Lost and Slipped Extraocular Muscles
Irene Ludwig
A lost extraocular muscle is defined as a muscle that has lost all direct or indirect connection to the sclera.1 It may be traumatic or iatrogenic. A slipped muscle lacks direct attachment between muscle tendon and sclera but is indirectly attached via loose (muscle capsule) or dense (lengthened scar) connective tissue.2,3,4 Slipped muscles are always iatrogenic, usually following prior strabismus surgery.
The repair of a lost or slipped muscle requires advanced diagnostic and surgical skill. Therefore, alternative procedures such as muscle transpositions, Faden procedures, and weakening of antagonist muscles often are used. However, with adequate preparation, direct repair is usually possible and produces a more functional result.
COMPLETE LOST MUSCLE
Mechanism
Iatrogenic
Most lost muscles occur during strabismus or retinal detachment surgery while the muscle is under traction. In some, the muscle ruptures at the musculotendinous junction due to connective tissue weakness.5,6 This has been termed the “pulled-in-two syndrome” and is usually seen in the elderly, but it has been described in younger patients with presumed collagen abnormality. The proximal portion of the muscle retracts posteriorly and becomes a lost muscle. In others, the suture pulls through the muscle tendon after muscle disinsertion,7 also leading to a lost muscle. It is also possible that some lost muscles may be created by nonattachment of tendon to sclera caused by long hang-back strabismus procedures.8 Once the suture dissolves, the muscle retracts posteriorly and becomes lost.
Traumatic
In blunt trauma, the muscle may avulse from its insertion, without losing its attachments to intermuscular septum. The torn end scars into surrounding orbital soft connective tissue (personal observation).10 Penetrating trauma may directly sever the muscle, with variable presentation, depending upon the location of the penetration.11,12
Diagnosis
As in all facets of medicine, the clinical history is crucial in diagnosis of lost muscles. Most commonly, the diagnosis of lost muscle is made immediately, as it is visualized intraoperatively. Large strabismus overcorrection occurring 2 to 4 weeks after large hang-back or adjustable suture surgery could indicate nonattachment to sclera and a lost muscle. If strabismus resulted from trauma, was the trauma blunt or penetrating? Where was the impact, and from what direction? Did loss of consciousness occur, and if so what was the time in coma? Was ptosis or enlarged pupil present? Was ecchymosis, periorbital edema, or proptosis present? Was onset of diplopia immediate or gradual after the injury? Diplopia following periorbital trauma with little or no evidence of head injury should increase one’s suspicion toward muscle injury rather than cranial nerve palsy.
Examination consists of complete sensorimotor evaluation, with particular attention to alignment measurement in all fields of gaze, versions, eyelid function, proptosis or enophthalmos, and pupils. Assessment of torsion is measured subjectively by double Maddox rod, and objectively by fundus exam. Clinical features include large angle consecutive strabismus, limited duction, and widening of the palpebral fissure, greatest with motility toward the direction of action of the lost muscle. Forced duction testing for muscle restriction and force generation testing of muscle strength are especially helpful and may be performed with topical anesthesia on adults in the office.
Ancillary testing include orbital computed tomography (CT) scans to rule out orbital fracture, and orbital magnetic resonance imaging (MRI) scans to view the extraocular muscles. Newer high-resolution MRI imaging utilizing orbital surface coils allow images of the extraocular muscles in multiple gaze positions. Published reports of this technique indicate detailed information about altered muscle and perimuscular anatomy and function.13 When high-resolution extraocular muscle imaging becomes more widely available, it will be a useful diagnostic tool in assessment of lost muscles.
Repair
Better than learning to treat a lost muscle is to prevent one from developing in the first place. Perimuscular tissue (capsule, intermuscular septum, orbital septae) will often support the muscle within the orbit and allow simple retrieval. During strabismus surgery, limit dissection of intermuscular septum, and place the suture well into tendon, with secure lock bites. Never cut tissue blindly. Directly visualize the muscle to avoid cutting the wrong muscle. Pull gently on the muscle hook to avoid pulling the muscle in two.
A strabismus or orbital surgeon should repair a lost muscle. Thorough understanding of extraocular muscle and orbital anatomy is essential, especially with regard to the connective tissue orbital septae. The lost muscle may still retain its intermuscular septal attachments to the oblique muscles. These can then be used to trace back to the lost rectus muscle. This applies to the inferior, superior, and lateral recti. As the medial rectus lacks these indirect attachments, it is the most difficult muscle to recover when lost. With the posteriorly retracted medial rectus, it is sometimes possible to follow the Tenon capsule posteriorly to the point where the muscle originally penetrated the Tenon in order to recover the lost muscle. In muscle avulsion following blunt trauma, the muscle is often found near the globe, adherent to orbital soft connective tissue. Preoperative MRI scan should alert the surgeon to this location and prevent unnecessary and destructive posterior dissection. The repair of the complete muscle avulsion is similar to the partial avulsion repair, which is described in detail below.
