Chapter 55 Macular Telangiectasia
History, nomenclature, and classification of macular telangiectasia
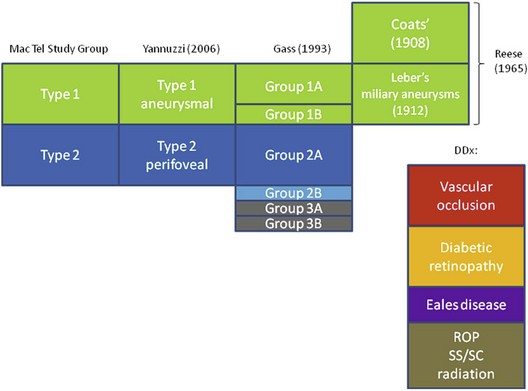
The concept of “retinal telangiectasia” has been known for over a century. First alluded to by Graefe in 1808 as “Telangiectasie der Retina” and/or “Aneurismen der Zentralarterie,” it was used to describe dilated retinal vessels on all three components of the circulation, arterioles, capillaries, and venules for a variety of abnormalities, mostly cutaneous and cutaneous-ocular in nature.1 One hundred years later, in 1908, Coats described “exudative retinitis,” which was best characterized as vascular abnormalities with massive subretinal exudation.2 Today, congenital telangiectasia goes by his name, Coats disease, and it consists of dilated retinal capillaries, micro- and macroaneurysms, ischemia, nonperfusion, and retinal vascular leakage, usually unilateral in males. Four years after Coats’ original description, Leber described “miliary aneurysms,”3 which were quite similar clinically to cases seen by Coats. It was not until 1956 that Reese suggested that Coats disease and Leber miliary aneurysms were one and the same, occurring either in child or adulthood.4 By 1968, Gass acknowledged the contribution by Reese, suggesting that Leber and Coats were indeed manifestations along the spectrum of one disease, but Gass also introduced a new distinct entity, which he called idiopathic juxtafoveolar retinal telangiectasis (IJRT),5 in order to differentiate it from Coats disease. This resulted in an extensive, detailed classification in 1993.6 Table 55.1 puts the various diseases and their classifications in context.
Table 55.1 Various Classifications of Macular Telangiectasia (Types 1 and 2) and the Differential Diagnoses
DDx, differential diagnosis; ROP, retinopathy of prematurity; SS, sickle cell disease; SC, sickle cell trait.
Classification
Gass classified what had previously been known as Leber miliary aneurysms into IJRT groups 1A and B; this distinction proved to be useful in terms of prognosis and therapy. IJRT group 2 was to include the common bilateral disease seen in older and elderly patients, but later a group 2B was created to accommodate two brothers, who developed subretinal neovascularization, although these two remain the only cases fitting this category.6 Another group was introduced and subdivided into IJRT group 3A, which is characterized by telangiectatic changes, vascular occlusion, and minimal exudation in 3 patients, and group 3B, who had similar retinal changes but had additional neurological changes in 3 patients also.
Yannuzzi classification
In 2006, Yannuzzi discussed new diagnostic, adjunctive imaging systems such as optical coherence tomography (OCT) and high-speed stereo angiography in a cohort of 36 patients with mac tel of various types. He introduced the name “idiopathic macular telangiectasia.”7 He proposed to pool together mac tel types 1 A and B and to classify them as “aneurysmal” telangiectasia. Gass group 2A mac tel was preserved but, because of the lack of subjects in the other categories, types 2B, 3A, and 3B were eliminated in this classification.
Epidemiology
Prevalence of disease: estimates from population-based studies
Beaver dam eye study
The Beaver Dam Eye Study8 regraded the stereoscopic fundus photographs of the eyes of 4926 subjects aged 43–84, 99% of whom were white, for mac tel type 2. Five individuals, one woman and four men, were identified to have mac tel type 2, which translates into a prevalence of 0.1%. The average age was 63 years, with a range from 52 to 68 years. Bilateral manifestations were found in 2 patients.
Melbourne collaborative cohort study
This Australian study9 analyzed 22 415 Caucasians, with regard to the presence of typical features of mac tel type 2 on nonmydriatic color fundus photographs. Twelve patients with “possible” unilateral mac tel type 2 and 5 patients with signs of bilateral mac tel type 2 were identified. The average age amongst bilateral cases was 63 and ranged from 53 to 72 years. Three of the 5 bilateral cases were female. Only one “very convincing case with early gray sheen and telangiectatic vessels temporal to the fovea” was reported. The authors concluded that the incidence in their studied population ranged from 0.0045% to 0.022%, a prevalence which is significantly lower than the one found in the Beaver Dam Eye Study.
As noted by Klein et al., this lower prevalence estimate found in the Australian population might be a result of using a screening protocol in which images were only reassessed specifically for mac tel type 2 if a previous grading had suggested at least one feature of the disease8. The Beaver Dam Eye Study was conducted by regrading the entire cohort. It is possible that both studies have underestimated the true prevalence because only color fundus images were available. Other imaging technologies such as fluorescein angiography (FA), OCT, or fundus autofluorescence (FAF) have been demonstrated to be sensitive in detecting early and asymptomatic disease stages of mac tel type 2.10
Although Gass and Blodi did not find gender differences in their cohort of 140 patients (94 with mac tel type 2),6 the proportions of women reported by the Mac Tel Project (n = 310) and by Yannuzzi were about 64% and 58%, respectively.11 On average, the Mac Tel Project participants (mean age 61 ± 9 years) had their disease diagnosed at age 57 (± 9 years).
Clinical presentation
Fundus appearance
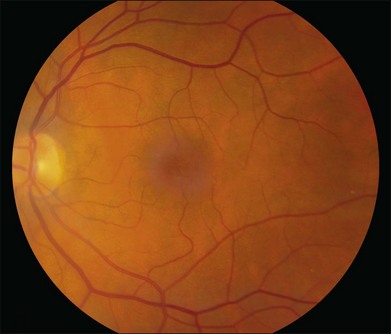
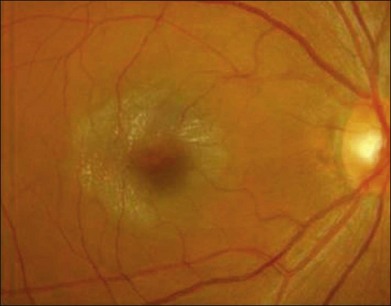
The disease tends to be bilateral, but one eye may be more advanced than the other. All lesions tend to begin temporal to the foveal center but may subsequently involve the entire parafoveolar area. The earliest fundoscopic manifestion of mac tel type 2 is a subtle loss of retinal transparency in the perifoveal region, beginning temporally (Fig. 55.1).7 This becomes more pronounced over time, and dilation of the parafoveal capillaries in the temporal parafoveal area ensues, and may extend to surround the fovea. These mildly ectatic capillaries were described to affect mainly the deeper capillary network (Fig. 55.2).6 However, others have identified involvement of both the inner and outer retinal circulation.7 In contrast to mac tel type 1, retinal hard exudate is not seen unless there is evidence of neovascularization. Crystalline deposits at the vitreoretinal interface may be seen throughout the course of the disease (Fig. 55.3).6,12
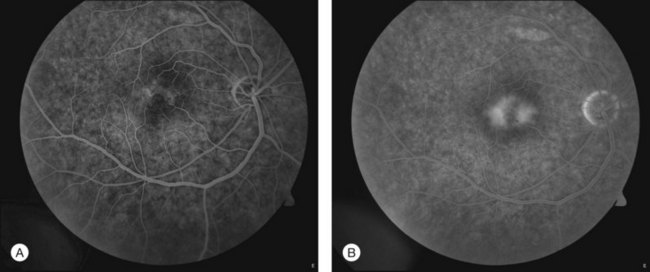
Fig. 55.2 (A) Early fluorescein angiographic findings of macular telangiectasia type 2 and (B) late leakage.
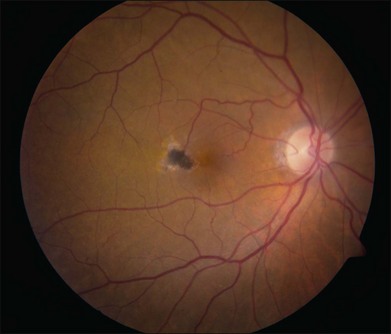
Blunted, dilated venules, either as single or multiple vessels, are often associated with ectatic capillaries. As vessels course towards the fovea, they usually decrease in diameter but, in mac tel type 2, they dilate and may make a right-angle turn, diving into the deeper retinal layers (Fig. 55.4). Eventually, intraretinal pigment migration and RPE hyperplasia along these diving dilated venules may occur7 (Fig. 55.5). In addition to RPE cell migration, atrophic changes in the neurosensory retina are another frequent finding.
A yellow spot, or vitelliform lesion, in the center of the fovea with slight loss of the foveal depression may become apparent in some eyes.7 Other foveal changes include lamellar or full-thickness macular holes that have been detected on clinical exams and some confirmed by OCT imaging.7,13–17 The degeneration and atrophy associated with this disease contribute to the formation of such holes. Surgical repair may not necessarily result in either structural or functional improvement.
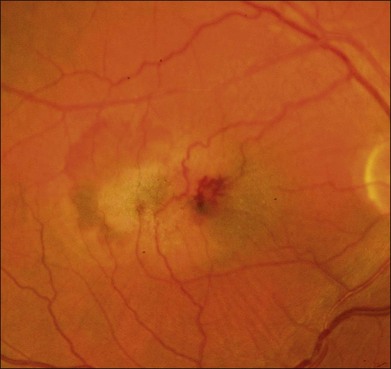
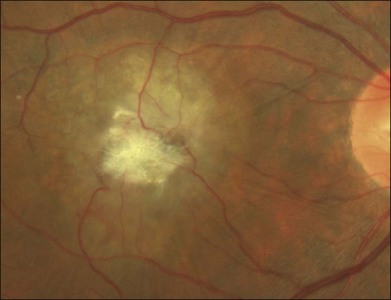
The development of neovascularization is often, but not always, preceded by the right-angle venule and the intraretinal pigment hyperplasia which is often temporal to the fovea.6,7 The neovascularization is most commonly seen temporal to the fovea.18 Retinal hard exudates, intraretinal edema, and subretinal or intraretinal hemorrhage may occur (Fig. 55.6). These neovascular complexes are retinal in origin, as seen by the feeder vessel from the retinal arteries and the drainage into venules (Fig. 55.7). This may be indistinguishable from choroidal neovascularization with chorioretinal anastomosis. A disciform scar may be the advanced stage of this process (Fig. 55.8).
Retinal imaging
Fundus autofluorescence
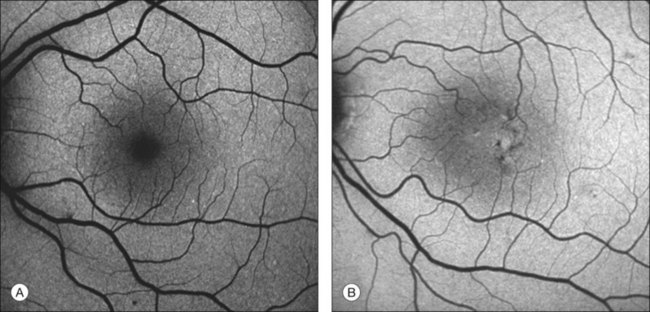
One of the earliest signs of mac tel type 2 is the loss of the hypofluorescent center seen normally on blue-light FAF due to the depletion of macular pigment in this condition (Fig. 55.9). Even in the absence of any fluorescein leakage or any other signs, especially in patients with asymmetrical mac tel type 2,10 this is diagnostic of the ocular condition. The area of retinal pigment hyperplasia will appear hypofluorescent on the FAF (Fig. 55.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree