Fig. 16.1
Failure of autologous limbal transplantation with recurrence of corneal conjunctivalization (a). Contralateral donor eye with signs of a large previous limbal harvesting for limbal transplantation (white arrows) and the small biopsy for ex vivo expansion done after failure of the first graft (red arrow) (b). One year after successful cultivated limbal stem-cell transplantation with transparent, avascular, and stable epithelium (c). The same patient after penetrating keratoplasty combined with cataract extraction, lens implantation, and pupilloplasty (d)
Autologous Versus Allogeneic Limbal Grafts
In unilateral LSCD, or in bilateral LSCD, where a small portion of healthy limbus can be used as donor tissue for ex vivo expansion, autologous limbal grafts are advised [30, 32]. On the contrary, in total LSCD when the limbus is completely destroyed in both eyes, limbal tissue taken from a deceased donor or from a living relative can be used. In the literature, contrasting results have been reported on the use of allogeneic keratolimbal grafts, with an overall success rate of 73 % [1]. Both clinical successes and failures have been observed in the presence of systemic immunosuppressive therapy [6, 16, 23], while positive clinical results have been reported in the absence of immunosuppression [20, 33] and/or in the absence of allogeneic cell survival [2, 14]. In most cases, however, the interpretation of results has been hampered, either by the lack of a proper genetic evaluation of the presumptive long-term engraftment of allogeneic limbal grafts or by the inadequate length of follow-up. In the absence of demonstrated surviving donor cells, a possible explanation for clinical success is that patients with non-total limbal stem-cell deficiency have been included, and the grafted allogeneic limbal cells might have induced modification of the microenvironment and promoted proliferation of the patient’s own dormant stem cells, whose progeny gradually replaces donor cells. While remaining in situ in the injured eye, these limbal cells are evidently unable to generate corneal epithelium, either because of the lack of a suitable microenvironment for multiplication or because of fibrotic obstruction to their migration over the cornea. This would explain the mixed population of donor and recipient corneal cells observed at short-term follow-up. These findings are consistent with reports showing that clinical improvement observed following allogeneic keratolimbal grafts does not necessarily correlate with the long-term survival of donor cells [2, 14]. Similarly, cultured allogeneic epidermal keratinocytes do not engraft permanently, but provoke epidermal regeneration in partial-thickness skin burns, presumably by stimulating residual hair follicle stem cells [3].
Indications and Contraindications
Limbal stem-cell grafting is indicated to treat limbal stem-cell deficiency (LSCD) [8, 36]. As said above, LSCD includes heterogeneous diseases where the limbus has been damaged. The eyelids, conjunctiva, corneal stroma, nerves and endothelium, and immune and lacrimal systems can also be involved. Scrupulous step-by-step reconstruction should be planned, treating the structures involved separately, to prepare the best recipient bed for the cultivated cells. Eyelid malposition and malocclusion should first be treated. Conjunctival symblepharon should be then addressed using the appropriate procedures. Once the eyelids and conjunctiva have been treated, tear film and inflammation should be carefully evaluated. The minimum of tear film and the maximum inflammation allowing the successful long-term survival of the grafted stem cells are not clear. In our previous clinical trials [31, 32], we excluded patients with Schirmer’s test below 5 mm/5 min, but this was arbitrarily chosen, and one might suggest that the quality of tears might be even more important than the quantity. Unfortunately, at present there is still no valid method for its assessment. We do not include in our clinical protocol for limbal transplantation patients showing severe active inflammation. As for tear film, we are still far from having reproducible clinical assessment and inflammation grading, with the exception of redness scoring.
Diagnosis of LSCD
LSCD diagnosis is based on the evidence of a previous insult (cause) and peculiar clinical features (signs) and is eventually confirmed by instrumental tests [8, 36]. The causes of LSCD are shown in Table 16.1.
Table 16.1
Causes of LSCD
Congenital | Acquired |
|---|---|
Aniridia | Chemical/thermal injuries |
Dyskeratosis congenita | Radiation |
Autoimmune polyglandular syndrome | Contact lens abuse |
Ectrodactyly ectodermal | Drug induced |
Dysplasia-clefting syndrome | Extensive limbal surgery |
Endocrine deficiency | Extensive corneolimbal infections |
Xeroderma pigmentosum | Stevens-Johnson syndrome |
Mucous membrane pemphigoid | |
Atopic keratoconjunctivitis | |
Graft vs. host disease |
Clinical Features
Symptoms
The acute phase is characterized by pain, photophobia, and blurred vision with severity based on the extension of the damage. The chronic phase presents with milder photophobia, foreign body sensation, and pain in the presence of recurrent epithelial erosion. Varying visual acuity decrease depends on the extension of the damage. However, when the visual axis is not involved, there is no reason to propose surgical treatment. Conservative treatment for symptom relief, such as preservative-free artificial tears, autologous serum eyedrops, therapeutic soft or scleral contact lenses, and short courses of low-dose topical steroids, is therefore indicated.
Signs
Corneal signs can be, depending on the severity of the damage, the loss of normal limbal anatomy with disappearance of the palisades of Vogt, irregular epithelium with fluorescein uptake, recurrent or persistent epithelial defects, superficial neovascularization (“conjunctivalization”) and/or fibrovascular pannus formation, deep stromal neovascularization, and chronic inflammation (Figs. 16.1a and 16.3a) [8, 36].
Supplementary Tests
Impression Cytology
Cytokeratins (CKs) are intermediate filaments present in almost all epithelial cells [11]. Epithelia from different parts of the body express keratins, which are unique for each location: this specificity can be thus used to differentiate genotypically different cell types [24]. The cornea expresses the cytokeratins K3 and K12, but not K19, while the conjunctiva specifically expresses K19, but not K3 and K12 [10, 35].
We previously showed that immunocytochemistry carried out on corneal impression cytology specimens allows us to distinguish between corneal and conjunctival epithelial cells with positive/negative staining of K3/K12 (cornea) and K19 (conjunctiva) [7]. We also showed that impression cytology can be used to grade limbal stem-cell deficiency and assess the final results after limbal stem-cell grafting [31] However, it is an invasive procedure that, despite its simplicity, may cause painful epithelial defects that might be difficult to treat due to the underlying limbal problem. Therefore, impression cytology should only be implemented in those cases where there is a specific question needing to be answered.
Confocal Microscopy
Confocal microscopy is a noninvasive procedure that can distinguish between corneal and conjunctival epithelial cells and is therefore useful in the diagnosis of limbal stem-cell deficiency (Fig. 16.2) [9, 21, 37]. In a recent study by Nubile et al., confocal microscopy was compared with impression cytology in patients with limbal disorders with concordance in 90 % of cases [25]. Confocal microscopy is therefore a useful noninvasive method to confirm limbal stem-cell deficiency. We should remember, however, that confocal microscopy evaluates cell morphology but cannot recognize their true phenotype: without specific markers we might mistake transient morphological changes of corneal epithelial cells for conjunctival cells.
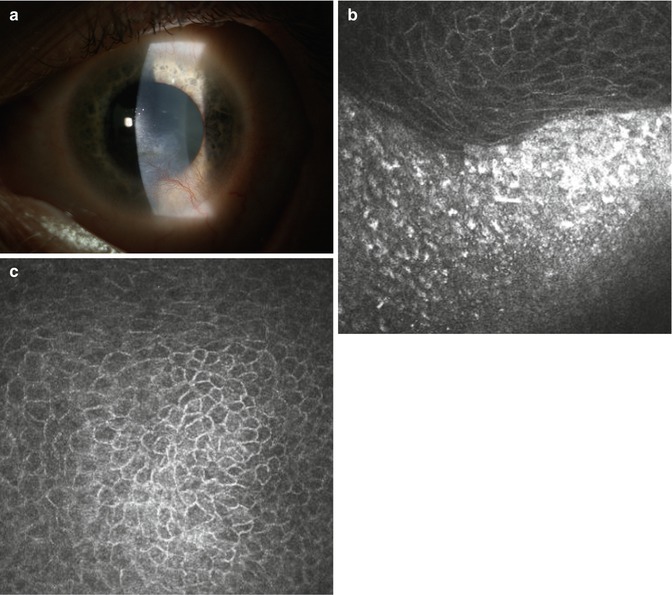
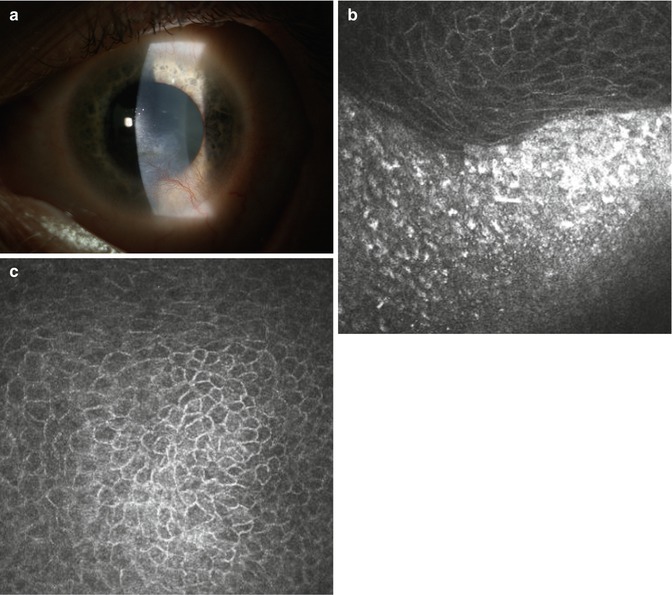
Fig. 16.2
