treating postintubation stenosis with resection by the same authors achieved an 87.5% “cure” in 200 patients in 1992. The definition of “cure” appears to include patients with a suboptimal airway. Couraud et al reported a 96% success rate in 217 patients in 1994, and Grillo et al cited a 94% success in 503 patients in 1995.4,36,37 They also described the correction of postintubation stenosis involving the subglottic area as being more difficult than lesions of the trachea. The etiology of postintubation stenosis injuries was initially unclear. At first it was thought to be due to irritation from the materials from which tubes and cuffs were made.38 Later it became clear that pressure necrosis from tubes and cuffs leading to circumferential injury and contracture was the principal explanation.39
The risk factors for laryngotracheal stenosis following a period of ventilation on the ICU include sizing of endotracheal tubes, excessive lateral cuff pressure due to poor cuff pressure monitoring, hypotension, local infection, duration of intubation, use of steroids and other causes of reduced patient immunity, patient movement and agitation, tracheostomies, and bilateral injuries of posterior vocal cords. The majority of patients ventilated on ICUs do not appear to develop airway stenosis. Although there are many etiological factors, patients who tend to scar excessively following injury may self-select for airway stenosis; however, there is no clinical study to support this.
With respect to endotracheal tubes, modern tubes are of a high volume and low pressure, design to reduce the risk of airway injury. To prevent ischemic damage, the cuff should not exceed a pressure greater than the capillary perfusion pressure of the mucosa. The mean capillary blood pressure is approximately 20 mm Hg. This is 27.2 cm H2O pressure.40 The recommendation is that the cuff inflation pressure, of a ventilation tube, should not exceed 30 cm. Seegobin and van Hasselt41 studied four types of large-volume, low-pressure cuff types. Following periods of endotracheal intubation, photographs were taken of the circumferential trachea at the site of cuff contact. Photographs were taken for varied cuff pressures after a period of 15 minutes. The conclusion of the study was that lateral wall pressures above 30 cm of water compromise mucosal capillary blood flow leading to pressure necrosis of the adjacent mucosa and eventually the cartilage.
The other risk factors for laryngotracheal injury in a ventilated patient on the ICU probably include gastric reflux, infection, coexisting health problems (such as diabetes mellitus and arteriopathy), and altered immunity as part of the stress response. There is, however, no research to support these as potential risk factors.
Posttracheostomy stenosis had been described as early as 1886 when Colles found four strictures in 57 patients treated for diphtheria.42 In the senior author’s (G.S.S.) series of 400 adult patients with benign laryngotracheal stenosis, the incidence of airway stenosis from endotracheal tubes was approximately the same as the incidence from tracheostomies. Damage to vocal fold anatomy and impairment of vocal cord mobility are more common with endotracheal tubes.43,44 Surgical management of bilateral vocal fold immobility is always a compromise between voice and airway. There is very little evidence supporting early tracheostomy on ICUs.45 The TracMan study was a multicenter UK study designed to look at the timing, morbidity, and mortality associated with tracheostomies on ICUs. Although the trial phase of this multicenter study took place in 2004, the main phase of the study failed to progress. Although this thesis cannot comment on the morbidity and mortality associated with early versus late tracheostomy, following review of the 400 patients in the database, some conclusions can be reached. There is a real risk of damage to the normal function of the glottis and vocal folds, which exists with endotracheal intubation that does not occur in patients with a tracheostomy. As the surgical results of restoration of impaired glottic function remain suboptimal, early tracheostomy would minimize the risk of glottis stenosis and bilateral vocal fold mobility impairment.
Surgery for Laryngotracheal Stenosis
The Rig Veda noted that the trachea could reunite “when the cervical cartilages are cut across, provided they are not entirely severed.” This description dates from circa 2000 BC. The earliest description of surgery for laryngotracheal stenosis was provided by L. von Schroetter in Vienna, Austria, in 1871. He described two techniques. The first involved the use of metal “olives” after placement of a tracheostomy. The second procedure was dilatation of the airway with hard rubber bougies delivered through the mouth.46,47 In 1885, O’Dwyer in New York48 described similar techniques of dilatation that became used widely in the United States. Gluck and Zeller in 1881 demonstrated healing after end-to-end tracheal anastomosis in dogs and believed that the technique could be applied in man.49 Primary anastomosis of the trachea after limited resection for posttraumatic stenosis was performed in man by Kuster in 1886.50 Nowakowski in 190951 described complex methods of repair of cervical tracheal defects and through cadaver studies placed the limit of tracheal resection at 3 to 4 cm. This was following cadaveric studies. It was many years later before Conley successfully resected the second and third tracheal rings for scar in 1953 with primary end-to-end anastomosis.52 In 1968, Grillo and Mulliken53 reported the length of trachea that could be resected for postintubation stenosis at 4.5 cm (~7.2 rings). He discovered that the length that could be resected in older patients was progressively shorter because of the reduced elasticity between the cartilaginous rings. He further demonstrated that it would be possible, with additional maneuvers involving release of pulmonary ligaments and suprahyoid laryngeal release, to resect a further 2 cm.53
Open approaches for the treatment of subglottic stenosis can be traced as far back as the late 1800s and early 1900s. Killian in Germany described an operation referred to as “laryngotracheostomy.”47 A vertical skin incision and a median vertical fissure of the larynx and trachea were created. A fistula was maintained and progressively larger, soft rubber tubes were inserted through the tracheostomy site. There is also a description in the German literature in 189654 describing the use of rib cartilage graft in a two-stage procedure to close an open tracheal wound. These original papers were essentially case reports but modifications of these techniques are still used in modern airway surgery.55
In 1927, M. F. Arbuckle27 in St Louis described his experience with three children who had been treated unsuccessfully with repeated intubations after a diphtheria throat infection. The larynx and subglottis were exposed after a median vertical incision through the skin and the airway. Arbuckle excised all visible scar tissue and placed a skin graft over the denuded area within the lumen of the airway. The graft was held in place with a rubber balloon attached inferiorly to a string that was brought out through the tracheotomy. He also described a similar technique with a balloon that was held by a stay suture from the outside, transfixing the larynx, graft, and balloon. In each case, the balloon was removed after 8 days.
Schmiegelow56 from Copenhagen described, in 1927, a surgical technique which he said he had been using since 1910. Via a laryngotracheal fissure, he entirely removed any structures or scar tissue encroaching on the lumen such that it appeared normal in size. He then placed a rubber drain slightly wider than the lumen, fixed into position using silver wire through the soft tissues and skin of the neck. This “stent” was left in place for several weeks or months.
Before the 1930s, the majority of stenoses of the airway resulted from infections and inflammatory processes. Often this was exacerbated by iatrogenic injuries from surgery. In 1921, Chevalier Jackson57 from Philadelphia, PA, United States, cautioned against the placement of a “high tracheotomy,” which he described as on or near the cricoid cartilage. LeJeune and Owens58 from New Orleans, LA, United States, noted in 1935 that 90% of their cases of laryngotracheal stenosis were caused by disease or trauma. They advocated complete dissection of all scar, granulation, cartilage, and osseous tissues via laryngofissure and application of a skin graft over a stent—their argument being that primary tissue healing where there is skin approximation produces less scar tissue than healing by secondary intention. Jackson in his article of 193646 stated that all cases of congenital or acquired stenosis of the larynx were curable. He also stated that the wearing of a canula (tracheotomy) would dominate the entire life of a person and create an inferiority complex. Jackson favored the placement of elastic rubber core molds that changed weekly and slowly increasing in size. These rubber stents were placed above the tracheotomy. Jackson admonished the cutting of the cricoid cartilage even in laryngeal atresia as “it is the only complete ring in the airway.” Some of the principles described by Jackson are part of modern laryngology teaching.
In 1938, Edward Looper from Baltimore, Maryland, United States, described the use of the hyoid bone as an autologous material for grafting in airway reconstruction. He described it as being advantageous over the use of rib or ear cartilage.59 This is the first reference to cartilaginous graft tissue for airway reconstruction. In addition to performing the first tracheal resection in 1953, John Conley of New York52 summarized several techniques for treatment of subglottic stenosis. He performed a laryngofissure, removed all scar tissue, and placed a split skin graft, over a petroleum jelly gauze, over a foam rubber sponge. He also mentioned that autologous cartilage could be used to assist in reconstructing the tubular form of the trachea. He did not discuss specific cases, but the ideas are in use in pediatric airway reconstruction today.60
In 1971, Grahne of Helsinki61 continued to completely remove scar tissue, but described a hole placed through an Aboulker stent to accommodate a metal tracheostomy tube. This stent was left in place for 4 months. By the 1970s, the principal cause of airway stenosis was no longer infectious diseases, high tracheostomies, or surgical dilatations. The principal cause then was a period of prolonged ventilation using an endotracheal tube. In 1972, Fearon and Cotton in Toronto62 published an experimental procedure where thyroid cartilage was used to augment an anteriorly split thyroid cartilage in a monkey. They also demonstrated that there was no inhibition of laryngeal growth following this. In 1974, Evans and Todd in London63 reported the use of rib cartilage in laryngotracheoplasty, but favored a castellated laryngofissure to expand the airway over a piece of rolled silastic sheet used as a stent for 6 weeks. Cotton in Cincinnati (Ohio, United States) in 197855 described in detail laryngotracheal reconstruction (LTR) with an anterior costal cartilage graft. Later, in 1984, Cotton64 published a series of 100 cases of LTR in children over a decade. He emphasized that the stenosis should be mature before undertaking open surgery. In 1985, Fearon and McMillin in Toronto, Ontario, Canada,65 described cricoid resection and thyrotracheal anastomosis in primates. They demonstrated that there was no interference with normal laryngeal growth following this. Ranne et al in Kansas City (MO, United States) are credited with the first cricoid resection in patients,66 published in 1991. This procedure, originally described by Pearson et al,67 was adopted by Monnier et al in Switzerland, who subsequently published their series in 1993.68 Robin Cotton’s group in Cincinnati, when considering an open procedure for subglottic stenosis, primarily perform anterior and posterior augmentations. In only 15% of cases, usually those that have failed augmentation surgery, do they consider cricotracheal resection.
One other technique, originally described by Herberhold et al,69 was the use of preserved tracheal allografts. These held the promise of being able to treat long-segment tracheal stenosis in children and adults without the need for immunosuppression. These grafts consisted of chemically treated cadaveric tracheas to remove donor cells and antigenicity. The simplicity of the technique was the ability to tailor the size and shape of the tissue to suit the patient’s requirements. However, like other teams70,71 our unit discovered that, following an intense inflammatory response lasting several weeks, these grafted tracheas were replaced in time by host scar tissue. When the technique worked, it appeared to do so if the scar tissue retained the size and shape of the original graft. Publications by Herberhold et al did not give detailed follow-up data to allow full appreciation of the long-term results.
Resection of the damaged airway had become the “gold standard” for treating laryngotracheal stenosis in adults at the start of this research. Grillo59 had the largest experience of this technique in adult patients and most other publications were case series. He achieved “successful” outcomes in the majority of his patients; however, the possibility of bias based on patient selection cannot be ruled out. These results are all the more difficult to interpret as there were no standardized and validated outcome measures in widespread use. As Abraham Maslow,72 a psychologist, wrote in 1966, “it is tempting, if the only tool you have is a hammer, to treat everything as if it were a nail.”
Endoscopic Approach to Postintubation Subglottic and Tracheal Stenosis
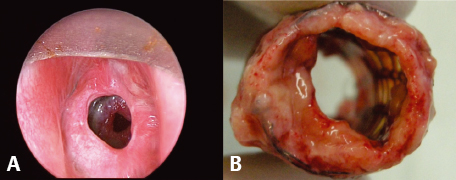
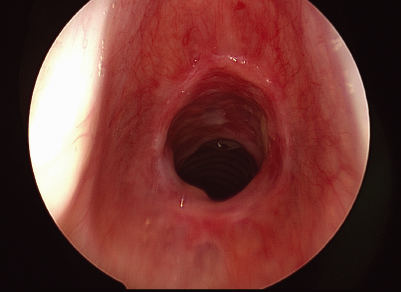
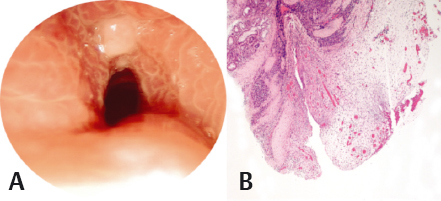
In clinical practice, the majority of patients with postintubation upper airway stenosis have mature fibrotic airway scars with minimal evidence of ongoing airway inflammation. These patients typically have had an intubation episode in the relatively distant past and some of them have been treated for “adult onset asthma” for some time before the diagnosis is secured. Less commonly, patients are referred within a few weeks of extubation with airway symptoms during the active fibroinflammatory phase of tracheal injury (Fig. 28.13).
These two presentations occur at different times within the natural history of the same disease process. The early phase of the postintubation airway stenosis is characterized by mucosal ulceration and perichondritis followed by the formation of exophytic granulation tissue. As healing progresses, granulation tissue is gradually replaced with mature fibrotic tissue and the wound contracts giving rise to the classical picture of mature airway scar (Fig. 28.14). It has been shown that inflammatory conditions in the airway do respond to intralesional steroids.30 Using suspension laryngoscopy and supraglottic jet ventilation, up to 3 mL of methylprednisolone acetate (40 mg/mL) can be injected into the stenosis. Radial cuts are then made into the stenosis with the carbon dioxide laser (8 to 10 W continuous) delivered through the microscope using a line-of-sight technique. The lesion is then dilated using a pulmonary balloon dilator to the size of the adjacent normal airway. With more mature and fibrotic lesions, intralesional steroids are of limited value. In these cases, radial cuts into the lesion are followed by balloon dilatation and topical mitomycin-C application may be considered. Endoscopic surgery is repeated every 3 to 4 weeks. Patients whose lesions prove recalcitrant to endoscopic therapy, and this usually became evident by the third procedure, should be treated with open laryngotracheal reconstruction or tracheal resection techniques. Also, where there is collapse and damage to the laryngotracheal cartilaginous structure, open surgical techniques should be considered, as endoscopic techniques are likely to fail. Fig. 28.15 shows the overall success rate of the endoscopic approach to airway stenosis (n = 62) of 72%. Patients with a body mass index of greater than 45 failed endoscopic airway surgery.73
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree