General Considerations
Each year, 11,000 new cases of larynx cancer will be diagnosed in the United States (1% of new cancer diagnoses), and approximately one-third of these patients will die of their disease. The current male-to-female ratio for larynx cancer is 4:1, but the relative percentage of women with this, as with other smoking-related illness, has been on the rise. Larynx cancer is most prevalent in the sixth and seventh decades of life and is more prevalent among lower socioeconomic groups, for whom it is often not diagnosed until more advanced stages. More than 90% of larynx cancer is squamous cell carcinoma (SCC) and is directly linked to tobacco and excessive alcohol use. Because of the complex and multifaceted nature of this disease, treatment planning is best delivered through a multidisciplinary tumor board format.
Anatomy
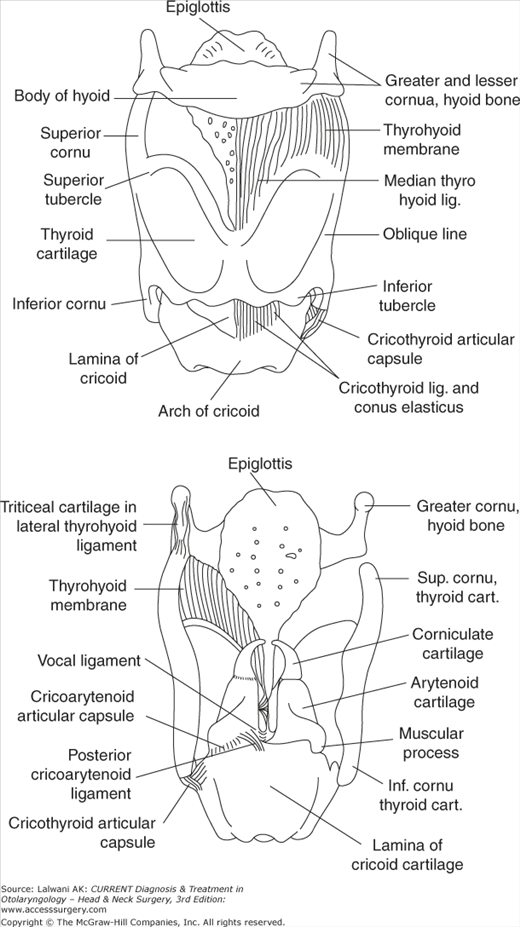
The larynx functions not only to produce voice but also to divide and protect the respiratory tract from the digestive tract. It acts as a sphincter during deglutition, protecting against the penetration of bypassing food by closing off the trachea at two sites: the epiglottic flap and the closure of the vocal cords. The larynx consists of a framework of cartilages connected by ligaments, membranes, and muscles covered by a respiratory and stratified squamous mucosal epithelium (Figure 31–1).
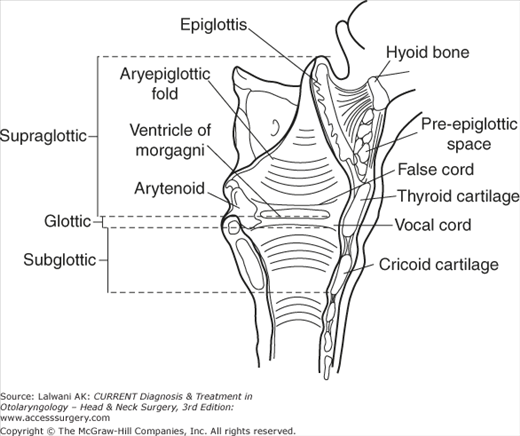
The larynx can be divided into three parts: the supraglottis, the glottis, and the subglottis (Figure 31–2). The supraglottic larynx extends from the tip of the epiglottis and vallecula superiorly to the ventricle and undersurface of the “false” cords inferiorly; it includes the arytenoid cartilages, the aryepiglottic folds, the false vocal cords, and the epiglottis. The glottic larynx encompasses the “true” vocal cords, extending from the ventricle between the true and false cords to 0.5 cm below the free edge of the true cords, including the anterior commissure and interarytenoid area. The subglottic larynx extends from the inferior extent of the glottis to the inferior edge of the cricoid cartilage.
Understanding the embryologic origin of these regions of the larynx helps to explain the difference in clinical behavior between cancers arising from these laryngeal subsites. The supraglottis derives from the midline buccopharyngeal primordium and branchial arches 3 and 4 with rich bilateral lymphatics. The glottis, on the other hand, forms from the midline fusion of lateral structures derived from the tracheobronchial primordium and arches 4, 5, and 6. There is a paucity of lymphatics and, compared with supraglottic primary neoplasms, malignant glottic tumors have less of a tendency for bilateral regional lymphatic spread and remain confined to the glottis for longer periods of time.
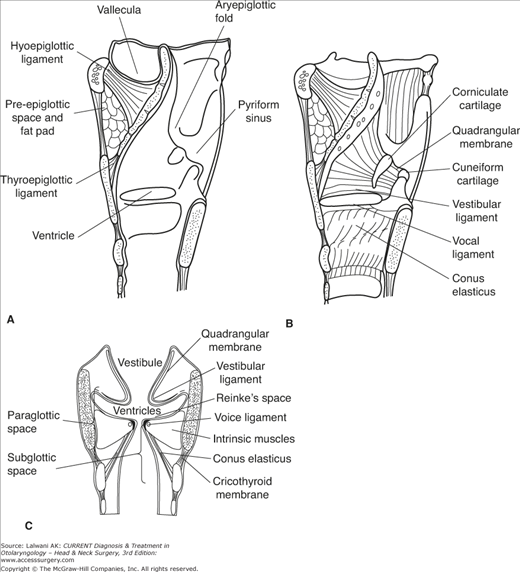
Fibroelastic membranes and ligaments further divide the larynx into the preepiglottic and paraglottic spaces. These structures, including the conus elasticus, the quadrangular and thyrohyoid membranes, and the hyoepiglottic ligament, act as barriers to the spread of tumor (Figure 31–3). The thyroid and cricoid cartilages and their perichondrium are further barriers to tumor spread. The anterior commissure tendon (Broyle’s ligament) and thyroepiglottic ligaments are not effective barriers to tumor spread, and tumors involving the anterior commissure are more likely to have direct regional spread.
Figure 31–3.
Laryngeal membranes and ligaments act as barriers to tumor spread and define the paraglottic and preepiglottic spaces. (A) Sagittal view, with mucosa intact and mucosa removed and (B) coronal view. (Reprinted, with permission, from Tucker HM. The Larynx. Thieme Medical Publishers, 1987.)
The muscles of the larynx are divided into intrinsic and extrinsic groups. The intrinsic muscles are those of the vocal cords and cartilages contained within the larynx itself. The extrinsic muscles, the strap muscles and constrictors, help with laryngeal elevation and pharyngeal constriction. Innervation of the intrinsic muscles is from the recurrent laryngeal branches of the vagus nerve on both sides. Arterial blood supply is from the external carotid artery and off the thyrocervical trunk via the superior and inferior thyroid arteries. Venous drainage is into the internal jugular vein. Lymphatic drainage is to levels II, III, and IV, as well as sometimes to level VI of the neck.
Pathogenesis
More than 90% of patients with larynx cancer have a history of heavy tobacco and alcohol use. Cigarette smoke, in particular, is a risk factor for cancer of the larynx. The combination of smoking and alcohol use has a more than additive carcinogenic effect on the larynx.
Other risk factors have been identified. Laryngeal infection with the human papillomavirus (HPV) results in laryngeal papillomatosis, which is usually benign, but subtypes 16 and 18 are known to degenerate into SCC. Gastroesophageal reflux has been implicated; however, a causal relationship with laryngeal cancer is still uncertain, although therapies directed at suppressing acid appear to decrease the recurrence of laryngeal cancer. Various occupational exposures and toxic inhalations (such as asbestos and mustard gas), nutritional deficiencies, and previous neck irradiation have all been linked to larynx cancer as well.
Increasingly, molecular and genetic markers of malignant potential, degeneration, and metastasis are being identified, unlocking the genetic causes of larynx cancer. Attention is being paid to predictors of clinical outcome and the response to specific therapy. Once these pathways are fully understood, gene therapy and other novel therapeutic approaches can be developed. Genes and gene products being investigated for their link to larynx cancer include p53, the Bcl-2 family of genes, and other markers of apoptosis, proliferating cell nuclear antigen (PCNA), Ki67, cyclin D1, the ras gene and other oncogenes, tumor suppressor genes, and the loss of heterozygosity and changes in the DNA content of tumors.
Epidemiology
Malignant disorders of the glottic larynx outnumber those of the supraglottis (ie, 1.5:1.0) in the United States (Table 31–1). This ratio does not hold worldwide. In Finland, for example, supraglottic cancers outnumber glottic cancers. The worldwide variation in the epidemiology of larynx cancer may reflect local tobacco and alcohol use customs, other environmental factors, or also the genetic makeup of the populations affected.
Malignant disorders arising in the subglottis are universally rare. For this reason, data on the incidence of nodal metastases and prognosis are scant, and the discussion of the diagnosis and management of larynx cancers that follows focuses on primary supraglottic and glottic cancers. Most larynx cancers involving the subglottis are extensions of primary cancers arising in the glottis or supraglottis.
As explained above, cancers arising in the supraglottic larynx have a richer lymphatic drainage and are more often diagnosed with nodal metastases and, therefore, at a higher clinical stage (Table 31–2).
Prevention
Many studies address the protective effect of retinoids, beta-carotene, and other antioxidants against the development of larynx cancer. A reversal of laryngeal leukoplakia after treatment with retinyl-palmitate has been demonstrated.
Staging
Cancers of the larynx are staged according to the TNM (tumor, node, metastasis) system of the American Joint Committee on Cancer (Table 31–3). For staging purposes, positive neck nodes are considered locoregional metastases; metastases to other parts of the body (such as lung, mediastinum, liver, and bone) are considered distant. According to the 2010 update, T4 tumors are now divided into T4a or moderately advanced local disease & T4b or very advanced local disease. Stage IV tumors are still subdivided into Stages IVA, IVB, and IVC (distant metastases present). Studies before this date, however, are based on the 1998 or earlier systems in which there was a single umbrella T4 and Stage IV designation. Accordingly, the discussion in the rest of this chapter refers to the older system.
| Supraglottis | |||
| T1 | Tumor limited to one subsite of supraglottis | ||
| T2 | Tumor involving more than one adjacent subsite of supraglottis, glottis, or region outside the supraglottis (vallecula, tongue base, medial wall of pyriform sinus) | ||
| T3 | Tumor causes vocal cord fixation and/or invades preepiglottic space, postcricoid area | ||
| Moderately advanced local disease | |||
| T4a | Tumor invades through thyroid cartilage, and/or invades tissues beyond the larynx | ||
| Very advanced local disease | |||
| T4b | Tumor invades prevertebral space, encases carotid artery or invades mediastinal structures | ||
| Glottis | |||
| T1 | Tumor limited to vocal cord; may involve anterior or posterior commissure | ||
| T2 | Tumor extends to supraglottis, glottis, and/or impaired vocal cord mobility | ||
| T3 | Vocal cord fixation | ||
| Moderately advanced local disease | |||
| T4a | Tumor invades through thyroid cartilage, and/or invades tissues beyond the larynx | ||
| Very advanced local disease | |||
| T4b | Tumor invades prevertebral space, encases carotid artery or invades mediastinal structures | ||
| Subglottis | |||
| T1 | Tumor limited to the subglottis | ||
| T2 | Tumor extends to vocal cord with normal or impaired mobility | ||
| T3 | Vocal cord fixation | ||
| Moderately advanced local disease | |||
| T4a | Tumor invades through cricoid or thyroid cartilage, and/or invades tissues beyond the larynx | ||
| Very advanced local disease | |||
| T4b | Tumor invades prevertebral space, encases carotid artery or invades mediastinal structures | ||
| N0 | No cervical lymph nodes positive | ||
| N1 | Single ipsilateral lymph node ≤3 cm | ||
| N2a | Single ipsilateral lymph node >3 cm and ≤6 cm | ||
| N2b | Multiple ipsilateral lymph nodes, each ≤6 cm | ||
| N2c | Bilateral or contralateral lymph nodes, each ≤6 cm | ||
| N3 | Single or multiple lymph nodes >6 cm | ||
| M0 | No distant metastases | ||
| M1 | Distant metastases present | ||
| Stage | T | N | M |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III | T3 | N0 | M0 |
| T1–3 | N1 | M0 | |
| IVA | T4a | N0–2 | M0 |
| T1–4a | N0 | M0 | |
| IVB | T4b | any N | M0 |
| any T | N3 | M0 | |
| IVC | any T | any N | M1 |
A shortcoming of the TNM staging system, which the subdivision of the T4 and Stage IV categories is starting to address, is that tumors of varying size and prognosis are frequently categorized together. Other indicators of the prognosis in laryngeal carcinoma have been identified and proposals exist to incorporate these into staging systems. These indicators include the following: (1) the histological characteristics of the tumor, such as extracapsular spread in nodal metastases, angiolymphatic invasion, perineural spread, and a high histological grade; (2) various chromosomal and molecular markers, such as p53 mutations, Ki67 or PCNA overexpression, DNA content, and loss of heterozygosity; and (3) the presence of patient comorbidities.
Clinical Findings
Signs and symptoms of malignant laryngeal lesions include hoarseness, dysphagia, hemoptysis, a mass in the neck, throat pain, ear pain, airway compromise, and aspiration.
Because only the slightest change in contour, thickness, or vibratory characteristics of the vocal cord results in perceived changes in the voice (namely, hoarseness), glottic larynx cancers often come to medical attention while still at an early stage. Patients with supraglottic cancers, however, typically present at a more advanced stage because tumors are bulkier (ie, at a higher T stage) before voice changes, dysphagia, airway compromise, or aspiration become apparent. Furthermore, because the supraglottis has a richer lymphatic supply, supraglottic primary lesions tend to metastasize earlier and are more often diagnosed at the advanced N stage. Clinical cervical adenopathy at the time of diagnosis portends a poor prognosis and advances the overall stage. Significant weight loss often accompanies the diagnosis of an advanced larynx cancer because of swallowing difficulties. Of note, throat and ear pain are usually symptoms of advanced-stage tumors.
When a larynx cancer is suspected, complete head and neck examination is performed, focusing on the larynx and the neck. The quality of the voice is noted. A breathy voice may indicate a vocal cord paralysis and a muffled voice, a supraglottic lesion.
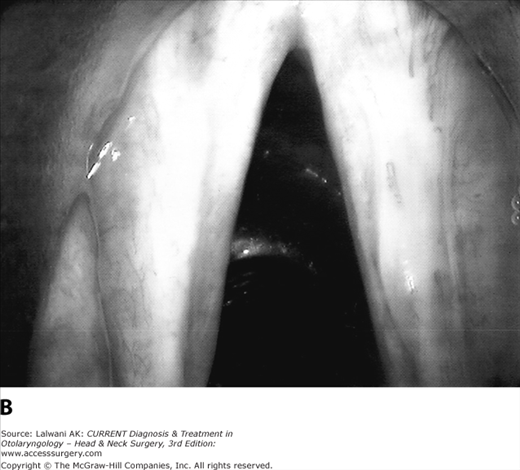
Laryngoscopy (or visualization of the larynx) is done in the office setting using either a laryngeal mirror (indirect laryngoscopy) or a fiberoptic endoscope. Irregularities in the contour, color, vibratory characteristics, and mobility of the vocal cords are noted. Malignant laryngeal lesions can appear to be fungating, friable, nodular, or ulcerative, or simply as changes in mucosal color (Figure 31–4). A stroboscopic video laryngoscopy can highlight subtle irregularities in the mucosal vibration, periodicity, and closure of the vocal cords. Careful attention must be paid to the airway status. Some large, bulky lesions require urgent airway intervention with either intubation, tumor debulking, or tracheotomy. Direct laryngoscopy is performed under general anesthesia and provides the definitive examination of tumor extent.
The neck is examined by palpation for enlarged lymph nodes and by noting their location, size, firmness, and mobility. Restricted laryngeal crepitus (the “clicking” movement from side to side across the pharynx and prevertebral fascia) can reveal postcricoid or even retropharyngeal invasion.