Cornea with partial limbal stem-cell deficiency (a). Although in some cases the detection of conjunctival pannus is obvious with confocal microscopy (b), in some other cases the presence of conjunctival epithelium may be proposed, but not so obvious (c). In these cases, further confirmation with clinical findings and/or standard impression cytology techniques with staining for specific markers may clarify the diagnosis
Procedure
Various protocols for the cultivation of limbal stem cells for transplantation have been proposed and recently reviewed by Shortt et al. and Joe and Yeung, including methods to extract cells from the biopsy (mechanical disruption or enzymatic dissociation), substrates and carriers (fibrin sheet, amniotic membrane, polymers, contact lenses, collagen), or mediums with animal-derived components or xeno-free [18, 36]. Although good clinical outcomes have been reported with all of these different culture procedures, few studies have evaluated the clonal characteristics of the cultivated cells and their proliferative potential. When dealing with stem-cell-based therapies for diseases involving cell-renewing tissue, it should be mandatory to demonstrate the presence, survival, and concentration of stem cells in culture and in the graft and validate the procedure under GMP conditions [4, 28].
We previously showed, analyzing the proliferative potential and cloning characteristics, that corneal stem cells are segregated in the limbus, while conjunctival stem cells are uniformly distributed in the bulbar and forniceal conjunctiva. Moreover, conjunctival epithelial cells and goblet cells derive from a common bipotent progenitor [26]. We also showed that autologous limbal stem cells, cultivated on fibrin and 3 T3 feeder layer, maintain their properties and are able to restore corneal integrity in severe limbal stem-cell deficiency [31]. We later confirmed the long-term stability of the results, up to 10 years, and validated the procedure, comparing clinical results with the level of expression of ΔNp63α in culture [5, 29, 32]. Clinical success was statistically associated with the percentage of p63-positive cells in culture. Cultures in which p63-bright cells made up more than 3 % were associated with successful transplantation rate close to 80 %. In contrast, cultures with less than 3 % were associated with poor results, with successful transplantation in only 10 % of patients. On the basis of these data, only cultures that contain more than 3 % ΔNp63α cells are now grafted on patients.
We hereafter report our protocol: (i) biopsy, (ii) stem-cell expansion in culture, (iii) grafting, and (iv) postoperative management.
Biopsy
A 1–2 mm2 wide, approximately 100 μm deep, limbal biopsy is taken from the contralateral eye (Fig. 16.1b) or from an unaffected portion of the limbus in partial bilateral cases. The procedure can be carried out under topical anesthesia with oxybuprocaine or para/retrobulbar anesthesia with Carbocaine or Marcaine without adrenaline depending on patient collaboration. The use of topical lidocaine should be avoided due to its toxicity. Limbal tissue is normally harvested in the superior quadrant. Meyer-Blazejewska et al. found that stem-cell isolation is highest when using biopsies from the superior limbus and also that harvesting in the superior quadrant keeps it less exposed [22], although harvesting can be carried out from any quadrant if necessary. We previously showed that there are no differences in the efficacy of stem-cell isolation and growth comparing different areas of the limbus [26]. The biopsy specimen is then inserted into a sterile tube containing the transport medium and immediately sent to the laboratory where it will be processed within 24 h. Sutures are not required, but we use two 10/0 nylon stitches to bring the conjunctiva over the area of the corneal biopsy to reduce risks and symptoms. Bandaging is generally not required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