When a lost muscle is demonstrated to be posterior in location and not retrievable by tracing the attachments to intermuscular septum, it should be recoverable by the orbital approach. Goldberg describes approaching the lost medial rectus muscle via a transcaruncular incision, locating it adjacent to the periorbita in the extraconal space, retrieving it and directly or indirectly (hang-back) suturing it to the globe.14
Other techniques, which have been described, include a transnasal endoscopic approach to the lost muscle15 and the use of an electrical stimulator to locate the muscle.16 Locating the proximal stump of the lost muscle may be easier than the actual repair. In the elderly or debilitated patient who has suffered dehiscence at the musculotendinous junction, the torn tissue is usually friable and not strong enough to support sutures. Repair should then be directed at the surrounding muscle capsule.11 Suturing around the capsule of muscle and tendon has the dual advantage of allowing better suture support due to the connective tissue in the capsule and reducing the tension and vascular strangulation on the traumatized muscle tissue. This principle is utilized in orthopedic tendon repair.17 A lost muscle following sinus surgery may have a significant myectomized portion, preventing reanastomosis. The use of nonabsorbable sutures to bridge the gap has been described, combined with botulinum toxin injection into the antagonist muscle, with moderate success.9 Excessive dissection should be avoided, as disruption of orbital fat leads to adherence syndrome with limited motility.
If retrieval of the lost muscle is judged not to be possible, weakening of the antagonist muscle and transposition of adjacent muscles may restore alignment in the primary position. Both Hummelsheim1 and Jensen12 procedures have been advocated but are needed only rarely with meticulous approach to primary repair of the lost muscle (personal observation).14
PARTIAL LOST MUSCLE (PARTIAL AVULSION, FLAP TEAR)
Mechanism
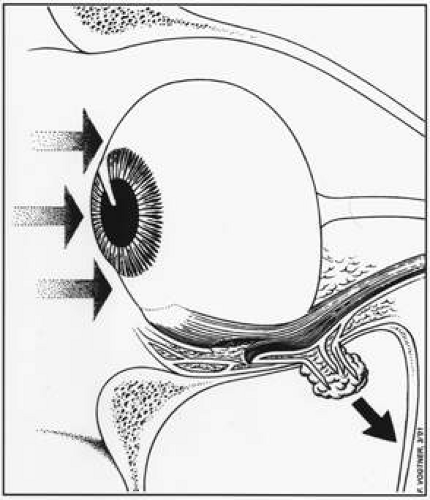
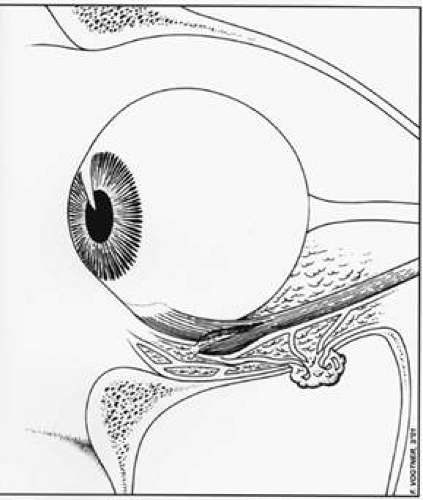
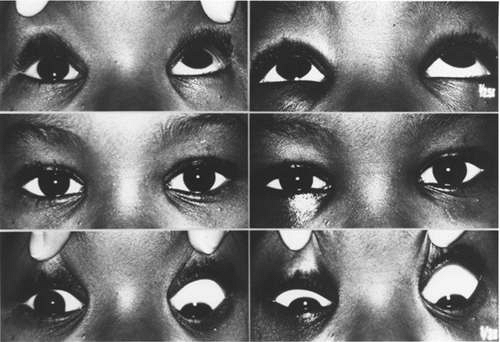
During blunt trauma, traction on the orbital septae by the bending or fracturing orbital wall may tear a portion of the extraocular muscle away from its insertion on the sclera. It is also possible to tear the external, or orbital layer, of muscle away from the internal, or global layer18,19 (Fig. 1). Demer has demonstrated the penetration by elastin fibers from the orbital septae into the orbital layer of the rectus muscle.20 This avulsed portion of muscle may then heal into surrounding orbital soft connective tissue, creating a motility disturbance (Fig. 2). The motility defect usually simulates muscle paresis, with decreased function into the field of action of the involved muscle, due to a tether effect created by the lost “flap” of avulsed muscle tissue (Fig. 3). Associated orbital fracture is common (Fig. 4) but not found in all cases. Either there is orbital bending without fracture, or more likely, a small hairline fracture that does not show on CT scan.
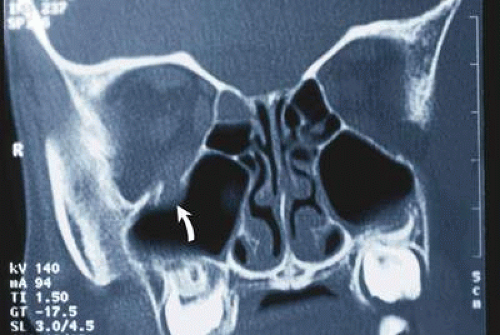 Fig. 4. Orbital CT scan of child in Figure 3, showing posterior orbital fracture with inferior rectus entrapment (arrow). (From Ludwig IH, Brown MS: Flap tear of rectus muscles. An underlying cause of strabismus after orbital trauma. Ophthalmic Plastic Reconstr Surg 18:443–450, 2002, with permission, and Ludwig IH, Brown MS: Strabismus due to flap tear of a rectus muscle. Trans Am Ophthalmol Soc 99:53-63, 2001, with permission.) |
Partial avulsions of rectus muscles have also been seen following retinal detachment surgery with encircling element and direct trauma to the muscle insertion.
The most commonly avulsed extraocular muscle is the inferior rectus (Fig. 5), followed by the medial rectus (Fig. 6). Partial avulsions of the superior recti are less common, and lateral rectus avulsions are rare. When medial rectus partial avulsions are present, the adjacent inferior or superior recti are often involved. The size of the avulsed flap may be very small, only involving a few fibers and capsule, or large, with only a small portion of muscle remaining attached to the globe.18,19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree